To the Editor:
At present, stent thromboses (ST) are relatively uncommon. Most occur within the first 24 hours (acute ST) or 1 to 30 days after implantation (subacute ST).1 In the case of bare-metal stents, late (>30 days) and very late (>1 year) thromboses are very rare. Drug-eluting stents considerably reduce restenosis and the need for new revascularizations2 and do not increase ST during the first year. However, drug-eluting stents appear to be associated with a slight increase (0.1%-0.2% per year) in the risk of very late ST.3
An association has been described between ST and stress testing, possibly as a result of increased platelet aggregation.4 This association has been described with bare-metal stents,5,6 but not drug-eluting stents, to our knowledge.
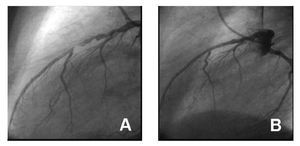
We describe a 56-year-old man with hypertension and dyslipidemia, former smoker, who presented an anterior myocardial infarction treated with thrombolysis. A year later, he had an anterior reinfarction, also treated by thrombolysis. Posterior coronary angiography showed severe stenosis in the middle-to-proximal left anterior descending artery. A Taxus stent of 2.75´28 mm (16 atm) was directly implanted and found to be successful on angiography (Figure 1). The patient was prescribed aspirin (indefinitely) and clopidogrel (1 year).
Figure 1. A: initial angiography. B: outcome after placement of Taxus stent.
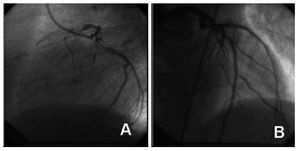
Angiographic follow-up at 8 months showed no restenosis. Fifteen months after stent implantation (3 months after clopidogrel was discontinued) with the patient asymptomatic, a symptom-limited stress test was performed with negative results. However, he presented chest pain 3 hours later that disappeared within 5 to 10 minutes; 8 hours later he presented persistent chest pain and went to the hospital after the first 2 hours of symptoms. Anterior reinfarction with criteria for reperfusion was documented and treated with thrombolytics. The patient presented pain and ST elevation again 3 days later, and was referred to our hospital for emergency coronary angiography, which showed complete thrombotic occlusion of the stent (Figure 2). He was treated by balloon dilation (3´20 mm), abciximab, and unfractionated heparin. Aspirin and clopidogrel were prescribed indefinitely. The patient was asymptomatic during the 5 months of follow-up.
Figure 2. A: stent occlusion. B: outcome of balloon angioplasty of the stent thrombosis.
Drug-eluting stents have substantially improved the medium-term and long-term results of percutaneous coronary revascularization by significantly reducing restenosis and the need for new revascularization. Randomized studies have shown a similar incidence of ST between both types of stents during the first year,2 although later studies indicate that at least the 2 FDA-approved drug-eluting stents (Cypher® [Cordis Corp.] and Taxus [Boston Sci.]) are associated with a slight increase in late ST (0.1%-0.2% per year).3
Some characteristics associated with ST are patient-related (ventricular dysfunction, acute coronary syndrome, heart failure, diabetes, renal failure, resistance to antiplatelet therapy), lesion-related (presence of thrombus, long lesions, calcium, small vessels, complete occlusions, bifurcations), and procedure-related (number, length, and diameter of stents, insufficient expansion of stent, residual dissection, initial TIMI flow <3, intracoronary brachytherapy).1 In the case of drug-eluting ST, other additional mechanisms have been proposed, such as poor stent positioning or even hypersensitivity to the polymer.
However, the most important predictor is early discontinuation of thienopyridines. Subacute5 and late6 stent thromboses have been described in relation to stress testing after the implantation of a bare-metal stent. A transient increase in platelet aggregation and the coagulation cascade during stress testing has been proposed as the main mechanism.4 Traditionally, stress testing has been contraindicated during the first month after the stent placement. The complication we describe (very late drug-eluting ST after stress testing) is probably very rare and, therefore, we do not believe that the indications and contraindications of stress testing depend on whether the patient was treated with a bare-metal or drug-eluting stent. Nevertheless, additional data on the safety of stress testing in patients treated with drug-eluting stents are probably needed.