To the Editor:
The use of intravenous immunoglobulin (IVIG) concomitant with platelet transfusion is indicated in patients with idiopathic thrombocytopenic purpura (ITP) in the case of life-threatening severe thrombocytopenia or hemorrhaging, or when therapeutic procedures with some risk of bleeding are performed.1
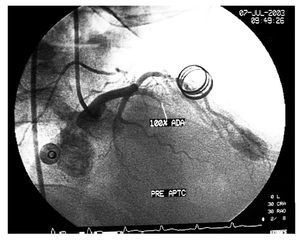
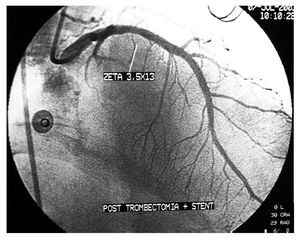
We describe a 44-year-old man with ITP who underwent a stress test for mixed angina attacks. Early positive results were obtained and, therefore, the patient also underwent coronary angiography. The thrombocyte count was 34 000/µL. The patient received 2 units of plasma and 6 of platelet concentrates before the procedure. An ulcerated thrombotic lesion in the proximal anterior descending artery was detected and treated by direct stenting with a drug-eluting stent. In addition, 8000 IU of intravenous heparin sodium and 300 mg of oral clopidogrel were administered; 3 hours later he was prescribed intravenous human immunoglobulin, 1 g/kg, for perfusion over 5 hours. This was repeated 24 hours later. Platelet count rose to 115 000/µL, and treatment with clopidogrel was started (75 mg/day); 5 days later, the patient presented precordial pain with ST elevation in the anterolateral aspect. Emergency coronary angiography showed complete thrombotic stent occlusion (Figure 1) that was treated by thrombectomy with an X-sizer and bare-metal stent (Figure 2). At discharge, oral anticoagulant therapy was prescribed and antiplatelet therapy was discontinued. The patient was asymptomatic 3 years later.
Figure 1. Coronary angiography shows total stent occlusion caused by a thrombus in the proximal segment of the left anterior descending artery.
Figure 2. Coronary angiography shows the result of acute occlusion treatment by revascularization, thrombectomy with an X-sizer, and implantation of a 3.5´13-mm multilink stent.
The purpose of treatment in ITP is to increase the platelet count to a safe, hemostatic range. Various treatments have been used effectively for this purpose.2 Despite the successful use of IGIV in patients with ITP who undergo coronary interventional procedures and present hemorrhagic problems,1 there are several published reports of acute myocardial infarction and stroke in relation to this condition. There may be a causal relationship between the administration of IVIG and the acute ischemic event,3 with this possibly related to the drug concentration and incidence of cardiovascular events.4
The management of hemostasis in patients with ITP who undergo PCI is not well established. The use of acetylsalicylic acid increases the risk of bleeding, although it has been used without complications in some cases with stent placement.5 The contraindication of clopidogrel is not defined.6
The prophylactic approach we used to prevent bleeding (indicated by the Hematology Department) was probably not the most adequate because the IVIGs were used 3 hours after the procedure, when the bleeding risk was lower, although it is true that clear recommendations in this regard have not been published.7 The placement of a drug-eluting stent may be criticized. However, the decision had been taken when the propensity of these devices to thrombosis, particularly late thrombosis, was less established. Furthermore, in our patient, the risk for dual antiplatelet therapy conditioned the choice of a bare-metal stent in the second procedure.
In patients with ITP who have undergone a percutaneous coronary intervention, IGIV should be administered only after careful consideration of the risks and benefits, and reserving it for patients at risk of severe hemorrhage, always considering the use of bare-metal stent over drug-eluting stent as the first option.