Keywords
INTRODUCTION
The gradual aging of the Spanish population poses important social, economic, and public health challenges. According to data provided by the last census, octogenarians currently form 4.3% of the total Spanish population and this percentage is even higher in Castilla and León.1 On the other hand, progress in surgical techniques and perioperative care has made it possible to operate on elderly patients with a reasonable level of risk. Thus, the age of patients undergoing cardiac surgery has significantly increased in recent years.2
However, whereas indications for surgery are rarely discussed in relation to patients aged 75-79 years, they are frequently questioned in relation to octogenarians. A patient older than 80 years represents, for cardiologists and surgeons alike, a psychological barrier that identifies a high-risk population for interventionist procedures, and surgical procedures in particular. This attitude is not always justified and can prevent specific patients benefiting from all the therapeutic resources at our disposal. Unfortunately, we have little information on the outcomes of cardiac surgery in octogenarians in Spain.
The present study has 2 aims: to investigate early morbidity and mortality and the medium-term clinical outcomes of cardiac surgery in octogenarians and compare them with outcomes in other elderly patients (75-79 years), and to identify the factors determining early and late mortality and major complications in this population, with the aim of improving the selection of octogenarians who can benefit from surgical treatment.
METHODS
Between October 1999 and September 2006, a total of 2258 patients underwent major cardiac surgery in our hospital. Of these, 140 (6.2%) were 380 years (group I) and 449 (19.9%) were 75-79 years (group II). The surgical indication was agreed by cardiologists and surgeons in consensus, either during regular clinician-surgeon review sessions or after conferring with the duty medical team. When selecting octogenarian patients, special attention was paid to the preoperative assessment of comorbidity, the degree of autonomy and family support. No patient was rejected exclusively because of age. A total of 11.2% of the octogenarians and 9% of the septuagenarians who attended medical-surgical assessment were rejected due to anatomical or clinical circumstances that made surgery inadvisable (P=.473). No records were kept in relation to these patients.
The perioperative data and clinical evolution of each patient were prospectively included in the hospital database (Cardiac Surgery Computer System, version 11.3, Sorin, Milan, Italy). The patients who needed more than 1 surgical procedure (4 patients) were included as different patients in the analysis of early morbidity and mortality and as just 1 patient in the survival analysis.
The preoperative variables analyzed were as follows: age, sex, body mass index, cardiovascular risk factors, chronic obstructive pulmonary disease, peripheral vascular disease, kidney failure (creatinine >2 mg/dL), intraaortic balloon counterpulsation (IABP), and a history of cardiac intervention, stroke, or myocardial infarction (AMI). We assessed functional class in line with the Canadian Cardiovascular Society and New York Heart Association criteria, as well as heart rate at admission, coronary anatomy, the valvular lesion, the degree of left ventricular dysfunction (mild, 50%-59%; moderate, 30%-49%; and severe, <30%) and pulmonary hypertension (mild, 25-39 mm Hg; moderate, 40-59 mm Hg; and severe, >59 mm Hg). Surgical risk was calculated for each patient using EuroSCORE.3
The perioperative factors analyzed were as follows: priority, type of intervention, number of coronary vessels revascularized and grafts used, type of valvular procedure and intervention times, cardiopulmonary bypass (CPB), aortic cross-clamping, and circulatory arrest.
Surgery with CPB was performed under light hypothermia, using a centrifugal pump, and cold blood cardioplegia in combination (antegrade induction, and maintenance, and retrograde warm blood reperfusion). Intraoperative cell salvage was systematically performed. The myocardial revascularization procedures with CPB were performed during a single aortic cross-clamping period.
The following postoperative complications were recorded: early bleeding requiring reintervention, late tamponade, perioperative AMI (appearance of a new pathological Q wave in the electrocardiogram or ST-segment elevation and markers of myocardial damage) low cardiac output (need for perioperative or postoperative IABP or for inotropic drugs for more than 48 h), bacteremia, pneumonia, mediastinitis, intestinal ischemia, other gastrointestinal complications (intestinal obstruction, cholecystitis, upper or lower gastrointestinal bleeding requiring transfusion), respiratory failure (mechanical ventilation for more than 48 h, tracheostomy, or readmission to the intensive care unit due to respiratory problems), stroke (transient or permanent neurological dysfunction), delirium, kidney failure requiring extrarenal dialysis, atrial fibrillation (AF), permanent pacemaker, and transfusion of blood components. All such complications were considered major except for well-tolerated AF, delirium, and the need for transfusion not associated with other complications. Early mortality was defined as occurring during hospitalization or during the first 30 days after surgery following discharge.
Follow-up was conducted by telephone interview and check-up in the hospital outpatient department between 1 September and 1 December 2006. Data on the clinical history of the patients attending our hospital were included. Patients from other hospitals who had experienced adverse events sent in a copy of their discharge report by mail. The average follow-up time was 2.8 (1.5) (median, 2.6) years, and was completed in all patients. Early death, cardiovascular death, or death due to unknown causes during follow-up, the need for new procedures, and hospitalization due to cardiac causes were considered adverse cardiac events.
Statistical Analysis
The Kolmogorov-Smirnov test was used to verify whether the variables followed a normal distribution. Continuous variables were expressed as the mean and standard deviation or the median and interquartile range (IQR, 25-75) when the variable was not distributed normally. Discrete variables were expressed as absolute numbers and percentages. Continuous variables were compared by analysis of variance or Student t test, and discrete variables by c2 corrected with Fisher's exact test when necessary. All variables with P£.1 in the univariate analysis were included in a multivariate logistic regression model to investigate the determinants of serious postoperative complications and hospital mortality. The validity of the model was assessed by ROC curve analysis. The survival rate was determined by the Kaplan-Meier method, using the log-rank test for between-group comparisons. Independent risk factors of mortality during follow-up were analyzed by Cox proportional hazard model. The statistical analysis was performed with SPSS software version 13.0 (SPSS, Chicago, Illinois, USA).
RESULTS
The proportion of octogenarians undergoing interventions in our hospital increased from 2.1% in 2000 to 9.2% in 2006, whereas the percentage of patients between 75 and 79 years varied little during the same period (from 17.3% to 19.4%).
Preoperative Patient Characteristics
Table 1 shows the preoperative characteristics of the 2 groups. Both were similar, except for the higher prevalence of previous AMI and moderate or severe ventricular dysfunction in the septuagenarians and unstable angina in the octogenarians. The estimated risk using Euro-SCORE was significantly higher in octogenarians, although the additive Euro-SCORE only differed by 1 point.
Operative Data
The distribution by categories was similar, except for surgery of the ascending aorta that was performed more frequently in octogenarians. A total of 40% of all patients undergoing valvular procedures required associated revascularization, with a similar prevalence in both groups. Mitral valve surgery, isolated and combined, were more frequent in the septuagenarians (Table 2).
Tricuspid valve annuloplasty was performed in 21% of the septuagenarian patients who required valvular surgery patients and in 14% of octogenarians. The use of tissue valves was significantly more frequent in octogenarians (97% vs 72%; P<.001). Mechanical valves were implanted in 2 octogenarians who required aortic valve surgery: 1 patient needed a valvular conduit and 1 was implanted with a small ring. Mechanical valves were implanted in septuagenarians in the case of preoperative AF.
Table 2 presents the data on coronary surgery. The total number of anastomoses per patient was similar in both groups. Revascularization without CPB was performed more frequently in octogenarians. The use of the internal mammary artery and the number of arterial grafts were significantly greater in the younger group. Nevertheless, the left anterior descending coronary artery was revascularized using the internal mammary artery in 91% of octogenarians.
Mortality
The early mortality rate was 10.7% divided by group as follows: 10% (14 patients) in group I and 10.9% (49 patients) in group II (P=.876). The main cause of death was infection (group I, 58.3%; group II, 48.8%), followed by low cardiac output (group I, 16.7%; group 2, 34.9%), respiratory complications (group I, 16.7%; group II, 2.3%) and gastrointestinal complications (group I, 8.3%; group II, 11.6%). Table 3 shows the mortality rates associated with the different types of intervention.
As expected, mortality associated with elective surgery was less than that associated with urgent or emergency surgery, both in octogenarians (7.4% and 26.3%, respectively; P =.06) and in septuagenarians (7.4% and 36.4%, respectively; P<.0001), although this was statistically significant only in the younger group.
Mortality associated with combined surgery was similar in both groups and higher than that associated with isolated valvular surgery, although the difference was statistically significant in octogenarians (6/28 vs 1/43; P=.022). No significant differences in mortality were found between isolated and combined aortic valve replacement (group I, 0/33 vs 2/19; P=.129; group II, 4/84 vs 1/52; P=.649). In contrast, mortality associated with combined mitral valve replacement and coronary artery bypass graft surgery was significantly higher than isolated mitral valve replacement only in the younger group (group I, 2/5 vs 0/5; P.444; group II, 10/36 vs 4/42; P=.043).
The discrimination of the additive and logistic EuroSCORE was good, with an area under the ROC curve of >0.76 for both groups. The logistic EuroSCORE was a better predictor of total mortality and in the subgroups at greater risk (data not presented).
Table 4 shows the results of the multivariate analysis. Moderate-severe pulmonary hypertension, emergency surgery, and combined surgery were independent predictors of mortality. The area under the ROC curve was 0.78 for the model. The inclusion of serious postoperative complications in the model had a strong impact on mortality, especially gastrointestinal complications (odds ratio [OR], 146.4) and kidney failure (OR, 54.89).
Postoperative Morbidity
A total of 22% of the octogenarians and 30% of the septuagenarians presented some major complication during the postoperative period, although this difference did not reach statistical significance. Table 5 shows the major complications. The most frequent was AF (group 1, 41.4%; group 2, 42.1%) and was often associated with other more serious hemodynamic or respiratory complications. Only 30.3% (group I) and 27.2% (group II) presented isolated AF.
Six (4.3%) octogenarians and 21 (4.7%) septuagenarians required readmission to the ICU. The most frequent cause was respiratory failure, especially in the older group (group I, 83.3%; group II, 47.6%). Other causes included gastrointestinal complications, alterations in heart rate and subacute cardiac tamponade.
In the multivariate analysis, emergency surgery, moderate or severe pulmonary hypertension, CPB lasting more than 2 h, combined surgery, and advanced functional class (grade III-IV) were independently associated with the development of major postoperative complications (Table 6). The area under the ROC curve was 0.75 for the model.
Hospital Stay
There were no significant differences between the 2 groups in relation to preoperative and postoperative hospital stay (Table 5). The hospital stay of the patients who developed some complication were significantly longer (group I, 10 [8-15] days vs 8 [6,7-9] days; P<.0001; group II, 11 [8-16] days vs 7 [6-9] days; P<.0001). Postoperative AF not associated with other complications prolonged hospital stay by an average of 3.4 days in the octogenarians and 1.8 days in the septuagenarians.
Follow-up
The mean follow-up time of discharged patients was 2.6 (1.4) (median, 2.3) years in the octogenarians and 2.8 (1.3) (median, 2.6) years in the septuagenarians. There were 83 new deaths, 15 (10.8%) among octogenarians and 68 (15.2%) among septuagenarians, with no differences found in the cause of death. A total of 53% of the deaths among the octogenarians and 54% among the septuagenarians were of cardiovascular origin. Neoplasms were more frequent in septuagenarians (25%) than in octogenarians (6.7%).
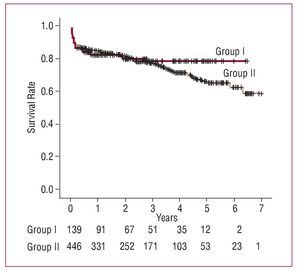
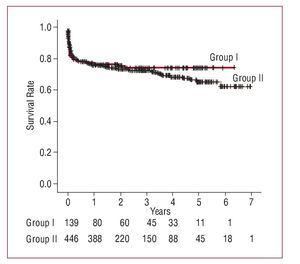
The actuarial survival rate, which included hospital mortality at 1 year, 3 years, and 5 years, was 82%, 79%, and 79% among the octogenarians and 85%, 77%, and 65% among the septuagenarians (P=.832) (Figure 1).Cardiac event-free survival at 1 year, 3 years, and 5 years was 77%, 75%, and 75% among the octogenarians and 76%, 72%, and 64% among the septuagenarians (P=.959) (Figure 2). The survival curves diverge at 3 years, in favor of the octogenarians, although the number of patients at risk is small. The multivariate analysis showed that the additive EuroSCORE and preoperative AF were associated with increased mortality during follow-up (Table 7).
Figure 1. Kaplan-Meier survival analysis during follow-up (P=.832).
Figure 2. Cardiac event-free survival during follow-up; Kaplan-Meier analysis (P=.959).
A total of 97% of the patients from both groups were in functional class I-II during follow-up and 71% of octogenarians were independent regarding daily life activities.
DISCUSSION
Age is an independent determinant of early mortality in cardiac surgery,4,5 and as such is included in different surgical risk scales.3,6 Surgery in octogenarians also involves an increased incidence of complications and increased hospital stay and consumption of resources.7-9 Their greater vulnerability to surgical trauma is due to the decreased functional reserve of different organs and systems. However, recent series have shown that mortality among octogenarians approaches that of younger patients.10
The aim of surgery in these patients is not only to improve the quality of life, as often argued, but also to survive diseases that have poor short-term prognosis with medical treatment.11 It should be borne in mind that life expectancy for 80-year-old people in Spain is 8.6 years.12
Indications for surgery in octogenarian patients is a complex issue and, in addition to clinical practice guidelines, other important aspects should be taken into account, such as the possible disparity between biological and chronological age, concomitant morbidity, autonomy, and family support.
Less than a third of the octogenarians who underwent surgery were women, despite constituting 65% of this population segment due to their greater life expectancy. Although this could be due to a selection bias regarding patients scheduled for surgery, other authors have highlighted less use of diagnostic and therapeutic resources in women.13
Total mortality among the octogenarians in our series was similar to that recently reported by other authors7,14-17 and less than that among the elderly reported by different Spanish groups.18,19 This was the case despite not excluding specific disorders that entail high surgical risk, such as the mechanical complications of myocardial infarction. Furthermore, mortality among the octogenarians was similar to that of septuagenarians. The octogenarians who underwent elective surgery had a mortality of 7.4% and this confirms that cardiac surgery can be performed in these patients with an acceptable level of risk.
Mortality among the octogenarians undergoing coronary surgery was similar to that reported by other authors.8,15,16 The use of the internal mammary artery, although significantly less in octogenarians (92% vs 98%), was far higher than that of other series (0% to 77%).7,8,20 Coronary revascularization without CPB in the elderly seems to be associated with less morbidity and mortality,21 although the low number of patients who were operated on with this technique in our series prevents us from drawing conclusions.
We should note the absence of mortality in isolated valve surgery (aortic and mitral) in the octogenarian group. Mortality in the octogenarians undergoing combined aortic and coronary surgery, although high, was similar to that reported in other series,8,15,22,23 nor was it greater than mortality in the septuagenarians. There is little experience with combined mitral valve surgery in octogenarians and, in general, the procedure has bad outcomes.8,22 Age and associated coronary revascularization are well-defined risk factors of mortality in mitral valve surgery.4 Disorders treated by emergency surgery, such as aortic dissection and mechanical complications of myocardial infarction, had high mortality in both groups, as found in other series.24,25 Emergency and combined surgery were independent risk factors of early mortality and postoperative complications, as reported by other authors.5,15,20,23
The estimated risk using EuroSCORE was significantly higher in octogenarians, although the difference was only 1 percentage point for the additive EuroSCORE and 2 points for the logistic EuroSCORE. This finding could be due to the fact that age involves a minimum of 5 points in octogenarians and 4 in septuagenarians. In our experience, the discrimination of the EuroSCORE was good in the elderly. The logistic EuroSCORE was a better predictor of mortality in the patients at greater risk, as other researchers have pointed out.26
The incidence of postoperative complications in the octogenarians was similar to that in the septuagenarians and to that reported in other studies.8,14,15,20 It should be recalled that age is an independent risk factor for the development of many such complications.27,28 Atrial fibrillation was the most frequent complication and its appearance prolonged hospital stay, in view of the fact that recurrences are not infrequent and patients were not discharged until conversion to sinus rhythm had occurred. Less frequent complications, such as gastrointestinal ones and kidney failure, were associated with greater hospital mortality in the multivariate analysis, as other authors have noted.18,19,28
In our study, the low incidence of reinterventions due to bleeding and neurological complications (stroke and delirium) should be noted.8,14,15,20,29 The former could be due to the standard administration of antifibrinolytic agents, and the latter due to the protocol followed in our group to prevent neurological complications. This consists in maintaining high perfusion pressure during CPB, external compression of both carotid arteries during aortic cross-clamping and unclamping maneuvers, the systematic use of transesophageal echocardiogram to guide cardiac venting and proximal anastomosis of the coronary grafts with single aortic cross-clamping. Furthermore, the use of the centrifugal pump seems to reduce the incidence of stroke.30
Although a cost analysis was not one of the aims of the present study, no differences were found between the 2 groups regarding intubation time, hospital stay, or the need for transfusions, that would entail a similar consumption of resources, unlike that reported by other authors.7,16
The actuarial survival of the octogenarians was similar to that of the septuagenarians, with 75% of the patients being free of cardiac events at 5 years. This result could be partly due to the natural selection of individuals we could call "biologically advantaged" and who have reached 80 years with excellent life expectancy. On the other hand, the almost unvarying use of the internal mammary artery for coronary revascularization could have contributed to these outcomes.22,31
The additive EuroSCORE and preoperative AF were independently associated with increased mortality during follow-up, as other authors have reported.32,33 The former could be due to including some of the variables of greater prognostic relevance in these patients, such as ventricular dysfunction, peripheral vascular disease, etc. Atrial fibrillation is a risk factor of stroke and bleeding complications associated with anticoagulation treatment and AF itself may lead to heart failure.
The results may have been affected due to the study being retrospective. In addition, there may have been biases in the selection of octogenarians referred for surgical evaluation and in relation to those accepted for intervention. Furthermore, no record was made of patients who were not referred for surgery, those who refused surgery or those who refused after being given further information. On the other hand, it is difficult to control all the possible confounding variables, some of which are difficult to quantify, such as the general state of the patient. However, the fact that octogenarians with complex diseases underwent surgery indicates that this subgroup was fully represented.
CONCLUSIONS
Cardiac surgery in selected octogenarians has outcomes similar to those obtained in other elderly individuals of a less advanced age, including those with complex diseases, with good medium-term survival rates, and quality of life. Pulmonary hypertension, emergency surgery, and combined surgery are risk factors of mortality and, together with advanced functional class, and prolonged CPB time, are risk factors of serious postoperative complications. Early surgical correction may avoid the need for operating on these patients in such unfavorable conditions. Preoperative AF and the additive EuroSCORE were associated with increased mortality during follow-up.
ABBREVIATIONS
AF: atrial fibrillation
AMI: acute myocardial infarction
CPB: cardiopulmonary bypass
IABP: intraaortic balloon counterpulsation
SEE ARTICLE ON PAGES 564-6
Correspondence:
Dr. F.J. López Rodríguez.
Servicio de Cirugía Cardiaca. Hospital Universitario de Salamanca. P.o de San Vicente, 58-182 3.a planta. 37007 Salamanca. España.
E-mail: jlopezrodri@wanadoo.es
Received October 13, 2007.
Accepted for publication March 4, 2008