To the Editor:
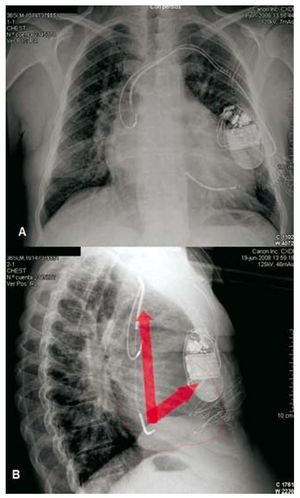
A male patient aged 35 years with d-transposition of the great arteries (dTGA), situs solitus, levocardia, left-facing apex, and intact septums was admitted due to ventricular fibrillation-induced cardiac arrest and was successfully reanimated. Seventy-two hours after his birth he had undergone balloon septostomy, and at the age of 4 years, a Mustard procedure. His NYHA functional class was II, and his systemic right ventricle (sRV) ejection fraction was 40%. Some days before his admission, an atrial flutter was detected with a ventricular frequency of 100 systoles/min. The echocardiogram and the MRI showed a dilated RV, severe tricuspid insufficiency and a dilated pulmonary artery. No alterations were detected in the atrial redirection baffles, the pulmonary left ventricle (pLV) or the left valves. We implanted an ICD (ConfientTM, Boston Scientific, St. Paul, Minnesota, U.S.A.) via the left subclavian vein, directing the defibrillation electrode to the LV through the atrial baffle. The atrial electrode was implanted in the right atrial roof. To guarantee effective defibrillation, we used a high-energy generator (maximum shock 41 J) located in the left submammary position in order to obtain a defibrillation vector covering the most ventricular mass (Figure 1). We practiced an effective defibrillation test for a shock of 23 J. No complications occurred at discharge from hospital.
Figure 1. Posteroanterior (A) and lateral (B) radiographies. The arrows sketch out the depolarisation vectors. Note the left subpectoral generator and the posterior distal coil located in the left (pulmonary) ventricle.
The Mustard correction procedure has successfully increased the survival of dGTA patients by 91% at 20 years, and most have a good functional class.1 However, there is a 6.4% incidence rate of sudden death (SD) in long-term follow up, which makes up 40% of total mortality.1 SRV dysfunction (32% after 18 years of follow-up) and the appearance of supraventricular tachyarrhythmias (14% and 21.5% at 11.5 and 23.4 years of follow-up, respectively) have been identified as predictive factors for SD.1-3 The ICD has become an increasingly widespread treatment for patients with surgically repaired congenital heart conditions and whose risk of sudden death is 25 to 100 times higher than that of the general population.4 Its feasibility has recently been documented for dTGA patients who have undergone a Mustard procedure.5,6 Implanting the device in these patients can be complicated due to inherent anatomical anomalies and such surgical sequelae as baffle stenosis, which must be ruled out before undertaking the procedure. One of the factors determining the device's effectiveness is the configuration of the defibrillation vector with respect to the heart chambers. This will depend on the arrangement of the coils and the generator body when it is active.7 To bring the case against the distal coil, which is posterior in this case due to its location at the LV, the generator should be in a lower position than usual, in the left submammary area.6 The use of high-energy devices is recommendable for increasing the defibrillator's probability of success.6 A dual-chamber ICD is also recommendable, due to the frequent development of sinus dysfunction1 and supraventricular tachyarrhythmias3 that cause inappropriate shocks.