To the Editor,
Takayasu disease is a chronic idiopathic inflammatory vasculitis of the elastic arteries that results in occlusive or ectatic changes, mainly in the aorta and its branches.1
A 35-year-old woman consulted for chest pain. Her history included hypercholesterolemia, migraine, iron deficiency anemia, benign elevated intracranial pressure diagnosed 3 years previously (by magnetic resonance angiography that showed occlusion of the left common carotid artery), and grade IV retinopathy. She was not under treatment and reported no symptoms of rheumatic disease.
The patient came to our emergency room for oppressive precordial pain starting 24 hours earlier, accompanied by occipital headache, which ceased after sublingual nitroglycerin. The physical examination revealed blood pressure of 246/114 mm Hg in the right arm and 144/102 mm Hg in the left, right carotid and pansystolic cardiac bruit radiating to the back, with enhancement of the second sound, as well as abdominal bruit. The peripheral pulses were preserved and symmetric; perfusion and trophism in the acral areas was normal.
Both the ECG and the transthoracic echocardiogram showed left ventricular hypertrophy. Computed angiotomography, performed to investigate a suspected acute aortic syndrome, showed marked atheromatous disease with soft, calcified plaques over the entire thoracic aorta, but no aortic dissection, coarctation, or pseudocoarctation. There were no coronary abnormalities, and markers of myocardial injury were not elevated.
The subsequent laboratory workup showed total cholesterol, 215 mg/dL (normal, 80-200); HDL-C, 47 mg/dL (50-100); LDL-C, 150 mg/dL; triglycerides, 89 mg/dL (50-150); C-reactive protein, 7.2 mg/L (normal <5); and erythrocyte sedimentation rate, 2. All other results were normal, including assessments of adrenal hormones and the renin-angiotensinaldosterone axis.
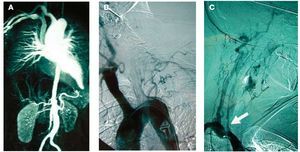
Doppler ultrasound showed kidneys of normal size and signs of aortic atheromatous disease, with slower flow in both renal arteries, the celiac trunk, and the upper mesenteric artery. Magnetic resonance angiography showed minimal flow in the left common carotid artery, no flow in the homolateral subclavian artery, and narrowing of the aortic adrenal-renal segment to 12 mm (Figure 1A). Ultimately, arteriography revealed no flow in the left common carotid artery or ipsilateral subclavian artery (Figure 1B), significantly reduced flow in the right common carotid artery (Figure 1C, arrow), and compensation by the right vertebral artery of considerably enlarged diameter.
Figure 1. Initial diagnosis.
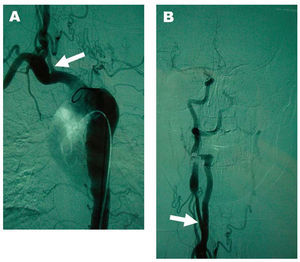
Treatment was initiated with 3 antihypertensive agents, statins, and acetylsalicylic acid, in addition to prednisone and methotrexate. After 6 months, blood pressure had returned to normal, there were no significant adverse effects, and the patient required only metoprolol for control. Follow-up arteriography 4 months after the diagnosis showed involution of the obstructive lesion in the right common carotid artery (Figure 2A and 2B, arrows).
Figure 2. Angiographic study at 4 months.
Takayasu arteritis, also known as Martorell-Fabré syndrome, was initially described in 1908. The incidence in Europe is 1 to 3 cases per million population, 80% to 90% in women.2 The diagnostic criteria most widely disseminated are those of the American College of Rheumatology3: a) age at disease onset <40 years; b) limb claudication; c) decreased pulse; d) blood pressure difference >10 mm Hg between the upper limbs; e) aortic or subclavian bruit; and f) stenosis or occlusion of the aorta or its branches not attributable to other causes. At least 3 criteria must be met to establish the diagnosis.
Our case describes a patient with Takayasu arteritis, with involvement of the supra-aortic trunks and the suprarenal and renal aorta, although without concomitant impaired renal function or neurological deficits. The reason for admission was grade 3 hypertension with a significant difference between the upper limbs, as well as chest pain, that we attributed to hemodynamic angina based on the normal coronary arteries seen in the angiotomography, the relatively rare involvement of these arteries,4 and the resolution of angina once blood pressure was controlled.
The clinical evolution after 6 months was favorable, with angiographic improvement of the lesions. This finding, although rare because of the chronic, progressive nature of the disease, has been described occasionally.5 For this reason, in view of the improvement in symptoms, interventional catheterization on the aortic and carotid lesions was ruled out.6