Keywords
INTRODUCTION
Heart failure (HF) is common in the general population and its prevalence can reach 8%-17% in people over 70.1 This elderly population is characterized by having a high degree of fragility and dependence from the physical, cognitive, and psychological points of view. Even younger people with HF may show a high degree of fragility and dependence. Fragility is not a well-defined clinical entity. It might represent a complex sum of several conditions characterized by the interaction of physical, psychological, and social impairment. We previously reported a high prevalence of fragility and depressive symptoms (one of the main components of fragility) in HF patients, with age and gender differences.2 The prognostic role of fragility in HF has not been comprehensively studied. Fragility might be important in HF patients because it probably makes treatment more difficult (more adverse effects, less tolerability, less adherence, etc) and it can predispose to readmissions.
The aim of our present study was to ascertain whether fragility and depressive symptoms detected during the first visit to the unit were related with 1-year mortality and with the need for HF hospital admission during the first year of follow-up.
METHODS
Patients
All patients referred to the HF unit were consecutively included. There were no exclusion criteria. Our HF unit is a multidisciplinary one where patients with HF of any etiology are admitted independently of the left ventricular function, although the majority of our patients have left ventricular dysfunction. Once they were admitted to the unit, patients were visited by the nurse at least every 3 months and by doctors every 6 months, and as many times as needed depending on their clinical situation. When one patient did not attend the scheduled visit, information about hospital admissions and vital status were obtained by telephone call, revision of hospital chart and laboratory and emergency department data, and finally, if necessary, official social security administration data base.
Instruments
As mentioned, fragility is not a well-defined clinical entity. The definition of fragility used in this study had previously been published.2 In summary, during their first visit to the unit all patients prospectively underwent a basic geriatric evaluation by the nurse, that should permit detection of possible loss of autonomy for carrying out basic and instrumental activities, cognitive deterioration, emotional disturbance, or social risk. This evaluation consisted of several tests and the use of standardized geriatric scales:
- Barthel Index3: evaluates patients' dependence for basic activities of daily living (range, 0-100)
- OARS Scale4: evaluates their autonomy in instrumental activities of daily living (range, 0-14)
- The Pfeiffer Test5 was the instrument selected to evaluate their cognitive function (range, 0-10)
- A Yesavage abbreviated geriatric depression scale (GDS) was used to identify possible emotional problems6
- A basic social interview
Patients fulfilling predefined criteria (Barthel <90; OARS score <10 in women and <6 in men; Pfeiffer Test score >3 [1] depending on educational level; a positive depression response on abbreviated GDS [1 positive response out of 4 questions]; and nobody to turn to for help) were considered to be frail for purposes of the study, although strictly speaking some could be considered more disabled than frail. OARS score was considered differently for men and women owing to the existence of marked cultural and environmental differences.
Quality of life was evaluated with the Minnesota Living With Heart Failure Questionnaire (MLWHFQ) during the first visit to the unit. Higher scores signify worse quality of life. Compliance with treatment and health recommendations were assessed using a nursing questionnaire as reported elsewhere.7 For the purpose of the current study, adherence to treatment and a low-salt diet, weight and blood pressure controls, daily exercise performance, and smoking and drinking habits were considered. All the questionnaires, scales and tests were recorded with the aid of the nurse. Only MLWHFQ was recorded without aid by various (most needed help from the nurse).
Endpoints
After a follow-up of 1 year for every patient, 1-year mortality, and the need for HF related hospital admission (primary cause of admission) were recorded and their relationship with fragility and depressive symptoms was analyzed.
Statistics
Statistical analysis was performed using the SPSS 11.0 package for Windows. Two-sided P<.05 was required for statistical significance. The c2 test was used for the main purpose of the study (fragility and depressive symptoms) and score comparison of MLWHFQ was made using the Kruskal-Wallis test owing to the non-normal distribution of scores. Two multivariate Cox regression analysis (enter method) were performed using 1-year mortality and need for HF hospitalization as dependent variables, and, as independent factors, age, gender, New York Heart Association (NYHA) functional class, left ventricular ejection fraction (LVEF), etiology, diabetes, time from HF symptoms onset, beta-blocker treatment, treatment with angiotensin converting enzyme inhibitors (ACEI) or angiotensin II receptor blockers (ARB), and fragility or depressive symptoms, to ascertain whether fragility and depressive symptoms were independently related to 1-year mortality and the need for HF hospitalization. Kaplan-Meier survival curves with log-rank statistical test were also performed.
The investigation conforms with the principles outlined in the Declaration of Helsinki (Br Med J 1964;ii:177). All patients gave verbal informed consent to participate in the study.
RESULTS
Six hundred and twenty-two patients (72.5% men; median age, 68 years) were analyzed. Demographic characteristics are shown in Table 1. Fragility was detected in 39.9% and depressive symptoms in 25.2% of patients, showing a different distribution in relation to age and gender of patients (Table 2).
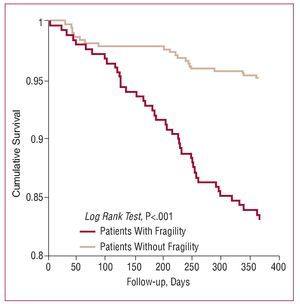
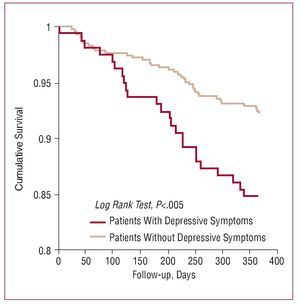
Sixty (9.5%) died during the first year of follow-up and 101 (16.2%) had heart failure hospitalizations. A statistical relationship was found between 1-year mortality and the presence of fragility: 16.9% in patients with fragility versus 4.8% in patients without fragility (P<.001). The higher mortality in frail patients was observed both in patients aged ≥70 (19.8% vs 7.5; P=.003) and in younger patients (12.5% vs 3.3%; P=.001). A statistical relationship was also found between 1-year mortality and the presence of depressive symptoms: 15.3% in patients with depressive symptoms versus 7.7% in patients without depressive symptoms (P=.006). A statistical relationship was also observed between the presence of fragility and the need for HF hospitalization: patients with fragility 20.5%, patients without fragility 13.3% (P=.01); however, no statistically-significant relationship was found between depressive symptoms and need for HF hospitalization: patients with depressive symptoms 19.1% versus 15.2% among patients without depressive symptoms (P=.26). Actuarial survival curves are shown in Figures 1 (fragility) and 2 (depressive symptoms). In Table 3 results on mortality and need for HF hospitalization according to the different parameters of fragility are shown.
Figure 1. Survival Kaplan-Meier curves for patients with and without fragility.
Figure 2. Survival Kaplan-Meier curves for patients with and without depressive symptoms.
Significant differences were found in the use of beta-blockers and ACEI or ARB among patients with and without fragility (63% vs 80%; P<.001; and 71% vs 81%; P=.002 respectively) and in those with or without depressive symptoms (67% vs 76%; P=.03; and 70% vs 80%, P=.01 respectively). However, no differences were found between patients with and without fragility or in those with or without depressive symptoms in any item when adherence to treatment and to a low-salt diet, frequency of weight and blood pressure controls, daily exercise performance, and smoking and drinking habits were evaluated.
In the multivariate Cox regression analysis, fragility showed an independent predictive value for mortality (Table 4), but not for HF hospitalization. Depressive symptoms did not prove to have an independent predictive value in the multivariate analysis.
As depicted in Table 5, when quality of life was evaluated, patients with fragility (P<.001) and depressive symptoms (P<.001) scored higher than patients without.
DISCUSSION
The incorporation of a geriatric specialist to an HF unit is based on the need to offer HF patients, many of whom are elderly, a global health problem assessment. This would permit wide treatment strategies, not only to address their heart disease, but also to maintain and improve their functional, cognitive, psychological, and social capacities.
Fragility is not a well-defined clinical entity. It might represent a complex sum of several conditions characterized by the interaction of physical, psychological, and social impairment and we must acknowledge that, strictly speaking, some of our patients could be considered more disabled than frail. As specific questionnaires to detect frail patients with HF are lacking we decided to use well known and validated geriatric scales. The cutoff points are either defined by the instrument (as is the Pfeiffer test and the abbreviated GDS), or clearly reveal a significant fragility in the explored area. We decided to evaluate all patients, not only elderly patients, as we suspected that younger patients may also suffer some degree of dependence and fragility, a fact we were able to confirm in our previous results on prevalence of fragility.2 In our current series, a significant proportion of patients under 70 fulfilled the pre-established criteria for fragility: 29.7% had difficulties in at least 1 of the explored areas.
Independently of dyspnea and fatigue, HF may cause disability through different mechanisms, such as skeletal muscle alterations8 and cognitive impairment— highly prevalent in HF9,10—, which actually hinder HF management, including pharmacotherapy introduction, diet and drug compliance and exercise performance. Furthermore, HF patients suffer from a significant number of co-morbidities which increase the difficulty of HF management11,12 and worsen the prognosis of HF patients.13 Treatment with beta-blockers and ACEI or ARB is crucial in patients with HF. In our study, although frail patients actually received those treatments in a lesser proportion than patients without fragility, in the multivariate analysis, that included such important treatments, fragility remained statistically associated with 1-year mortality. One recent study14 showed the predictive role of fragility in long-term mortality (12 years) in elderly subjects with chronic HF. In our study, frail patients showed a 3.5 times higher 1-year mortality than patients without fragility; the higher mortality in frail patients was also observed in elderly patients (≥70 years): 19.8% versus 7.5%, but even more clearly in younger patients: 12.5% versus 3.3%. A systematic functional assessment of HF patients becomes crucial for the early detection of such fragility and consequently for planning cardiac rehabilitation,15 not only to prevent disability16 but also to improve quality of life, considering that both actually have a great impact on mortality.17
Depression is common in patients with chronic HF18 and leads to more symptoms of heart failure, impaired quality of life and an increased risk of premature death. In our study, worse quality of life was significantly associated with fragility and depressive symptoms. The latter were detected in approximately 25% of patients, reaching almost 40% in women. The prevalence of depressive symptoms in our series is quite inferior to that observed by Guallar-Castillón et al19 using a 10 items GDS in elderly patients while they were hospitalized. Differences in the tool used (4 vs 10 items GDS) and also in the population studied (younger, ambulatory, and predominantly men [72.5%] in our series and more elderly, predominantly women [56.4%], and all studied during an hospitalization in the series of Guallar-Castillon et al19) can easily explain such differences. It is remarkable, however, that in our series depressive symptoms did not differ significantly between age groups. This finding suggests that depression in these patients is more related to HF itself or to HF mechanisms than to the patient's general circumstances (such as age, in this case). Several studies suggested a possible relationship between depression in HF patients and cardiovascular mechanisms, such as decrease in baro-receptor sensitivity or heart rate alterations,20 and immune system alterations and cytokine production.21 HF patients with depression also use more health care resources, thereby increasing health costs.22-24 We have no data on costs, and although our patients with depressive symptoms tended to need more hospitalizations during the first year of follow-up (19.1% vs 15.2%), the difference was not statistically significant.
Early detection of depression or simply depressive symptoms in HF is important. Several studies have shown that patients with depression have worse adherence to recommendations and to treatment, both in HF and in ischemic heart disease.25-26 Surprisingly, we found no differences in these aspects; nevertheless, our patients with depressive symptoms had significantly higher mortality than those without such symptoms (14.1% vs 5.8%). We actually expected to find differences in adherence and self-care behaviour among patients with and without depressive symptoms, but we did not. It is probable that the actual differences in treatment might have influenced prognosis, although the lesser use of beta-blockers and ACEI or ARB in patients with depressive symptoms had no a simple explanation. Other studies have also reported higher mortality in patients with depression.27-29 In a recently reported study, patients with a history of depression and lower education level showed worse outcome as early as 6 weeks of follow-up after being hospitalized for HF and/or chronic lung disease.30 However, studies that prove unmistakably a possible benefit of antidepressant treatment on HF outcome when mortality or hospital admissions are taken into account are still lacking. A recent report even suggested that patients receiving antidepressant treatment had worse outcome (death and HF hospitalization) than those not receiving this kind of treatment.31
Our results might support the implementation of multidisciplinary strategies for the assessment of fragility, although the benefits of a consequent specific intervention will require further studies.
Limitations
Although our population is a general one treated at an HF unit, we cannot rule out a possible bias of patients most of whom were referred from the cardiology department, were relatively young, had predominantly ischemic etiology, and men outnumbered women; consequently, our patients do not necessarily represent the whole population with HF. The definition of fragility used in this study is based in our previous work and has not been compared with other possible definitions of fragility. The study only took into account hospital admissions for HF; however, it was difficult to confirm the reason for admission if no report was available. Nevertheless, relatively few patients (<5%) did not have an admission report. Neither did we analyze admissions to the emergency room alone. Such admissions would have been difficult to count and check since information was often lacking. Finally, although the same nurse conducted approximately 85%-90% of the questionnaires, avoidance of some subjectivity differences in data collection is impossible.
CONCLUSIONS
Fragility and depressive symptoms are common in patients with HF, even in younger patients. Fragility and depressive symptoms showed significant relationship with 1-year mortality in the univariate analysis and fragility was also related to the need for HF hospitalization. However, only the prognostic predictive value of fragility for mortality was independent of other strong variables.
ACKNOWLEDGEMENTS
The authors thank Miss Christine O'Hara for help with the English version of the manuscript.
ABBREVIATIONS
ACE: angiotensin-converting enzyme
ARB: angiotensin-II receptor blocker GDS: geriatric depression scale
HF: heart failure
LVEF: left ventricular ejection fraction
MLWHFQ: Minnesota Living With Heart Failure Questionnaire
NYHA: New York Heart Association
Correspondence:
Dr. J. Lupón.
Unitat d'Insuficiència Cardíaca. Servei de Cardiología. Hospital Universitari Germans Trias i Pujol. Ctra. del Canyet, s/n. 08916 Badalona. Barcelona. España.
E-mail: jlupon.germanstrias@gencat.cat
Received January 1, 2008.
Accepted for publication March 4, 2008.