Transposition of the great arteries is a prevalent congenital heart defect with a high survival rate and a good long-term outcome, especially if managed with early surgical intervention during the neonatal period. In this study, our main objective was to describe patient characteristics and outcomes and to identify possible predictors of early and long-term morbidity and mortality.
MethodsRetrospective analysis through review of clinical and surgical charts of patients with transposition of the great arteries admitted to the service of neonatology during 2000-2011.
ResultsThe study included 136 patients; 119 of them had undergone corrective surgery during the neonatal period. Patients were divided into 3 groups: group I, 81 cases of isolated transposition; group II, 24 cases with ventricular septal defect; and group III, 31 with “complex” transposition of the great arteries. The overall postoperative survival was 96.7% (115 of 119 patients); no patients from group I died after surgery. Duration of surgery, intubation, inotropic treatment, and length of stay were higher in patients in groups II and III. The overall survival rate after an average of 6 years of follow-up was 90.4% 123 of 136 patients, with no deaths after discharge in group I. The most frequent residual defect during cardiac follow-up was supravalvular pulmonary stenosis, in 33 of 113 patients that had follow-up data.
ConclusionsIn our study, the survival rate was high in patients with transposition of great arteries and especially in those undergoing arterial switch. The number of subsequent residual heart defects was low.
Keywords
Congenital heart defects are the most common major congenital malformations. They are an important cause of morbidity and mortality in the neonatal period, occurring in 4-10/1000 live births.1
In the last three decades, there has been increased survival in these patients, mainly due to advances in diagnostic fetal and neonatal echocardiography, the extensive use of prostaglandin E1, and technological progress in cardiac surgery units.2
Unrepaired critical heart defects can result in progressive and irreversible secondary damage to various organs. Reconstructive surgery in this period can reduce mortality and prevent secondary damage.3
Transposition of the great arteries (TGA) accounts for 5% to 7% of congenital heart disease. In recent decades, TGA has been studied with more precision. Van Praagh et al.4 have clarified the underlying anatomy and include TGA in conotruncal heart defects that include malposition of the great arteries. Double outlet right ventricle (DORV), double outlet left ventricle, and anatomically corrected transposition are also included in this group.4
About half of the patients with TGA have no other cardiac malformations, and are designated as isolated TGA.4–6 The remaining cases are designated as complex TGA, that is, TGA accompanied by other malformations.
The main treatment for isolated TGA is surgical correction during the neonatal period.7 Several surgical techniques are available, but the technique of choice is the arterial switch (AS) operation, described by Jatene et al. in 1975.8 High survival rates have been reported, with few medium- or long-term sequelae.9–11 The aims of this study were:
- •
To determine the outcome of neonates with TGA who underwent AS during the study period.
- •
To describe differences in the outcome of neonates with isolated TGA, transposition with ventricular septal defect (VSD), or complex transposition accompanied by other malformations who underwent AS.
- •
To determine the prognostic factors of morbidity and mortality in neonates who underwent a simple AS procedure or AS combined with another surgical procedure.
- •
To determine the long-term cardiac outcome of patients with TGA.
This retrospective study consecutively included all patients admitted to the service of neonatology with a diagnosis of TGA. The study period was from April 2000 to December 2011. During this period, 7935 patients were admitted to the service of neonatology. Of these patients, 781 (10.3%) were diagnosed with congenital heart disease, including 136 (17.4%) with isolated or complex TGA; 59 (43.6%) of these were intrahospital transfers (from the maternity unit) and 77 (56.6%) were referred from other centers.
Mean birth weight was 3227 (506) g and mean gestational age was 39 (1.7) weeks; 102 (75%) were boys and 34 (25%) were girls.
Patients and Study GroupsThe patients were divided into 3 groups according to echocardiographic findings: group I, 81 neonates with isolated TGA (59%); group II, 24 neonates with TGA and VSD (18%), and group III, 31 neonates with “complex” TGA treatable by AS. The latter group consisted of 12 patients with DORV and transposed arteries, 11 patients with aortic coarctation and/or hypoplastic aortic arch, and 8 patients with pulmonary stenosis and VSD (23%).
Echocardiographic StudyIn all cases, congenital heart defects were identified using 2-dimensional color Doppler echocardiography. The heart defects were classified according to the recommendations of the International Nomenclature and Database Conference for Pediatric Cardiac Surgery.12 In patients with more than one heart defect, the defect with the greatest hemodynamic effect was chosen.
Initial Management of PatientsFollowing hospital protocol, pregnant women with a diagnosis of fetal congenital heart disease were referred to prenatal monitoring and early neonatal management. After birth, central venous cannulation was immediately performed for the administration of prostaglandin E1. Within the first 24h of life, a Rashkind balloon atrial septostomy procedure was performed in patients with isolated TGA and restrictive foramen ovale. Corrective surgery was scheduled in the first weeks of life.
Surgical TechniqueCorrective surgery was performed with extracorporeal circulation (ECC) and hypothermia according to the AS technique described by Jatene et al.8 If present, VSD was corrected using a heterologous pericardium patch during the same procedure. Patients with DORV and TGA were treated by AS and VSD closure whenever it was possible to maintain continuity between the ventricles and the great arteries. Aortic coarctation was corrected by coarctectomy with end-to-end anastomosis extending to the inferior aspect of the aortic arch.
An atrial switch (Senning procedure) was performed when needed, rerouting deoxygenated vena caval blood to the pulmonary artery and oxygenated blood to the aorta. The coronary artery pattern at the time of surgery was described according to the Leiden classification.13
Early Postoperative TreatmentFollowing surgery, the patients were readmitted to the service of neonatology, where they were treated according to standard guidelines. After the AS procedure, inotropic infusion was begun with milrinone and dopamine, adjusting doses according to clinical response. All patients received analgesia with fentanyl and mechanical ventilation. Extubation was scheduled within 24 to 48 h, providing there were no respiratory complications (pulmonary edema, atelectasis, pneumonia).
Postdischarge Follow-upFollow-up was scheduled in outpatient cardiology clinics. The first visit was 1 month after hospital discharge and then every 6 months providing there were no complications. Each visit included medical history, physical examination, electrocardiogram and echocardiogram to identify potential complications, in which case further tests were performed as appropriate.
Statistical AnalysisDiscrete variables are presented as numbers and percentages and continuous variables as mean (standard deviation) for normal distributions and as median (range) for non-normal distributions. The chi-square test or Fisher exact test were used to compare discrete variables and the Student t test or Mann-Whitney U test to compare continuous variables associated with dependent variables (dichotomous). Analysis of variance was used to compare continuous variables in different groups. Data were analyzed using the SPSS 19.0 software package for Windows.
RESULTSGeneral SampleOf the 136 newborn patients included in the study, 49 (36%)–44 (74.5%) of the 59 inpatients and 5 (6.5%) of the 77 referred patients–had a prenatal diagnosis of TGA.
Most patients without a prenatal diagnosis of heart disease presented symptoms in the first 24 h of life (75 of 87 [86%]).
Cyanosis was the most frequent clinical sign, either alone (27 cases [31%]) or with murmur (25 cases [28.7%]).
Initial ManagementIntravenous prostaglandin was administered to 125 patients (92%). A Rashkind balloon atrial septostomy procedure was performed in 108 patients (79.4%) at an average of 34 h of life.
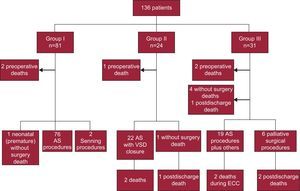
Surgical Treatment According to Study GroupThe Figure shows the surgical treatment of patients according to study group. Of the 81 patients in group I, 1 patient was very premature and did not undergo surgery in the neonatal period, 2 underwent Senning procedure, and 76 underwent AS; 2 died before surgery. Of the 24 patients in group II, 1 patient died before surgery and 1 was discharged without neonatal corrective surgery because of unfavorable anatomy. AS with VSD closure was performed in 22 (91.6%) patients. Of the 31 patients in group III, 10 were not candidates for AS because of unfavorable anatomy and 2 died before surgery. However, corrective surgery was performed in 19 patients: 10 of 12 patients with DORV and TGA, 7 of 11 patients with aortic coarctation and/or hypoplastic aortic arch, and 2 of 8 patients with pulmonary stenosis and VSD.
Thus, during the study period, neonatal corrective surgery was performed in 119 patients (87.5%), AS in 117 patients, and Senning procedure in 2. At the time of surgery, mean age was 14 (9.4) days and mean weight was 3336 (430) g.
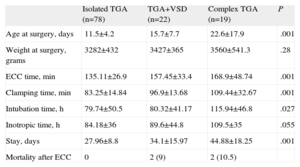
Patients with isolated TGA underwent surgery at a mean age of 11.5 (0.4) days, whereas patients in the other 2 groups underwent surgery at a mean age of 19.6 (14) days. These differences were statistically significant (Table 1).
Surgical and Postoperative Variables
| Isolated TGA (n=78) | TGA+VSD (n=22) | Complex TGA (n=19) | P | |
| Age at surgery, days | 11.5±4.2 | 15.7±7.7 | 22.6±17.9 | .001 |
| Weight at surgery, grams | 3282±432 | 3427±365 | 3560±541.3 | .28 |
| ECC time, min | 135.11±26.9 | 157.45±33.4 | 168.9±48.74 | .001 |
| Clamping time, min | 83.25±14.84 | 96.9±13.68 | 109.44±32.67 | .001 |
| Intubation time, h | 79.74±50.5 | 80.32±41.17 | 115.94±46.8 | .027 |
| Inotropic time, h | 84.18±36 | 89.6±44.8 | 109.5±35 | .055 |
| Stay, days | 27.96±8.8 | 34.1±15.97 | 44.88±18.25 | .001 |
| Mortality after ECC | 0 | 2 (9) | 2 (10.5) |
ECC, extracorporeal circulation; TGA, transposition of the great arteries; VSD, ventricular septal defect.
Data are expressed as mean±standard deviation or no. (%).
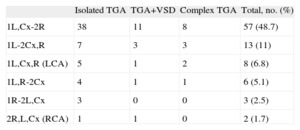
Mean ECC time was 144 (34) min and mean aortic cross-clamping time was 90 (20) min in the 117 patients who underwent AS. When comparing intraoperative and postoperative variables according to diagnostic group, significant differences were observed in ECC time, cross-clamping time, postoperative intubation time, and postoperative inotropic infusion time (Table 1). Coronary patterns are shown in Table 2. Delayed sternal closure was performed in 4 of 117 patients (3%).
Coronary Artery Patterns
| Isolated TGA | TGA+VSD | Complex TGA | Total, no. (%) | |
| 1L,Cx-2R | 38 | 11 | 8 | 57 (48.7) |
| 1L-2Cx,R | 7 | 3 | 3 | 13 (11) |
| 1L,Cx,R (LCA) | 5 | 1 | 2 | 8 (6.8) |
| 1L,R-2Cx | 4 | 1 | 1 | 6 (5.1) |
| 1R-2L,Cx | 3 | 0 | 0 | 3 (2.5) |
| 2R,L,Cx (RCA) | 1 | 1 | 0 | 2 (1.7) |
Cx, circumflex; L, left coronary artery; LCA, left coronary artery only; R, right coronary artery; RCA, right coronary artery only; TGA: transposition of the great arteries; VSD, ventricular septal defect.
Mean hospital stay was 32 (13) days in patients who underwent AS. Significant differences were found in hospital stay between groups, with shorter stays in patients with isolated TGA (Table 1).
MortalityThere were 5 preoperative deaths (2 in group I, 1 in group II, and 2 in group III). The causes were: refractory cardiogenic shock, necrotizing enterocolitis in the very premature patient, cardiac tamponade after catheterization, cardiorespiratory arrest during catheterization, and associated Charge syndrome. Cardiogenic shock and cardiac tamponade were not prenatally diagnosed in the 2 patients with these conditions.
There were 3 intraoperative deaths (2.5%) (Table 1). Of these, 2 patients had DORV and TGA. The other patient (group II) underwent urgent surgery for hemodynamic failure in the context of sepsis. Although AS was performed, the patient died during the procedure.
There was 1 early postoperative death. This patient had TGA and VSD (group II) and died after requiring support with extracorporeal membrane oxygenation due to multiorgan failure secondary to Candida sepsis after surgery.
In summary, there were 4 (3.4%) post-AS early deaths (less than 30 days after surgery). There were 4 late deaths (after discharge). Of these, 3 patients had complex heart disease and 1 patient had TGA and a large VSD. None of these patients were considered candidates for neonatal corrective surgery.
None of the patients who had undergone AS died during postdischarge follow-up.
Due to the low post-AS mortality rate, no statistically significant results could be obtained related to the operative variables or prenatal diagnosis.
MorbidityLaboratory tests suggested infection in 22 of 117 patients [18.8%]. Sepsis was confirmed by positive blood culture (12 of 117 [10.2%]) and urinary tract infection by positive urine culture (4 of 117 [3.4%]). Arrhythmias occurred in 22 patients during the immediate postoperative period. Two patients required pacemaker implantation and 6 needed medical treatment; the arrhythmia resolved spontaneously in the remaining patients. The most common pulmonary complication was pulmonary edema, with or without pleural effusion (20 cases [17%]). There were 9 cases of diaphragmatic paralysis.
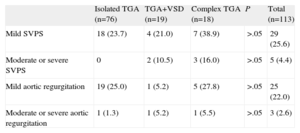
Cardiac Follow-upCardiac follow-up data were available for 113 patients who underwent surgery between 2000 and 2011. The duration of the follow-up period was between 1 year and 12 years (mean, 6 years). The most common residual defect (Table 3) was supravalvular pulmonary stenosis (34 of 113 [30%]). This was documented as mild in 29 patients; moderate in 1 patient (angioplasty of the pulmonary valve was needed), and severe in 4 patients (angioplasty was needed in 2 patients and a pericardial patch was used to widen the right ventricular outflow tract in the other 2 patients). The second most common residual defect was aortic valve regurgitation (28 patients [20.5%]), which was mild in 25 patients and moderate in 3 patients. No patient needed reintervention.
Residual Lesions After Arterial Switch (n=113)
| Isolated TGA (n=76) | TGA+VSD (n=19) | Complex TGA (n=18) | P | Total (n=113) | |
| Mild SVPS | 18 (23.7) | 4 (21.0) | 7 (38.9) | >.05 | 29 (25.6) |
| Moderate or severe SVPS | 0 | 2 (10.5) | 3 (16.0) | >.05 | 5 (4.4) |
| Mild aortic regurgitation | 19 (25.0) | 1 (5.2) | 5 (27.8) | >.05 | 25 (22.0) |
| Moderate or severe aortic regurgitation | 1 (1.3) | 1 (5.2) | 1 (5.5) | >.05 | 3 (2.6) |
SVPS, supravalvular pulmonary stenosis; TGA, transposition of the great arteries; VSD, ventricular septal defect.
Data are expressed as no. (%).
During the follow-up period, 2 patients with TGA and aortic coarctation needed catheterization and angioplasty after presenting with recoarctation. The new patch was needed in one of the patients with TGA and a large VSD.
The presence of residual lesions in patients with complex TGA was not statistically more common than in other patients.
DISCUSSIONIn this Spanish series, the percentage of patients with a prenatal diagnosis of TGA was similar to the 38% reported by other authors, such as Strauss et al.3 The higher percentage of internal neonatal patients in our hospital was due to the transfer of pregnant women from other centers to our tertiary-level hospital because of suspected fetal congenital heart disease.
There were no differences between patients who underwent prenatal diagnosis and those who did not; this may be due to the low mortality rate observed and improvements in neonatal transport. However, the 2 patients with isolated TGA who died did not have a prenatal diagnosis; their outcome may have improved if this had been the case.
The initial management of patients in our series was similar to that in the series reported by Hraska et al.,14 in which 88% of patients received prostaglandin E1 and 88% underwent atrial septostomy.
The study groups were similar to those reported by Prifti et al.,15 Swartz et al.,16 Fricke et al.,17 and Hraska et al.14; in general, these studies compared the outcomes of patients who underwent AS, dividing patients into groups: sometimes comparing isolated TGA with TGA plus VSD, or further separating out TGA with aortic coarctation/hypoplastic aortic arch or DORV. The number of patients with isolated TGA in these groups ranged from 66% to 74% of the total, somewhat higher than was observed in our series (59%). The number of patients with TGA and VSD ranged from 26% to 29% (18% in our series) and of those with complex TGA from 6% to 16% (23% in our series). The percentages in each series may have varied according to which patients were accepted or rejected for AS in each center; in our series, a slightly higher percentage of patients had complex TGA.
The most common coronary pattern was 1L,C-2R, although the percentage was somewhat lower than in other studies.7,12,18–22 Some studies have suggested an association between an abnormal pattern (such as intramural coronary arteries or single coronary artery) and increased surgical risk,18,20,21,23 but more recent studies,9,12,22,24 including ours, have not found a significant association. Long-term mortality could be influenced by this complication, although in our study there were no deaths related to coronary obstruction during 12 years of follow-up.
Kempny et al.25 reported outcomes in a series of adult patients who underwent previous AS. After analyzing the variables associated with poor prognosis (defined by the composite endpoint of death or reintervention in adulthood), the authors found that uncommon coronary patterns (other than type A) were associated with an increased risk of poor outcome.
Regarding surgical variables, Prifti et al.15 reported ECC times of 135min for isolated TGA and 154 min for TGA and VSD or other malformations; Fricke et al.17 reported 156 min and 180 min, respectively. These times were similar to or slightly higher than those in our study. However, the series described by Fricke et al.17 included a large number of patients (618) over a very long period (1983-2009), which could have led to different outcomes at each stage, as the authors themselves pointed out. In the series described by Prifti et al.,15 the average aortic cross-clamping time was 90 min for isolated TGA and 117 min for TGA and VSD and for complex TGA; Fricke et al.17 reported average times of 80 min and 103 min, respectively. These times were also similar to ours (Table 1). The increased difficulty in achieving clinical stability in preparation for surgery may have been because patients with TGA and other defects were older at the time of the AS procedure. Similar data have been reported in other series.15,17
Postdischarge mortality is an uncommon event,14–17,26 whereas there is a greater risk of inhospital mortality. The overall mortality rate after AS (6.8%) observed in our study was similar to the rates (0.8% to 9%) recently reported in the literature.7,9,11,12,18,27
The most recently published series of patients undergoing TGA in Spain was reported by Garcia-Hernandez et al.19 They presented the outcomes of patients with epidemiological data similar to ours: 121 patients treated over a period of almost 15 years; 80 patients with isolated TGA and 41 patients with TGA and VSD. Procedural time (ECC, aortic clamping) and mechanical ventilation time were somewhat higher than in our patients. In this interesting article, the authors stated that ECC times greater than 150 min were associated with increased mortality due to multiorgan failure after ECC.19,24 Another factor associated with poor outcomes was delayed sternal closure, which was performed in the operating room in 38 patients (31.4%) in their series. The authors reported that the mortality rate among patients with TGA and VSD was 0%, but VSD was corrected in only a quarter of the patients during the same procedure. The progressive decrease in mortality to about 2% in their hospital over the last 5 years is noteworthy.
The most common residual cardiac lesions in AS patients reported in the literature are supravalvular pulmonary stenosis, aortic regurgitation, and coronary obstruction.10,20–22,24
Supravalvular pulmonary stenosis is inherent to the surgical procedure itself. Brown et al.20 reported an incidence of 6%, whereas De Koning et al.10 reported 56% at 10-year follow-up, and Kempny et al.25 reported 57.6% in patients followed up into adulthood. De Koning et al.10 described a reintervention rate of 30%; the majority of these reinterventions were performed during childhood. It is the most common cause of reintervention in patients with TGA.
Approximately one-third of AS patients had aortic regurgitation during follow-up. This is the second most common residual defect, although it is documented as mild in the majority of patients. Its incidence ranges from 4% to 60%,10,20,24,25 although the percentage of severe cases that could require reintervention is null.10,20–22,24,25
De Koning et al.10 suggest that up to 70% can present dilation of the aortic root and Haas et al.21 describe a progressive increase in aortic regurgitation during follow-up.
Myocardial ischemia is considered to be a complication that should be taken into account during patient follow-up,11,28 as it can require reintervention or be the cause of long-term mortality. In the present series, myocardial ischemia did not occur in any of the patients.
Although the residual defects observed in our study are of little clinical relevance, we suggest that some complications could occur or worsen over time during long follow-up periods. Thus, adequate cardiac monitoring is essential.
Study LimitationsThis study describes the cardiological outcomes of corrective surgery for TGA in neonates at a single hospital. As the study period covered 11 years, it is possible that the overall treatment of patients has not been completely uniform over time.
Another limitation concerns the long-term outcome of the patients with TGA; follow-up could not be fully completed and some patients were lost to follow-up.
CONCLUSIONSOutcomes in the neonatal patients with TGA who underwent AS have been satisfactory in terms of survival rates, reintervention, or the occurrence of major complications during follow-up.
During the neonatal period, corrective surgery was needed in only two-thirds of the patients with TGA accompanied by malformations such as aortic coarctation, pulmonary stenosis or DORV.
There were differences in procedural time, need for medical treatment, and length of hospital stay in these patients according to whether they had isolated TGA, TGA with VSD, or complex TGA. Having TGA with VSD or another accompanying defect increases the risk of inhospital death; no patient with isolated TGA in our series died during the study period.
Regarding long-term outcomes, supravalvular pulmonary stenosis is the most common residual defect in neonatal patients with TGA who have undergone AS.
CONFLICTS OF INTERESTNone declared.