To the Editor,
Among several bleeding complications following platelet glycoprotein (GP) IIb/IIIa receptor inhibitors treatment, alveolar haemorrhage is often misidentified and confused with other respiratory syndromes. We would like to warn the physicians to keep in mind this fearful complication. The following case will help us in our explanation.
A 71-year-old woman presented with a chest pain. Six weeks ago, she had undergone a drug-eluting stenting of the left circumflex artery because of a non ST-elevation posterolateral myocardial infarction. Actually her electrocardiogram showed inferolateral ST-segment depression and significant increase of troponin I. Platelet count, coagulation profile, and chest x-ray was normal. The patient was treated with enoxaparin, aspirin, clopidogrel, B-blockers and tirofiban (0.4 µg/kg/min bolus and 0.1 µg/kg/min intravenous infusion), and scheduled for urgent percutaneous coronary intervention. An echocardiogram showed a left ventricular ejection fraction of 40 %, no valvular dysfunction, and normal pulmonary arterial pressures.
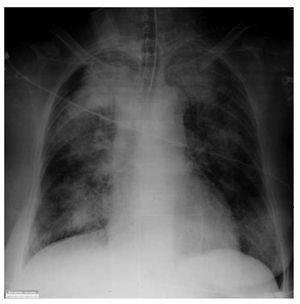
Two hours after tirofiban administration the patient became slightly dyspnoeic with low PaO2 levels. The urgent chest radiography showed widespread new alveolar shadowing (Figure).
Figure. 1. Urgent chest radiography showed widespread new alveoar shadowing, Patient developed a dense upper lobes consolidation and diffused consolidation in both sides.
She was treated with loop diuretics presuming left ventricular failure, but she became progressively hypoxic and hypotensive. Haemoglobin dropped from 12.2 g/dL on admission to 6.9g/L.
There was no haemoptysis, hematemesis, or evidence of intra abdominal bleeding by urgent echographic examination.
The patient required endotracheal intubation and mechanical ventilation support. During the manoeuvres of the lung intubation, large amount of bright red blood were seen in her airways. Immediate bronchoscopy was performed which revealed clotted blood filling the lobes of both lungs. No endobronchial lesions were evident. Stoppage of tirofiban, enoxaparin, and clopidogrel was performed. Blood transfusion was necessary. The coronary angiography was performed following clinical improvement, and documented intrastent thrombosis, treated with thrombus aspiration alone. Follow-up at 30-day was unremarkable.
This case report depicts a rare but potentially life-threatening complication of GP IIb/IIIa inhibitors use.1,2
In clinical trials, very few patients treated with these antiplatelet agents have experienced pulmonary blood loss. Nevertheless, this rate may be underestimated, primarily for under recognition of complication, especially if haemoptysis was not clearly evident. 3The misinterpretation may be due to the striking resemblance on chest x-ray with confounding syndromes, as well as pulmonary edema or pulmonary infiltrates.
For this reason, the number of patients in whom alveolar haemorrhage might have been incorrectly diagnosed is unknown.3,4
Moreover, the misdiagnosis may lead to inappropriate treatment with loop diuretics or antibiotic therapy for presumed heart failure or pneumonia.
Based on previous reports, an episode of spontaneous haemoptysis, or respiratory distress, or hypoxemia, associated with the evidence of new infiltrates on chest radiography in patients receiving GP IIb/IIIa inhibitors, should alert the physician about the potential development of pulmonary bleeding.4
Diagnostic flexible bronchoscopy must be considered early in this setting, because treatment is likely to be significantly improved if bleeding is identified quickly.
In previous reviews,4 it has been suggested that the presence of underlying lung disease, as well as chronic obstructive pulmonary disease, pulmonary
hypertension, and high pulmonary-capillary wedge pressure, may facilitate the risk of development of alveolar haemorrhage in patients treated with GP IIb/IIIa inhibitors, whereas others, believe that pulmonary disease does not necessarily define a subgroup of patients particularly at risk for this complication.
The unpredictable and potentially lethal course of pulmonary blood loss requires prompt identification, airway protection, and correction of coagulopathy.
Discontinuation of antiplatelet and anticoagulant agents and mechanical ventilation are the mainstay for the acute treatment of alveolar haemorrhage following GP IIb/IIIa inhibitors administration.2
The recognition of pulmonary alveolar haemorrhage requires a high degree of suspicion, particularly in patients presenting with dyspnoea, hypoxemia and/or chest radiographic abnormalities. Non specific symptoms and signs often delay or misidentify the diagnosis, thereby allowing fearful disease progression.5 The physicians should keep in mind this serious complication when they use antiplatelet GP IIb/IIIa inhibitors.