Keywords
INTRODUCTION
A recently published study has modified the classical concept of the ischemic cascade, demonstrating, in 100% of the cases studied, that the earliest event to take place in ischemia is the prolongation of the corrected QT (QTc) interval.1 Abnormal prolongation of the QTc interval has been reported in patients with unstable angina (UA)2 or ST-segment elevation acute myocardial infarction (AMI). Moreover, this variable has been found to be an independent predictor of arrhythmic death following AMI.4,5 In line with this observation, the ACTION trial demonstrated that, in patients with coronary artery disease, a QTc interval longer than 430 milliseconds was a predictor of death comparable to 3-vessel disease (odds ratio [OR], 1.52 vs OR, 1.14)6; however, this study was performed in patients with stable coronary artery disease. The prolonged QTc interval detected in patients with UA or AMI7,8 returned to normal values 48 hours after satisfactory myocardial revascularization. It has been speculated that the normalization of this interval in patients who have undergone angioplasty is a marker of satisfactory reperfusion.9
We have recently reported that the prolongation of the QTc interval is an independent risk marker in patients with UA.10 The objective of this study was to demonstrate the prognostic value of a prolonged QTc interval in patients admitted to the coronary care unit with a diagnosis of non-ST-elevation acute coronary syndrome (NSTEACS) and with a normal electrocardiogram (ECG) showing no evidence of acute ischemic changes.
METHODS
Patients
Since January 1995, we have studied 426 consecutive patients admitted to the Coronary Care Unit of Hospital Interzonal General de Agudos Eva Perón (a provincial university acute care hospital specializing in highly complex cases and general medicine) in Buenos Aires, Argentina, for the purpose of investigating the behavior of the QTc interval in UA and non-ST-elevation AMI, classified as IIB or IIIB according to the Braunwald criteria. We define UA as: typical anginal pain, with no elevation of biochemical markers, with or without ECG changes. Cardiac troponin T (cTnT) levels 30.04 ng/mL or a creatine kinase MB fraction (CK-MB) >5%, determined within 24 hours of admission, were considered to be abnormal, and served to differentiate patients with some degree of necrosis from those in whom there was no biochemical evidence of this complication (UA).
In no case was there electrocardiographic documentation of ST-elevation (transmural) AMI, according to the ACC/AHA criteria.12 We wish to point out that we included only patients with normal ECG (n=39) or with no new onset ischemic changes (n=16), as compared to an ECG performed within the preceding 6 months, in order to comply with the specific objective of this study. The latter 16 patients in whom ECG was not normal had sequelae of AMI (n=13), left anterior hemiblock (n=2), or complete right bundle branch block (n=1). This investigation was carried out with the intention of extending our previous observations in patients with UA who did present with acute ischemic changes on admission ECG.10
The systematic use of cTnT determinations was not introduced in our hospital until November 12, 2001; thus, 328 cases in which this parameter had not been measured could not be included in the protocol. Of the remaining 98 patients, we excluded 41 with new onset negative T waves, 1 with severe heart failure and 1 with a QRS complex duration 30.12 seconds. Other exclusion criteria taken into account for patient selection were: secondary unstable angina, post-AMI angina pectoris, severe valve disease or cardiomyopathy, serum potassium concentration £3.5 mEq/mL, treatment with any antiarrhythmic agent or drug that could have modified the QTc interval at the time of admission, and arrhythmias like Wolff-Parkinson-White syndrome, atrial fibrillation, atrial flutter, and ventricular or atrial premature beats. The 55 patients that remained after application of the exclusion criteria constituted the study population. The coronary origin of the disease was confirmed by coronary angiography in 29 cases (52.7%), whereas 14 patients (25.5%) had a history of coronary artery disease, and the remaining 12 (21.8%) underwent functional tests to provoke ischemia. With respect to the 29 patients in whom coronary angiography was performed to evaluate the severity of the coronary artery disease, significant obstructive lesions were observed in 25, and normal coronary arteries in 4.
Ventricular function was considered to be normal when 2 of the following 3 criteria were met: a) a shortening fraction 325%; b) a mitral valve E point septal separation <0.8 cm; and c) agreement between 2 experienced echocardiographers in that systolic function was conserved.
All the patients included in the study (16 of whom had high cTnT concentrations [30.04 ng/mL]) had primary angina pectoris. Upon admission, they all received conventional treatment with aspirin, heparin, intravenous nitroglycerin, and atenolol. The dose of beta-blockers considered to be useful was that which achieved a heart rate that did not surpass the baseline rate by more than 10% following a maneuver to induce tachycardia.
Twelve-lead ECG was performed at hospital admission in every case, and blood samples were collected more than 6 hours after the onset of the most recent episode of anginal pain. The cTnT level was determined by means of chemiluminescence using approved commercially available reagents. Concentrations 30.04 ng/mL were considered to indicate myocardial injury. In addition, at admission, risk stratification was performed in each patient according to the Thrombolysis in Myocardial Infarction (TIMI) score for NSTEACS.13
All the patients gave their written informed consent prior to being included in the study, which was approved by the local ethics committee.
Clinical Characteristics, Follow-up, and Objectives of the Study
The variables included at the time of enrollment in the study were: age, sex, height, weight, arterial blood pressure, history of myocardial infarction, hypertension, diabetes mellitus, smoking, hypercholesterolemia, family history of coronary artery disease, cerebrovascular disease, and previous coronary angioplasty. No patient had peripheral vascular disease. Medication being taken prior to inclusion in the study was also recorded.
Following baseline characterization, all the patients were subjected to 1 month of post-discharge follow-up.
The clinical events observed over the 30 days following discharge from the hospital, which constituted the combined endpoint, were: cardiac-related death, nonfatal myocardial infarction (defined according to the ACC/AHA criteria: increase in cardiac enzyme levels, characteristic electrocardiographic changes, and typical chest pain lasting at least 20 minutes), and the need for percutaneous or surgical revascularization due to recurrent angina, a positive functional test in the provocation of ischemia, or criteria indicative of high clinical or hemodynamic risk.
Measurement of the Corrected QT Interval
Two independent experienced investigators (FG and SL), who were not involved in decision making, performed the manual measurement of the QTc interval using a hand-held instrument and a magnifying glass, as described in an earlier study carried out by our group.10 We analyzed the measurements recorded for each patient at admission, 12, 18, and 24 hours later, and daily thereafter. The longest QTc interval obtained from the measurements made in the ECG performed from the time of admission to 24 hours later was taken as the final value. The electrocardiographic recordings involved 12 leads and standard gain, and were obtained with a Schiller Cardiovit AT-1 ECG (Schiller AG, Baar, Switzerland) and, depending on the clinical circumstances of each patient, the tracings were acquired in the presence of pain or after it had subsided. The QT interval was measured from the beginning of the QRS complex to the end of the T wave, defined as the point at which the T wave returns to the isoelectric line, or the nadir between the T wave and the U wave, when the latter is present. In all the ECG, the QT interval was measured at precordial leads V2,V3, and V4 for 2 reasons: first, the T wave acquires its greatest amplitude in these leads and, second, they also coincided with the closest agreement between the 2 observers.14,15 The measurements recorded in the 3 leads were averaged, and this value was considered to represent the duration of the QT interval for that ECG, as measured by 1 of the 2 investigators. Subsequently, the average calculated by each of the 2 investigators was again averaged, and this final value was that taken into account for the analysis. The variability between these observers was calculated on the basis of the relative risk, which was determined using the formula: (A-B)/([A+B]´0.5)´100, where A and B are the QTc intervals in the measurements made by each of the 2 observers.16 To obtain the QT interval corrected for the heart rate, the Bazett formula was employed.17 Corrected QT intervals with durations greater than or equal to 0.45 seconds in men and greater than or equal to 0.47 seconds in women were considered to be abnormally prolonged.
Statistical Analysis
The results of the continuous variables having a normal distribution are expressed as the mean plus or minus the standard deviation (SD) and the continuous variables having a non-normal distribution are expressed as the median (interquartile range). The Kolgorov-Smirnov test was used to analyze the normality of the distribution of the continuous variables, which were compared by means of the unpaired t test or the Mann-Whitney U test, as appropriate. The proportions were compared using the χ2 test or Fisher's exact test if the number of expected values was <5. The correlation between 2 continuous quantitative variables that follow a normal distribution was assessed with the Pearson correlation test. Information on the presence or absence of the combined endpoint was obtained for all the patients. The independent predictors of the combined endpoint were determined using binary logistic regression analysis. The analysis of the parameters by means of binary logistic regression involved the application of the Wald test, and a forward stepwise selection procedure was carried out, for which a probability of inclusion of 0.05 and of exclusion of 0.1 were chosen. The variables included in the multivariate analysis were the TIMI score, a cTnT level 30.04 ng/mL and a QTc interval of 0.458 seconds (the best cut-off point provided by the receiver operating characteristic [ROC] curve).
The differences were considered to be statistically significant if the null hypothesis could be rejected at a confidence level of over 95%. The SPSS 15.0 statistical software package (SPSS, Inc., Chicago, Illinois, United States) was used for all the calculations.
RESULTS
On admission, 39 patients (71%) had normal ECGs; in the remaining 16 (29%) with a history of coronary artery disease, the ECGs were abnormal, but revealed no new onset acute ischemic changes when compared to previous ECGs; 21 patients (38%) experienced clinical events (Table 1) during follow-up; while the remaining 34 (62%) did not. The clinical and demographic characteristics of the patients in whom clinical events were reported (group A) and of those in whom they were not (group B) are shown in Table 2.
The mean QTc interval was longer in the group in which events were reported (0.487 [0.053] seconds) than in the event-free group (0.44 [0.022] seconds; P=.001).
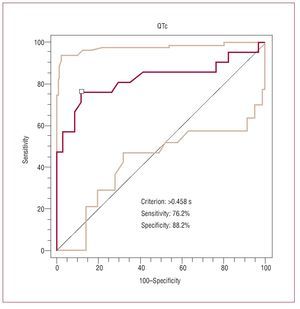
On the basis of the reference values for the QTc interval corresponding to each sex, this parameter was prolonged in 17 patients (81%) in group A, versus only 6 (17.6%) in group B (P=.0001; Table 2). We should point out that, in agreement with the analysis of the ROC curve, the best cut-off point for the QTc interval in terms of the prediction of clinical events was 0.458 seconds, with a sensitivity and a specificity of 76.2% and 88.2%, respectively (area under the ROC curve equal to 0.825; Figure 1).
Figure 1. Receiver operating characteristic (ROC) curve constructed to establish the cut-off point for the QTc (corrected QT) interval having the highest sensitivity and specificity for clinical events (QTc=0.458 s).
After adjustment using binary logistic regression, the QTc interval was found to be the only independent risk variable (OR, 19.8; 95% confidence interval [CI], 4.8-80.5; P=.001). The TIMI risk score was excluded from the independent predictors of the combined endpoint (P=.13), as was cTnT (P=.09). Other variables that were not predictors of events in this model were: age (P=.09), sex (P=.16), smoking (P=.07), hypercholesterolemia (P=.09), diabetes mellitus (P=.23), hypertension (P=.51), history of infarction (P=.88), and left ventricular dysfunction (P=.06). It should be pointed out that there was a positive and statistically significant correlation between the cTnT levels and the QTc interval (Pearson correlation = 0.78; P<.001).
The incidence of events was higher in patients with a TIMI risk score above the median and with a QTc interval 30.458 seconds, as compared to the rest of the study population.
DISCUSSION
The results of the present study demonstrate for the first time that the QTc interval predicts adverse cardiovascular events up to 30 days after hospital discharge in patients with NSTEACS who had a normal ECG or no new onset ischemic changes at admission.
The relevance of our findings lies in the fact that, despite the recording of a normal ECG or the absence of ischemic changes of new onset at admission, the patients with a prolonged QTc interval had a 19-fold higher risk of cardiovascular events. The measurement of the QTc interval, added to that of the troponins, which are universally recognized as prognostic biomarkers, would undoubtedly provide strong support for the interpretation of the diagnosis and the prognosis in this patient population. On the basis of our findings, 0.458 seconds should be taken as the QTc interval indicative of the risk of a cardiovascular event in patients with NSTEACS. This cut-off point is very similar to that reported recently by Jiménez-Candil et al.18
When compared with the patients who did not experence cardiovascular events, those who reached the combined endpoint of death, AMI or percutaneous or surgical revascularization up to 30 days after hospital discharge had longer QTc intervals. In any case, we do not rule out the possibility that these results would have varied had we decided to prolong the follow-up period.
Our findings confirm and extend our previous results and those of Jiménez-Candil et al in patients with acute coronary syndrome, in which the QTc interval was a useful early marker for cardiovascular risk in patients with an abnormal ECG pattern at admission produced by acute myocardial ischemia.10,18
In the present study, we have also found a positive correlation between prolonged QTc intervals and cTnT levels. The latter observation could suggest that the prolongation of the QTc interval is not only associated with myocardial ischemia, but with myocardial injury linked to the presence of limited areas of focal necrosis (micronecrosis). In agreement with our findings, Doven et al19 observed a direct relationship between QT dispersion and cTnT levels in patients with UA. Likewise, Rukshin et al20 reported that the prolongation of the QTc interval was more marked in patients with non-Q-wave AMI than in those with UA who exhibited no evidence of myocardial injury.
In 1990, Renkin et al21 documented their experience in a series of patients with UA and persistent negative T wave that indicated the presence of myocardial stunning. Interestingly, the ECG employed as an example in their article, performed prior to coronary angioplasty, revealed the presence of a prolonged QTc interval.
In the same year, Shawl et al2 produced the first publication addressing the subject of the QTc interval in patients with UA; it involved a series of patients who underwent coronary angioplasty to treat critical lesions proximal to left anterior descending coronary artery, in whom the ECG prior to the procedure revealed prolongation of the QTc interval, which was restored to normal after treatment.
Although our follow-up was relatively short, and the longer-term results may be uncertain, Jiménez-Candil et al18 have recently reported that the QTc interval was found to be a predictor of risk, both over the short term and for up to 1 year, in a series of 427 patients with NSTEACS and several types of electrocardiographic abnormalities at admission.
In some way, the rate of events in our series was surprising, considering that, at admission, the patients had normal ECG or abnormal ECG but no new onset acute changes. In addition to this circumstance, they also had a low mean TIMI risk score. However, all the patients had a number of risk factors and were asymptomatic at admission; the clinical course of 52.7% of them indicated the need for coronary angiography, and 30% had had a previous AMI. Twenty-one of the patients in group A experienced clinical events, and the QTc interval was prolonged at admission in 52% of them. Together, these observations indicate that the prolonged QTc interval may be a good predictor of cardiovascular risk and a useful diagnostic tool in patients who are admitted to the hospital with NSTEACS and normal ECG.
One question of interest that contradicts affirmations published by other authors, who reported the association between the increase in QT dispersion and the onset of death due to cardiac arrhythmia in patients with coronary artery disease, none of the participants in our study had severe ventricular arrhythmia or arrhythmic death.22 Thus, the prolongation of the QTc interval in our patients was a predictor of risk for ischemia, not arrhythmia.
Study Limitations
The weakest point of our work is probably the number of patients, and this could lead to unstable results and be the reason for the exclusion of the TIMI score and the cTnT, both well-known prognostic predictors, as independent variables. The reason for including 55 patients was that recruitment was carried out in only 1 center and the subjects had to be individuals with NSTEACS who, at admission, had a normal ECG or exhibited no new onset changes when the comparison was made with a previous ECG performed within the preceding 6 months. This last point was decisive when it came to selecting the patients. It made it necessary to resort to the study of a combined endpoint, with the understanding that if death had been the only consideration, the population could have been much larger.
Likewise, the follow-up period was short (up to 30 days after hospital discharge), since our objective from the start was to evaluate the QTc interval as a predictor of risk soon after discharge, without ruling out the possibility of variations in the results if we had proposed a longer follow-up period. In any case, it will be necessary, in the future and with a larger series of patients, to confirm these results, which may have been influenced by other factors, not contemplated in this patient population.
CONCLUSIONS
Our data indicate that the prolongation of the QTc interval in patients with NSTEACS having a normal ECG or one that shows no new onset acute ischemic changes is an independent predictor of cardiovascular risk, and that 0.458 seconds may be the cut-off point to be taken into account.
The purpose of this study is to call attention to a novel approach that can be made available in any emergency cardiac setting. However, we are aware of the fact that studies involving larger numbers of patients will be necessary to confirm and compare the predictive value of the QTc interval.
ABBREVIATIONS
AMI: acute myocardial infarction
cTnT: cardiac troponin T
ECG: electrocardiogram
NSTEACS: non-ST-elevation acute coronary syndrome
QTc: corrected QT interval
ROC: receiver operating characteristic
SD: standard deviation
TIMI: thrombolysis in myocardial infarction UA: unstable angina
Correspondence:
Dr. F.L. Gadaleta.
Jefe de Unidad Coronaria. Servicio de Cardiología. Hospital Interzonal General de Agudos Eva Perón. Ricardo Balbín 3200. (1650) San Martín. Provincia de Buenos Aires. Argentina.
E-mail: fgadaleta@intramed.net
Received July 2, 2007.
Accepted for publication March 4, 2008.