Keywords
INTRODUCTION
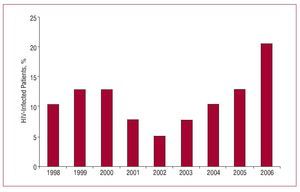
Infection due to the human immunodeficiency virus (HIV) has become a universal public health problem. According to recently published epidemiologic data from the World Health Organization, it is estimated that more than 40 million individuals currently live with HIV infection, and more than 4.3 million new cases of infection occurred in 2006. In the USA alone, between 850 000 and 950 000 individuals have HIV infection, including more than 200 000 who are unaware that they are infected by the virus.1 Recent reports on the evolution of HIV have observed a decrease in the incidence of the virus in Western countries. In all probability, this decline is secondary to the sustained inhibition of viral replication resulting from the introduction of highly active antiretroviral therapy (HAART) and protease inhibitors (PIs).2 Although the new antiretroviral therapies are not free from adverse reactions, they have changed the natural history of the disease and led to greater survival among patients with acquired immunodeficiency syndrome (AIDS) and those with HIV infection.3 Thus, the infection has come to be considered a chronic disease, in which patients are exposed to the same cardiovascular risk factors affecting the general population. This chronic nature of the disease, together with the effects of antiretroviral drugs on the patients' metabolism, has resulted in an increase in the number of HIV patients referred for cardiac surgery (Figure 1).
Figure 1. Stratification of the number of surgical procedures per year performed in HIV-infected patients, expressed as percentage of the total sample (data from our department).
To date, surgical morbidity and mortality rates in HIV patients undergoing cardiovascular procedures remain unknown. Furthermore, the scarcity of publications in the related literature and the limited number of patients enrolled in the few available studies have made it difficult to derive definitive conclusions regarding the perioperative management of this particular patient population. In this study we describe our experience with HIV-infected patients undergoing cardiac surgery in our hospital, with particular emphasis on the outcome of surgery and the results for long-term survival.
METHODS
A retrospective study including 7174 patients who underwent cardiovascular surgery at The Mount Sinai Medical Center was conducted between January 1998 and December 2006. A computerized registry, audited and validated by the New York State Department of Health (NYSDH), was used to identify the patients. The NYSDH prospectively compiles a mandatory operative report that includes all the demographic and cardiovascular variables for each patient undergoing cardiac surgery at our hospital. One of the preoperative variables recorded is the patient's immunodeficiency status (223/7174; 3.1%). Thus, the clinical records of each patient were meticulously reviewed to identify those with immunodeficiency due to HIV infection and obtain additional information for the study. The diagnosis was established based on a serological profile consistent with HIV infection (prior negative ELISA, followed by positive ELISA, or positive baseline ELISA with inconclusive Western blot findings, followed by positive Western blot). A total of 39 HIV-infected patients comprised the study population.
The patients'demographic data, preoperative variables, operative parameters, variables related to postoperative morbidity, and status at hospital discharge were analyzed retrospectively. The variables on postoperative morbidity included fever requiring antibiotic therapy, systemic infection or endocarditis, superficial sternal infection, mediastinitis, respiratory failure (mechanical ventilation for more than 72 hours), renal failure or dialysis requirement (creatinine >2.5 mg/dL for more than 7 days), stroke, new myocardial infarction, repeat surgery due to bleeding, and additional surgery requirement.
Follow-up survival information was obtained through postoperative visits to our department and by cross matching the patient's Social Security number with the web-based Social Security death index.
Compilation of HIV-Specific Data
The study was approved by the institutional review board of our hospital and the investigation period was in compliance with the Health Insurance Portability and Accountability Act (HIPAA) Privacy rule, thus meeting the international recommendations for clinical research set down in the Declaration of Helsinki of the World Medical Association (1975). All necessary precautions were taken to safeguard the patients' identity and avert any possible link to identification from the study data.
The clinical variables specifically related to HIV infection included coinfections due to hepatitis viruses B and C (HBV and HCV), AIDS clinical status, and CD4 lymphocyte count (cells/µL). Patients were classified by clinical stage using the Centers for Disease Control and Prevention (CDC) revised system for staging HIV infection in adolescents and adults.4 Variables related to the therapeutic regimen included the use of any parallel treatment, HAART regimen (including PIs), and degree of compliance with treatment as self-reported by the patient.
Operative Safety Measures
Standard infection control measures were taken for the surgical management of HIV patients, including the use of double surgical gloves and complete, impermeable face shields. Specialists with advanced training were assigned to each procedure to avoid any type of wound during surgery. There were no operative accidents of any type during the study period.
Statistical Analysis
Values are expressed as the mean (standard deviation [SD]) or median and interquartile range (IQR) for quantitative variables. Discrete variables are expressed as percentage of the sample. Kaplan-Meier curves were used to provide a graphic representation of survival (percentage [standard error]). Statistical analyses were performed with SPSS 15.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
The clinical characteristics of the patients are shown in Table 1. The study population included 30 (77%) men and 9 (23%) women with a mean age of 49 (10) years. The mean ejection fraction (EF) was 44% (15%).
HIV Infection-Related Data
HIV transmission occurred by the following routes: sexual contact in 14 (36%) patients; parenteral in 24 (61%) drug abusers, and transfusion in 1 (3%). Fourteen patients (35%), all intravenous drug abusers, had hepatitis coinfection. CD4 lymphocyte counts were <500 cells/µL in 56% (n=22) of patients. Based on the CDC classification system, 23 (59%), 6 (15%), and 10 (26%) patients were in clinical stage A, B, and C respectively; 13 (36%) patients had a history of opportunistic infections. Among the total, 70% (n=28) of patients were actively receiving antiretroviral treatment at the time of surgery, whereas 30% (n=12) were not under any treatment. The HIV-related epidemiologic, clinical, and therapeutic data, as well as information on evolution are shown in Table 2.
Preoperative Risk Factors
Sixteen patients (41%) presented congestive heart failure (NYHA functional class III-IV), and 9 (23%) had preoperative renal failure. In addition, 4 (10%) presented advanced liver cirrhosis secondary to HBV and HCV coinfections (Child B, n=3; Child C, n=1). Among the 39 surgical procedures carried out, 5 (13%) were performed on an emergency basis, and 6 (15%) were performed in patients with a history of prior cardiac surgery.
Indication for Surgery and Operative Details
The most frequent indication for surgery was infective endocarditis (n=16; 41%). The disease was multivalvular in 8 (20%) patients and in the active phase in 9 (23%) patients. Isolated coronary disease, occurring in 12 (31%) patients, was the second most common indication, 7 (18%) patients had aortic disease, and the 4 (10%) remaining patients presented degenerative valvular disease that was unrelated to prior endocardial processes.
Details on the surgical procedures are shown in Table 3: 15 (38%) patients underwent valve surgery alone, 12 (31%) had coronary artery surgery (CS) for myocardial revascularization, 7 (18%) had aortic surgery, and 5 (13%) had combined surgery. The duration of aortic clamping and on-pump circulation was 110 (43) min and 158 (37) min, respectively.
Morbidity and Mortality
The mortality rate during hospitalization or within the 30 days following surgery was 5% (n=2). In both patients the cause of death was multiorgan failure. The first patient had undergone emergency surgery for fulminant infective endocarditis, and the second presented multiorgan failure secondary to prolonged low cardiac output syndrome following aortic surgery.
Postoperatively there were 2 (5%) cases of systemic infection, 1 (3%) of stroke, 2 (3%) of renal failure, and 5 (13%) of respiratory failure. Among the patients with preoperative end-stage liver failure, 2 (7%) had to be reoperated because of active bleeding. There were no postoperative complications in 29 (72%) patients. Furthermore, there was a notable absence of opportunistic infections during the hospitalization period. The median duration of hospital stay was 7 (IQR, 6-10) days; only 9 (23%) patients required more than 10 days of hospitalization. Postoperative events are summarized in Table 4.
Clinical Follow-up
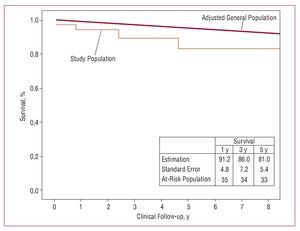
Clinical follow-up was complete in 100% of cases. After a follow-up period of up to 8.2 years, the crude late mortality rate was 10.8% (4/37). Survival was 91.2% (4.9%) at 1 year, 86% (7.2%) at 3 years, and 81% (8.4%) at 5 years (Figure 2).
Figure 2. Kaplan-Meier curve in HIV-infected patients undergoing cardiovascular surgery. The straight line represents survival of the general population of the USA, age- and sex-adjusted to the study population.
DISCUSSION
In the present retrospective study, we describe our clinical experience with 39 HIV-infected patients consecutively undergoing cardiovascular surgery. To our knowledge, this is one of the largest series of such patients in the contemporary literature. The operative mortality rate was 5% (n=2), there were no postoperative complications in 29 (74%) patients, and no events of any kind in the group undergoing CS.
Morbidity and Mortality
It is unusual to come across articles investigating and analyzing surgical outcome in HIV patients, and even more so in the case of cardiovascular surgery. The studies published to date with a sample larger than 30 patients are listed in Table 5.5-8
In a retrospective study covering a period of 17 years (1985-2002) and including 31 HIV-positive patients who underwent cardiovascular surgery, Mestres et al6 reported a mortality rate of 23%. Among the total, 68% of patients had infective endocarditis, and only 16% were treated for coronary disease. All deaths occurred in patients undergoing valvular surgery, whereas there were no inhospital deaths among the patients who required CS. In the study by Trachiotis et al,7 operative mortality was 2.7% in a cohort of 37 patients, the majority of them (n=27; 73%) treated with CS. Similarly, there were no deaths in the group with coronary disease. Lastly, in a recent case-control study of patients undergoing CS (n=7) Jiménez-Expósito et al9 reported postoperative mortality only in the control group (HIV-negative), thereby supporting the findings highlighted in previous studies. Our experience with 39 consecutive patients (valvular surgery, 51%; CS, 31%; aortic surgery, 18%) over 9 years yielded an overall mortality of 5%, with no deaths whatsoever in the group of patients undergoing CS.
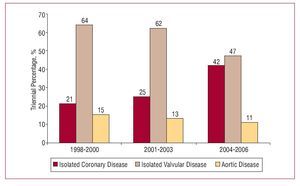
The decrease in operative mortality observed in the most recent series is likely to have several causes, involving factors such as the progress made in therapy for HIV infection and AIDS with the development of HAART, and the numerous advances in perioperative management of surgical patients over the last decade.10,11 Furthermore, the number of patients with infective endocarditis has decreased considerably, whereas the total number of patients who are candidates for CS continues to increase among the HIV population, and these facts have a relevant impact on mortality rates (Figure 3).12-14 Thus, morbidity has become the focus of attention in this type of patient, particularly (and obviously) complications of an infectious nature. In the present study, postoperative complications occurred in 10 (25%) patients, all of whom had important preoperative risk factors, such as end-stage liver failure, renal failure, and active endocarditis. There were no postoperative complications in any of the patients undergoing CS (31%). Chong et al15 reported similar results in patients treated with CS, documenting a low incidence of postoperative systemic infections, which indicates a more than acceptable state of perioperative immunocompetence in these patients.7
Figure 3. Triennial stratification of surgical indications in HIV-infected patients undergoing cardiovascular surgery.
Coronary Disease in HIV-Infected Patients
In the stage of expansion of the HIV disease, infective endocarditis was the most common, if not the only, indication for surgery in HIV-positive patients undergoing cardiac surgery.12 In contrast to what has occurred in the general population, however, the most recent clinical studies have shown a growing number of patients referred for CS. A progressively longer life expectancy has resulted in exposure of HIV-positive patients to the most common cardiovascular risk factors. Moreover, the new HAART-and PI-based therapeutic regimens have contributed notably to the development of early cardiovascular disease.16,17 An increasing number of studies have correlated HAART therapies with the development of metabolic syndrome, hypercholesterolemia, lipodystrophy, and insulin resistance.18-22 In a surgery article, Trachiotis et al7 described a significant increase in cholesterol concentrations in the vast majority of HIV patients undergoing CS (19/23; 83%). In parallel, the virus has been reported to produce adverse effects of chronic inflammation in the coronary circulation.23 HIV seems to contribute to the development of endothelial injury and consequently, to enhance problems related to arteriosclerosis.
All these findings indicate that HIV-infected patients receiving various aggressive treatments require intensive cardiologic monitoring, particularly when cardiovascular risk factors have been detected.24
CONCLUSIONS
The introduction of new antiretroviral therapies has resulted in a longer life expectancy and increased need for cardiac surgery in HIV patients. Currently, cardiovascular surgery in patients with HIV infection/AIDS can be carried out in a completely safe manner and with clearly promising outcomes. In addition, this study shows that long-term survival can reach more than 80% in these patients. Lastly, we believe that HIV-infected patients receiving various aggressive therapies require careful supervision and close cardiologic follow-up, particularly when they have risk factors for coronary disease.24
ABBREVIATIONS
AIDS: acquired immunodeficiency syndrome CS: coronary surgery
EF: ejection fraction
HAART: highly active antiretroviral therapy HIV: human immunodeficiency virus
PI: protease inhibitor
Project funded by the Department of Cardiothoracic Surgery.
Correspondence:
Dr J.G. Castillo,
Research Fellow, Department of Cardiothoracic Surgery, Mount Sinai Medical Center,
1190 Fifth Avenue, New York, NY 10029-1028, USA
E-mail: javier.castillo@mountsinai.org
Received July 3, 2007.
Accepted for publication January, 2008.