Keywords
INTRODUCTION
Cardiac resynchronization therapy (CRT) has been demonstrated to improve clinical outcomes and left ventricular (LV) performance in advanced heart failure patients.1,2 However, there is still a significant percentage of patients who do not show any clinical or echocardiographic response to CRT.1,3,4 One of the reasons proposed to explain the lack of response to CRT is the absence of LV dyssynchrony.3,4 The QRS duration on electrocardiogram is the parameter proposed by current guidelines to define LV electrical dyssynchrony.5 However, the value of QRS duration to predict response to CRT remains still controversial and in parallel, a definition of dyssynchrony based on LV mechanics has been proposed in order to better understand LV dyssynchrony and to identify potential responders to CRT.6 Accordingly, several imaging techniques have emerged to identify LV mechanical dyssynchrony.7-11 Echocardiography, with techniques based on color tissue-Doppler imaging, is the method most commonly used for that purpose due to its high temporal resolution and ability to realidy analyze segmental motion. However, LV mechanical dyssynchrony analyzed with tissue Doppler imaging is derived from only 1-dimensional longitudinal motion data and limited by the Doppler angle of incidence.
Three-dimensional echocardiography provides a unique imaging technique to assess the whole LV volume simultaneously. Therefore, our aim was to evaluate the feasibility of real time 3-dimensional echocardiography (RT3DE) to assess the presence and distribution of LV mechanical dyssynchrony in different clinical settings as well as to detect changes in LV mechanical dyssynchrony after CRT.
METHODS
Study Population
A series of 60 subjects were prospectively studied. The study included 10 healthy volunteers and 50 patients with LV systolic dysfunction: 23 with myocardial infarction and 27 with dilated cardiomyopathy.
Healthy volunteers were recruited among a group of post-graduate university students without any remarkable medical history.
The group of patients with myocardial infarction included 23 patients with a first ST-segment elevation acute myocardial infarction. All of them were selected from among those admitted at the emergency department of our institution. Those patients in Killip class III-IV were excluded as well as those referred from other hospitals in which an early transfer to the hospital of origin did not allow following the scheduled imaging diagnostic tests. Diagnosis of ST-segment elevation acute myocardial infarction was made on the basis of prolonged ischemic chest pain, an ST-segment elevation above 0.2 mV in at least 2 contiguous leads and cardiac enzyme abnormalities. All of them underwent percutaneous coronary intervention and were scanned with both 2-dimensional echocardiography and RT-3DE within the first 48 hours from hospital admission.
The group of patients with dilated cardiomyopathy comprised 27 patients scheduled for CRT. All of them fulfilled the criteria for CRT: LV ejection fraction ≤35%, QRS duration ≥120 ms on the surface electrocardiogram and New York Heart Association functional class III-IV.5 The RT3DE studies in the dilated cardiomyopathy patients were performed before and 24-48 hours after CRT device implantation and the study was repeated at 6-month follow-up.
The ethics committee at our institution approved the protocol, and all patients gave written consent.
Transthoracic 2-Dimensional Echocardiography
The overall study population underwent transthoracic 2-dimensional echocardiography evaluation. Patients were imaged in the left lateral decubitus position using commercially available equipment (Vingmed Vivid-7, General Electric Vingmed, Milwaukee, Wisconsin, USA; SONOS 7500, Philips, Andover, Massachusetts). Data acquisition was performed with a 3-3.5-MHz transducer at a depth of 16 cm and standard gray-scale images were obtained during breath hold and stored in cineloop format from 3 consecutive beats. Left ventricular end-diastolic volume and end-systolic volume were derived; the LV ejection fraction was calculated from the apical 2- and 4-chamber views using the Simpson's rule.12
Assessment of LV Mechanical Dyssynchrony by Tissue Doppler Imaging
In patients with dilated cardiomyopathy color-tissue Doppler echocardiography was performed to assess LV mechanical dyssynchrony, following the study protocol of our institution for these patients. Data acquisition was performed with a mean color Doppler frame rate of 128 fps (range, 120-148 fps) depending on the sector width of the region of interest. The tissue Doppler-based parameters were measured from 4-chamber apical views images of 2 consecutive heart beats by offline analyses. Data were analyzed using commercially available software (Echopac 6.1, General Electric-Vingmed). Peak systolic velocities were determined at the basal portion of the septum and the lateral wall, and LV mechanical dyssynchrony was defined as the time delay between both peak systolic velocities, as previously described.13
Transthoracic Real Time 3-Dimensional Echocardiography
Real time 3-dimensional echocardiography was performed using a commercially available ultrasound scanner equipped with the x4 matrix array transducer (SONOS 7500, Philips, Andover, Massachusetts). Dedicated software incorporated in the system enabled the acquisition of 4 small real-time subvolumes from alternate cardiac cycles. Subsequently, a pyramidal volume was obtained from the complete capture of the LV. The 3-dimensional studies were considered unsuitable for analysis if >2 segments could not be visualized or if contained visible translation artifacts.
Apical full volumes of the LV were obtained in all patients. For further optimization of the frame rate of acquisition, depth was minimized to include only the whole LV. The mean frame rate used was 19 (3) fps.
The RT3DE raw data were digitally stored and transferred to a separate workstation. The off-line analysis was performed using commercially available software (Qlab, version 4.0, Philips). The quantification of LV 3-dimensional volumes and ejection fraction were performed as follows: after definition of the long-axis of the LV, the mitral valve annulus and LV apex were determined with 5 points at the end-diastolic and end-systolic frames. A semiautomatic algorithm subsequently used these points for automatic detection of the endocardial border. A cast of the LV cavity was then created following a mathematical model, providing time-volume data for the entire cardiac cycle. Finally, this volume was divided and analyzed according to the 17-segmental volume. The accuracy of RT3DE to quantify LV volume and ejection fraction has been compared to magnetic resonance in our laboratory, showing an excellent correlation despite a slight underestimation of the 3 parameters (r=0.83 and mean difference, -14.2 [9.2] mL for LV end-diastolic volume; r=0.81 and -6.9 [7.9] mL for LV end-systolic volume; and r=0.8 and -1.0 % [2.7 %] for LV ejection fraction).
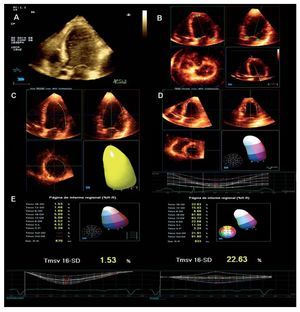
Index to Quantify LV Mechanical Dyssynchrony by RT3DE
Once the full volume of the LV was constructed, changes in segmental LV volumes along the entire cardiac cycle were analyzed to obtain the systolic dyssynchrony index (SDI) (Figure 1). The 3-dimensional software displayed the volume-time curves for the 17 segments in which the LV volume was divided. To obtain the SDI, the standard deviation of the times taken to reach the minimum regional volume for 16 segments (excluding the true apex) was calculated. Finally, the SDI was expressed as a percentage of the duration of the cardiac cycle. Higher SDI identified therefore, those patients with more pronounced LV mechanical dyssynchrony.
Figure 1. Assessment of LV mechanical dyssynchrony by RT3DE. The assessment of LV mechanical dyssynchrony by real-time 3D echocardiography can be summarized as follows: A: acquisition of full LV volume by ECG gating. B: the acquired LV volume is cropped to obtain a real long axis of the LV and to define the mitral valve annulus and LV apex with 5 points (green stars). C: from these 5 referral points, semiautomatic endocardial border detection provides a mould of the LV cavity at end-diastole and end-systole. D: by dividing the volume obtained into 17 pyramidal subvolumes an estimation of time-volume changes for each of the LV segments can be defined. The standard deviation of the times taken to reach the minimum regional volume for 16 segments (the apical segment is excluded from the analysis) provides the systolic dyssynchrony index (SDI) expressed in percentage. E: in the panel on the right, time-volume curves of a patient with dilated cardiomyopathy demonstrating the dispersion of time to reach minimum volume for the different LV segments, with a consequently high SDI value. Conversely, in the left panel, time-volume curves of a healthy volunteer with small dispersion and lower SDI value.
Distribution of LV Mechanical Dyssynchrony
The volume-time curves provided by 3D software allowed for the identification of the more delayed LV segments attaining the minimum systolic volume. In addition, we sought to find the most delayed segments to characterize the distribution of LV mechanical dyssynchrony by analysis of volume-time curves in the overall study population.
Changes in LV Mechanical Dyssynchrony After CRT
In the group of patients with dilated cardiomyopathy, changes in SDI were evaluated before and at 24-48h and 6-month follow-up after CRT. Furthermore, LV remodeling was evaluated and a reduction in LV endsystolic volume ≥10% was used as criterion for response to CRT.14
Statistical Analysis
Continuous variables were expressed as mean (SD), whereas qualitative variables were expressed as number and percentage. One-way analysis of variance test followed by post hoc Bonferroni test was used to compare LV volumes, ejection fraction, and SDI among the 3 subgroups previously defined. In addition, in the group of patients with dilated cardiomyopathy, LV volumes, ejection fraction, and SDI were compared during follow-up by the 2-tailed Student t test for paired data.
Furthermore, the agreement between the presence /absence of LV mechanical dyssynchrony on tissue Doppler imaging and RT3DE was expressed as percentage with the corresponding k value. With tissue Doppler imaging, LV mechanical dyssynchrony was defined as a septal-to-lateral wall delay ≥60 ms.13 Definition of LV mechanical dyssynchrony with RT3DE was set with an arbitrary cut-off value calculated as the mean + 3SD of the SDI value found in the healthy population of the present study, similar to what other authors have previously described.15
Finally, reproducibility of SDI measurements was studied by repeated measurements of 2 observers; both intra and interobserver variability were analyzed using the Bland-Altman method. Additionally, intraclass correlation coefficient for inter- and intraobserver comparisons was calculated. A P value less than .05 was considered significant. All data were analyzed using the SPSS version 12.0 statistical package (SPDD, Inc., Chicago, Illinois).
RESULTS
Patients Characteristics
Out of 60 patients who underwent RT3DE, 54 (90%) had suitable acoustic windows to be further assessed. Excluded patients belonged to the subgroups of patients with acute myocardial infarction (n=1) and dilated cardiomyopathy (n=5).
Healthy volunteers (n=10; mean age, 25 (6) years old; 50% men) showed a QRS duration on surface electrocardiogram <120 ms (mean, 85 [3] ms). In addition, echocardiography exams were normal and ruled out valve disease or any other cardiomyopathy.
A total of 22 patients with acute myocardial infarction were finally studied (mean age, 57 [13] years old; 86% men [n=19]). Localization of the acute myocardial infarction was anterior in 11 patients and inferoposterior in the other 11. Mean QRS duration was 96 (6) ms, and none of them showed left or right bundle branch block. Mean time from the onset chest pain to reperfusion was 4 (3) hours. Mean value of biomarkers reached was 2064 (1385) U/L for creatin-kinase and 108 (107) ng/dL for troponin I.
The group of patients with dilated cardiomyopathy comprised 22 patients (mean age, 72 [8] years old; 77% men [n=17]). The etiology of the cardiomyopathy was ischemic in 9 patients and idiopathic in the remaining 13 patients. All patients in this group had a QRS duration ≥120 ms (mean, 160 [20] ms) with left bundle branch block morphology.
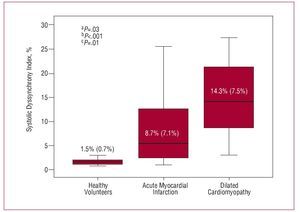
Assessment of LV Volumes, Systolic Function, and LV Mechanical Dyssynchrony by RT3DE
Table 1 shows the left ventricular parameters measured by RT3DE. Patients with dilated cardiomyopathy showed significantly larger LV volumes and lower ejection fraction compared to patients with acute myocardial infarction and healthy volunteers. Patients with ischemic dilated cardiomyopathy (n=9) showed comparable baseline characteristics to patients with idiopathic dilated cardiomyopathy (n=11) (LV end-diastolic volume, 226 [100] mL vs 195 [82] mL, P=NS; LV end-systolic volume, 173 [100] mL vs 150 [71] mL, P=NS; LV ejection fraction. 27% [8%] vs 26% [8%], P=NS; SDI, 12.9% [7.5%] vs 15.3% [7.7%], P=NS). Importantly, SDI was also significantly higher in patients with dilated cardiomyopathy compared to the other 2 subgroups: 14.3% (7.5%) versus 8.1% (7.1%) in patients with acute myocardial infarction and 1.5% (0.7%) in healthy volunteers (P<.0001) (Figure 2).
Figure 2. Systolic dyssynchrony indices in the 3 different groups of patients. Patients with dilated cardiomyopathy showed statistically significant higher value of systolic dyssynchrony index when compared with those patients with ST-segment acute myocardial infraction and healthy volunteers. aHealthy volunteers versus acute myocardial infarction patients. bHealthy volunteers versus dilated cardiomyopathy patients.cAcute myocardial infarction patients versus dilated cardiomyopathy patients.
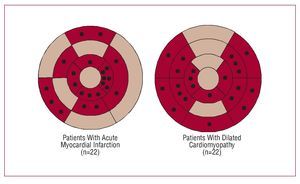
Distribution of LV Mechanical Dyssynchrony Assessed by RT3DE
Among patients with acute myocardial infarction the most delayed segments were more frequently located at the apical and mid segments of the LV, in concordance with the segmental wall motion abnormality (localized area of hypo/akinesis induced by the acute myocardial infarction).
In patients with dilated cardiomyopathy, who had more globally hypokinetic LV with diffuse motion abnormalities, the most delayed LV segments were more frequently located at the basal and mid-levels of the infero-posterior LV segments (Figure 3).
Figure 3. Bullseye views of delayed LV segments in 2 different groups of patients. Each black point denotes the most delayed LV segment for each of the studied patients. Patients with ST-segment acute myocardial infarction had delayed segments more frequently located at the apical and mid portion of the LV whereas patients with dilated cardiomyopathy had delayed segments more frequently located at the base of the LV.
Effect of CRT on SDI
Acute changes in LV volumes, ejection fraction, and SDI could be assessed in all patients with dilated cardiomyopathy (n=22). At 6-month follow-up, changes in these parameters could be assessed in 11 patients.
At 24-48h after implantation of CRT in the patients with dilated cardiomyopathy, RT3DE demonstrated a significant reduction of LV end-systolic volume with a significant improvement in the ejection fraction and synchronicity of the LV (Table 2). At 6-month follow-up, the improvement observed in LV ejection fraction with the concomitant reduction of SDI was sustained in the studied patients (Table 2).
Those patients who showed a decrease in LV endsystolic volume ≥10% were considered responders to CRT. Accordingly, there were 10 patients (45%) who showed acute response to CRT. Out of 11 patients who completed 6-month follow-up, 5 patients (45%) showed LV reverse remodeling. At baseline, responder patients had a SDI value slightly higher than non-responder patients albeit this difference was not statistically significant (16.4% [8.4%] vs 12.6% [6.5%]; P=.2).
Concordance Between Tissue Doppler Imaging and RT3DE for LV Mechanical Dyssynchrony Assessment
In the group of patients with dilated cardiomyopathy, LV mechanical dyssynchrony was also evaluated by color-tissue Doppler imaging. By this method, LV mechanical dyssynchrony was defined as a septal-to-lateral wall delay ≥60 ms, as previously described.13 In the patients with dilated cardiomyopathy, mean septal-to-lateral time delay assessed by color-tissue Doppler imaging was 57 (37) ms. Additionally, as LV mechanical dyssynchrony was evaluated by RT3DE, the cut-off value used to define LV mechanical dyssynchrony was defined arbitraryily as the mean + 3SD of the SDI value found in the healthy population of the present study (SDI=4%). The concordance between color-tissue Doppler imaging and RT3DE was analyzed, and in 10 patients (45%), both methods detected substantial LV mechanical dyssynchrony, whereas in 6 patients (27%) both methods indicated the absence of LV mechanical dyssynchrony. Therefore, the agreement between the 2 techniques for defining LV mechanical dyssynchrony was 72% (k=0.5, P=.02).
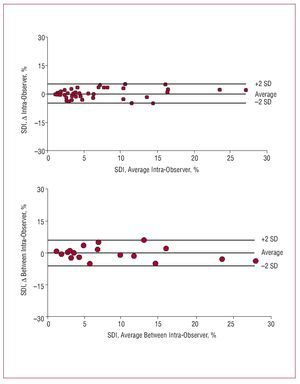
Reproducibility of SDI
RT3DE scans of 18 random patients were re-analyzed for intra- and inter-observer reproducibility evaluation for SDI measurement. Measurements of SDI were performed twice on separate days by the same observer for intraobserver variability assessment; additionally, a second blinded observer also performed the measurements for the interobserver variability. The intraobserver reproducibility was good, with an average difference of 0.02 (2.5%) between repeated measurements from the same observer (Figure 4). Similarly, agreement of measurements made by two different observers was good, with an average difference of 0.38 (3.2%) (Figure 4). The intraclass correlation coeficient for intra- and interobserver comparisons were 0.97 and 0.96 respectively (P<.001).
Figure 4. Bland-Altman plots for intra and inter-observer variability. SDI indicates systolic dyssynchrony index.
DISCUSSION
The present study demonstrates the feasibility of RT3DE for the assessment of LV mechanical dyssynchrony in a broad spectrum of patients. In patients with dysynchronous LV contraction due to either a localized akinesis (acute myocardial infarction patients) or global LV dysfunction and conduction abnormality (patients with dilated cardiomypathy with left bundle branch block), the SDI was significantly higher as compared to normal healthy volunteers. Moreover, in those patients with dilated cardiomyopathy who received CRT this index significantly improved both in the acute and mid-term follow-up. Therefore, the index appears to closely reflect different degrees of cardiac synchronicity corresponding to the different clinical settings evaluated.
Evaluation of LV Mechanical Dyssynchony by RT3DE
Previous studies have demonstrated the usefulness of 3-dimensional echocardiography to assess LV mechanical dyssynchrony in different groups of patients.15,16 Kapetanakis et al,15 by using a different 4-dimension LV postprocessing software, analyzed LV synchrony in a large population with various degrees of LV systolic function.15 The authors found a relation between SDI and LV ejection fraction and the more depressed ejection fraction resulted in higher SDI value.15 In contrast, QRS duration showed a weak relation with the SDI.15 These results were also corroborated by Park et al16 in a recent study, where LV mechanical was evaluated by RT3DE in 23 patients with advanced heart failure and compared to 16 normal controls.16 The mean value of SDI observed was significantly higher in patients with heart failure than in controls (7.7% [2.5%] vs 1.5% [1.0%]; P<.01).16 Finally, Marsan et al,17 by using RT3DE and the same postprocessing algorithm as the current study, assessed the LV mechanical dyssynchrony in a group of heart failure patients scheduled for CRT. The authors observed a baseline SDI mean value of 7.3% (4.6%) for the overall population with a SDI cut-off value to define LV mechanical dyssynchrony of 5.6%.17 Our results are in line with these previous studies and importantly, the obtained SDI cut-off value to define LV mechanical dyssynchrony (4%) was similar to the SDI value observed by them (5.6%). Therefore, the present study adds more evidence on the clinical utility of RT3DE among patients with heart failure who may benefit from LV mechanical dyssynchrony assessment and treatment with CRT.11,18,19
Distribution of LV Mechanical Dyssynchrony
In our study we found that LV mechanical dyssynchrony had a different distribution and pattern according to the underlying cardiomyopathy. Therefore, in the acute ischemic setting, the dyssynchrony more involved frequently the apical segments, in relation to the infarcted areas. On the other hand, in patients with dilated cardiomyopathy, where LV motion abnormalities are commonly diffuse, the dyssynchronous segments were usually located at the basal and mid LV levels. These findings may suggest that a delayed segment cannot only be delayed, but also infarcted. By assessing asynchrony with myocardial velocity imaging or volumetric changes such as we did in our study, an akinetic segment can be passively moved by the active contraction of the adjacent segments. This may underscore the importance of studying the viability of those delayed segments prior to CRT implantation.20,21
On the other hand, in line with previous studies, we observed that the most delayed myocardial segments in patients with dilated cardiomyopathy tended to be more frequently located in the infero-postero-lateral walls of the LV.22,23 RT3DE could offer a noninvasive approach to identify the most delayed areas where the third lead would have to be placed.
LV Mechanical Dyssynchrony Assessment With RT3DE and Other Methods
In this study we have found that LV mechanical dyssynchrony is independent of the duration of the QRS in concordance to what other authors have also reported.6,24 In acute myocardial infarction patients, all of them with a QRS duration <120 ms, SDI was higher than in healthy volunteers. We found a moderate agreement between tissue Doppler-derived LV dyssynchrony index and SDI. The comparison was performed only in those patients treated with dilated cardiomyopathy and wide QRS (left bundle branch block) undergoing CRT who showed more dyssynchrony at the basal level of the lateral and septal ventricular segments which can be easily analyzed with tissue-Doppler. However, the agreement would have been probably lower in a wider group of patients including those with myocardial infarction in whom the apical segments were more dyssynchronous and therefore, not suitable to be studied with Tissue Doppler.25
Study of LV Mechanical Dyssynchrony Changes Induced by CRT
In the patients with dilated cardiomyopathy who received CRT, LV mechanical dyssynchrony was evaluated prospectively by RT3DE. Data about the effect of CRT on LV mechanical dyssynchrony assessed with RT3DE are scarce.15,26 Zhang et al26 demonstrated in 13 heart failure patients treated with CRT an acute changes in LV synchronicity.26 With the CRT device activated, the RT3DE-derived LV mechanical dyssynchrony parameters used were significantly lower than with the withdrawal of the biventricular pacing.26 Furthermore, acute changes in LV volumes and ejection fraction were also reported, with an improvement in LV performance with the CRT activated.26 These results are in line with the findings of the present study. An acute improvement in LV systolic function and a reduction in LV volumes were observed together with a decrease in SDI. In those patients who completed the 6-month follow-up, the beneficial effects of CRT on LV performance and synchrony were sustained. However, neither in the present study nor in the previous studies could a cut-off value for SDI to predict long term response to CRT be reported.15,26
Study Limitations
Despite technological advances, RT3DE still has limited applicability in patients with difficult acoustic windows. In our case, 6 from 60 patients had to be excluded for analysis due to bad quality images, which yields a feasibility rate around 90%. Another limitation that should be taken into account is the low frame rate of the acquired data. However, despite this technical limitation, the reproducibility of the measurements was good in the present study.
We could not demonstrate a cut-off value in patients with dilated cardiomyopathy from which mid-long-term response to CRT could be predicted. Indeed, this was not the aim of the present study. The small number of studied patients in whom CRT was implanted (n=22) and who finished the 6-month follow-up (50%) preclude from any strong conclusion regarding this issue in the present study. However among those patients who did not showed response to CRT after 6 months of follow-up, mean SDI value showed a tendency to be lower than those who responded. This finding is consistent with previous studies showing that, regardless the dyssynchrony parameter used to predict response, those with less dyssynchrony were often non-responders.19,27-29
CONCLUSIONS
RT3DE is a feasible echocardiographic method to assess and quantify LV mechanical dyssynchrony. In those patients with severe symptomatic heart failure despite optimal medical treatment, RT3DE could be a useful tool for identifying dyssynchrony amenable to be corrected with CRT.
ABBREVIATIONS
CRT: cardiac resynchronization therapy
LV: left ventricle/ventricular
RT3DE: real time 3-dimensional echocardiography
SDI: systolic dyssynchrony index
SEE EDITORIAL ON PAGES 800-2
Funding: Victoria Delgado, Jose Maria Tolosana, and Bàrbara Vidal, were supported by a post-residency award from Fundació Clínic and a grant from the Sociedad Española de Cardiología. The study was supported in part by a Research grant from the Sociedad Española de Cardiología 2006, Fondo de Investigaciones Sanitarias FIS PI 05/0118, and from the Technological Development Centre (CDTI) under the CENIT Programme from the Ministerio de Industria of Spain (CD-TEAM project).
Correspondence:
Dra. M. Sitges.
Servicio de Cardiología. Instituto Clínico del Tórax. Hospital Clínic. Villarroel, 170. 08036 Barcelona. España.
E-mail: msitges@clinic.ub.es
Received January 17, 2008.
Accepted for publication April 9, 2008.