Keywords
INTRODUCTION
The value of exercise echocardiography (EE) in the prediction of death and myocardial infarction is well known.1,2 However, we have less information concerning its possible incremental value over resting or baseline echocardiography in patients with ventricular dysfunction, in particular when information on resting mitral regurgitation (MR) is available. Although MR can be assessed during EE,3-5 this is not a common practice, and only recently has the value of MR during exercise in the prediction of events in patients with ventricular dysfunction been stressed.6
The purpose of this study was to determine a) whether EE has incremental value over a resting Doppler echocardiographic study and b) whether immediate post-exercise MR increases the value of EE for predicting events in patients with left ventricular dysfunction.
METHODS
Patients
From a database including 2479 patients who underwent treadmill EE in our center over a period of 4.2 years, we selected those having a left ventricular ejection fraction (LVEF) less than 50%. Patients with organic MR, significant aortic valve disease or confirmed dilated or hypertrophic cardiomyopathy were excluded. The final group consisted of 388 patients (mean age, 64 [10] years; 312 men). We encountered mild resting ventricular dysfunction (LVEF between 40% and 49%) in 43% of the patients, while the dysfunction was moderate (LVEF between 30% and 40%) in 32% and severe (LVEF less than 30%) in 25%. According to their symptomatic status, 20 patients (5%) had typical angina, 166 (42%) had probable angina, 9 (2%) complained of noncardiac precordial pain and 22 (6%) presented dyspnea. The remainder of the patients (44%) were asymptomatic. The reasons for performing EE in the latter group included previous acute myocardial infarction (AMI), ventricular dysfunction in resting echocardiography and positive or nondiagnostic electrocardiogram (ECG) in a conventional exercise stress test. Table 1 shows the remainder of the clinical characteristics. Only 5% of the patients were taking beta-blockers at the time of EE since our usual practice is to discontinue them prior to the test.
Exercise Echocardiography
The heart rate, arterial pressure and resting ECG were assessed at each stage of exercise. The patients were encouraged to perform maximum exercise tests according to adjusted protocols (87% the Bruce protocol, 10% the modified Bruce protocol and 3% the Naughton protocol) to exhaustion or until they reached an endpoint. These endpoints included an ST depression or elevation of more than 2 mm, significant arrhythmia, severe hypertension (systolic arterial pressure over 240 mm Hg or diastolic arterial pressure over 110 mm Hg), hypotensive response (decrease greater than or equal to 20 mm Hg) or limiting symptoms. The ECG was considered to be positive in the case of elevation or horizontal or downsloping depression of the ST segment greater than or equal to 1 mm 80 ms after the J point, and was defined as nondiagnostic when the resting ECG was abnormal or when the patient was being treated with digoxin.
Two-dimensional echocardiography was performed at rest and at peak exercise, using fundamental or harmonic imaging in the standard views.7 Echocardiography at peak exercise was performed when the patient presented signs or symptoms of exhaustion or had reached one of the endpoints. The images were stored on disk for subsequent analysis.
Image Analysis
For analysis, the images were displayed on a digitized screen in quad format for comparison of the same views at rest and at peak exercise. Left ventricle was divided into 16 segments,8 each of which was assigned to each of the three coronary territories.9 The appearance of a new wall motion abnormalities (WMA) or deterioration of hypokinesia was considered to be an ischemic response. The persistence of a SMD involving at least one segment or deterioration of hypokinesia was considered to indicate necrosis, except in the case of hypokinesia of the posterobasal segment alone and that of septal hypokinesia in patients with complete left bundle branch block or pacemaker, or who had undergone recent surgery. In those cases, hypokinesia was considered to be normal. On the other hand, in patients with global ventricular dysfunction of unknown origin, progressive improvement was considered normal, suggesting a diagnosis of dilated cardiomyopathy.11 In the remaining patients, EE was defined as positive when ischemia or necrosis was observed in one coronary territory.12,13 We calculated a segmental motility index at rest and during exercise, in which normal motility had a score of 1, hypokinesia a score of 2, akinesia a score of 3 and dyskinesia a score of 4. The LVEF at baseline and during exercise were estimated visually14 by an observer.
Measurement of Mitral Regurgitation
The MR was measured by color Doppler in the 4-chambero apical view at baseline and in the immediate post-exercise period (within 30 seconds). The MR area was based on the total jet area, and was graded as mild (<4 cm2), moderate (4-8 cm2) or severe (>8 cm2), as has been described elsewhere.15 Mitral regurgitation was considered to be worse when there was an increase of at least one grade between resting and post-exercise MR. The interobserver and intraobserver variability in the determination of the grades of resting and exercise MR was determined in 30 patients, randomly selected from those with MR signals.
Follow-Up
The follow-up and determination of events was based on the review of clinical records and death certificates. We had access to the hospital admissions, outpatient visits and emergency services of all the SERGAS (Galician Health Service) centers, and none of the patients were lost to follow-up. As a last resort, when, at the end of the study, data corresponding to a given patient were missing, we checked the health care card database to determine whether the patient had died or moved out of the autonomic community of Galicia. In the first case, if the cause of death was unknown, the information concerning the death, as well as the exact cause (cardiovascular disease, neoplastic disease, etc), was obtained from the Death Registry of Galicia. Only serious events, defined as cardiac death and nonfatal AMI, were considered. Causes of cardiac death included sudden death, death preceded by an acute coronary event or heart failure, heart transplantation and appropriate defibrillator discharge; cardiac death was also considered in those cases in which the death certificate excluded noncardiac causes. Sudden death that could not be explained in any other way was considered to be of cardiac origin. Revascularization procedures performed during follow-up were recorded.
Statistical Analysis
The continuous variables are expressed as the mean ± 1 SD. The categorical variables are expressed as percentages, and the intergroup comparison was performed using the χ2 test. Event-free survival was estimated by means of the Kaplan-Meier method, using the time to first event method. The patients in whom the cause of death was a noncardiac event and those who underwent revascularization before an event occurred were censored at the time of death or of revascularization.
The univariate associations of the clinical variables, resting echo-Doppler, exercise stress test, EE, and post-exercise MR with hard events were measured using the Cox proportional hazards model. A P value of less than 0.1 was considered to be significant. The 95% confidence intervals (CI) and the hazard ratios (HR) are provided. The incremental value of EE over the clinical variables, resting echo-Doppler and the stress test was determined, as was the incremental value of MR over EE. The first step included clinical data, resting echo-Doppler and the stress test. In the second step, EE was introduced. Since different EE variables can express the same concept of deterioration of left ventricular function, the variable most closely related to the prognosis was identified by means of receiver operating characteristic (ROC) curves. The final step consisted of the post-exercise MR. We analyzed combined events (cardiac death plus nonfatal infarction), as well as cardiac death alone. The area under the ROC curve (AUC) values were estimated for each step of the multivariate analysis.
RESULTS
Exercise Echocardiography
The clinical data, ECG and hemodynamic variables during EE are shown in Table 2. The EE was considered to be normal in 69 patients (18%) and abnormal in 319 (82%). SMD were detected at rest in 244 patients (63%) and ischemia in 230 (59%). Of the latter patients, 158 (69%) also presented resting SMD. During exercise, single-vessel SMD was observed in 86 patients (22%), while 233 patients (60%) presented multivessel involvement. These disorders were detected in anterior descending artery in 293 patients (76%) and in the circumflex artery and/or right coronary artery in 251 (65%).
Variability in Mitral Regurgitation Measurements
The interobserver variability in the grading of resting and post-exercise MR was 3% (κ=0.94) and 10% (κ=0.83), respectively, whereas the intraobserver variability was 0% (κ=1.00) and 3% (κ=0.94), respectively.
Grading of Resting and Post-Exercise Mitral Regurgitation
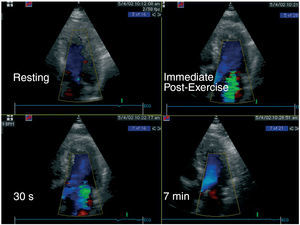
In all, 233 patients (60%) presented MR at rest, which was moderate or severe in 103 (27%), while MR was detected after exercise in 244 (63%), in 153 (39%) of whom, it was moderate or severe. The MR increased in 79 patients (20%), and was mild in 14, moderate in 52 and severe in 13. Most of these patients (n=48, 61%) had had mild MR at baseline, while 8 (10%) had had moderate resting MR and in 23 (29%), there was no evidence of MR prior to exercise. An example of a patient in whom MR had been exacerbated by exercise appears in Figure 1. Table 3 shows that the resting and post-exercise echocardiographic findings were more abnormal in the patients with increased MR than in those who presented no exacerbation.
Figure 1. Example of a patient with mild ventricular dysfunction (resting left ventricular ejection fraction [LVEF] 49%, exercise LVEF 46%) who developed severe mitral regurgitation (MR) during exercise. Top left: no evidence of MR at rest. Top right: severe MR detected in the immediate post-exercise period. Bottom left: the MR was similar 30 seconds later. Bottom right: 7 minutes later, the MR signal had disappeared.
Revascularization Procedure
During follow-up, 113 patients (29%) underwent revascularization (angioplasty was performed in 49 patients and surgery in 64). Of these patients, 109 who had undergone revascularization prior to some event were censored on the date of revascularization. As could be expected, the results of the stress tests were poorer in revascularized patients than in those who had not undergone this procedure, with a significantly higher prevalence of angina during the test (32% vs 12%, P<.0001), positive ECG (20% vs 7%, P<.0001), abnormal EE (91% vs 79%, P<.01), ischemia during EE (80% versus 52%, P<.0001), and multiterritory involvement (71% vs 56%, P<.001).
Events
Over a mean follow-up period of 2.1 (1.5) years (median, 2.0 years; maximum, 5 years), 61 serious events took place. Of these, 46 occurred prior to revascularization and were used to estimate event-free survival by means of the Kaplan-Meier method. The causes of these events were nonfatal AMI in 10 patients (25%) and cardiac death in 36 (75%). The causes of cardiac death were fatal AMI in four patients, exacerbation of heart failure in 4 and sudden death in 2. Out-of-hospital cardiac death was recorded in another 20 patients, once noncardiac causes were ruled on the basis of the death certificate. Heart transplantation in 2 patients and appropriate defibrillator discharge in four were also considered as deaths. Of the 46 events, 43 occurred in 319 patients in whom the results of EE were abnormal and 3 in the 69 patients with normal results (13% vs 4%, P=.04). Events were more frequent in patients in whom the resting MR had been graded as moderate or worse (19% vs 9%, P=.006), as well as in those with a moderate or poorer grade of post-exercise MR (19% vs 7%, P<.0001). The patients in whom MR had been exacerbated or was graded as moderate or worse after exercise suffered more events (19% vs 7%, P<.0001) and more cardiac deaths (16% vs 4%, P<.0001) than the remaining patients. The resting ejection fraction (a widely used prognostic index) was 37.3 (8.6) in patients who presented no events and 33.6 (7.8) in patients in whom events were recorded (P=.004), whereas the peak ejection fraction was 36.8 (10.7) versus 31.1 (9.1), respectively (P<.0001).
Predictors of Combined Events (Cardiac Death Plus Myocardial Infarction)
The variables that were significantly associated with risk of these combined events according to univariate analysis are shown in Table 4. The independent predictors were the resting MR (HR=1.3, 95% CI=1.1-1.4, P=.0001), peak double product (HR=0.91, 95% CI=0.86-0.96, P=.001) and the number of territories involved during EE (HR=1.6, 95% CI=1.2-2.1, P=.001; incremental value P=.001). The majority of the EE variables that proved to be significant in the univariate analysis were also of incremental prognostic value when introduced into the model in place of the number of territories involved: abnormal EE (P=.008), peak LVEF (P=.02), Δ LVEF (P=.01), peak segmental motility index (P=.01), multiterritory involvement (P=.003), SMD in anterior descending artery territory (P=.006), SMD in circumflex artery and/or right coronary artery territory (P=.004) and ischemia in circumflex artery and/or right coronary artery territory (P=.01). The inclusion of exacerbation of MR did not improve the prediction of combined events.
Predictors of Cardiac Death
The independent predictors were resting MR (HR=1.3, 95% CI=1.1-1.5, P=.002), peak double product (HR=0.89, 95% CI=0.84-0.96, P=.001), number of territories involved during EE (HR=1.6, 95% CI=1.1-2.3, P=.007, incremental value P=.001), and exacerbation of MR (HR=2.2, 95% CI=1.1-4.4, P=.04, incremental value P=.04). Figure 2 shows the survival rate according to the grade of MR at baseline. The survival rate according to the results of EE and to the presence or absence of exacerbation of MR appears in Figure 3. Figure 4 shows the ROC curves and the AUC values for the prediction of combined events and cardiac death at each step.
Figure 2. Kaplan-Meier survival curves in patients with no mitral regurgitation (MR) or with mild, moderate or severe MR at baseline. No MR versus mild MR, not significant; mild versus severe MR, P=.02; moderate versus severe MR, not significant. The survival rate was 94% in patients with no MR, 91% in patients with mild MR, 84% in patients with moderate MR and 69% in patients with severe MR.
Figure 3. Kaplan-Meier survival curves in patients classified according to the results of exercise echocardiography and the increase in mitral regurgitation (MR) during exercise. Negative test/no exacerbation of MR versus negative test/exacerbation of MR, not significant; negative test/no exacerbation of MR versus positive test/no exacerbation of MR, P=.03; negative test/no exacerbation of MR versus positive test/exacerbation of MR, P=.001; negative test/exacerbation of MR versus positive test/no exacerbation of MR, not significant; positive test/no exacerbation of MR versus positive test/exacerbation of MR, P=.04. The survival rate was 97% in patients with negative test and no exacerbation of MR, 100% in patients with negative test and exacerbation of MR, 91% in patients with positive test and no exacerbation of MR and 84% in those with positive test and exacerbation of MR.
Figure 4. Receiver operating characteristic (ROC) curves for each multivariate model for the prediction of a combined event (left) and of cardiac death (right). The area under the curve (AUC) values and 95% confidence intervals (CI) are provided. MR indicates mitral regurgitation.
DISCUSSION
The most relevant findings were that EE maintains its incremental value over resting echocardiography, even when the latter provides information on the resting MR, and that the exacerbation of MR increases the prognostic value of EE for the prediction of cardiac death in patients with ventricular dysfunction. These observations were made in a population in which there was a high prevalence of ischemic ventricular dysfunction (positive test results in 82% of the patients), and could be different in a population having other characteristics.
Mitral Regurgitation As a Predictor of Events
Mitral regurgitation has been shown to be a powerful predictor of cardiac death in patients with coronary artery disease.16,17 However, to the best of our knowledge, the value of the measurement of MR at baseline and during exercise for the prediction of events in patients with ventricular dysfunction has not been analyzed in large groups of patients. A recent study by Lancellotti et al,6 involving patients with ischemic ventricular dysfunction, reported that an increase in MR during exercise identified a subgroup at greater risk of events during follow-up, including death and hospital admission due to heart failure. However, since these findings were not compared with the results of EE, the incremental value of MR over EE could not be assessed. The exacerbation or development of MR, as measured by color Doppler, has been found to be associated with exercise-induced ventricular dysfunction, as well as with a greater extension of the coronary disease demonstrated by angiography.3,4 In the present study, we extended those results by showing that MR wor sening stratifies patients with ventricular dysfunction into different risk categories. However, as shown in Figure 3, an exacerbation of MR was of prognostic importance only in patients with abnormal EE, there being a rate of cardiac death of 16% among those with abnormal EE and increasing MR, versus 9% among those with abnormal EE in whom MR did not change. The relationship between exacerbation of MR and cardiac death could involve several mechanisms, such as increased MR during routine daily activities,6 chronic ventricular overload and progression of myocardial involvement.
Mitral Regurgitation During Stress
The feasibility of acquiring confident MR signal during stress has been previously demostrated.3,4 However, these measurements are not usually incorporated into conventional protocols. Our method consisted in the acquisition of echocardiographic images at peak exercise and color Doppler images immediately after exercise. Other researchers have employed supine bicycle exercise5,6,18 or dobutamine19 to measure the changes in MR during stress. While supine bicycle exercise appears to be an excellent method for measuring MR during stress, dobutamine-induced stress is not. Dobutamine produces a significant decrease in afterload and a positive inotropic effect that can reduce the regurgitant orifice and, thus, MR. Heinle et al19 found no association between an ischemic response to dobutamine and exacerbation of MR. Therefore, MR is not associated with ventricular dysfunction during dobutamine-induced ischemia.
Exercise Echocardiography
The incremental value of EE over other variables has been reported previously.1,2 In this study, we extend those findings, demonstrating that this incremental value is maintained when the grade of the resting MR is known.
Limitations
We performed peakinstead of post-exercise imaging because higher sensitivity has been demonstrated with the former.7,20 If we had employed the latter, the superiority of EE might have been underestimated. Likewise, post-exercise MR could have been underestimated if we had used the post-exercise period to acquire two-dimensional echocardiographic images because the severity of MR can diminish rapidly.
The measurement of MR by means of color Doppler is highly dependent on the technician and the apparatus, and can be affected by gain, the filters, the transducer frequency and the number of images per second, among other aspects.21 In the attempt to minimize these factors, the same settings were used both at baseline and after exercise. The intraobserver and interobserver variability in grading MR was less than 5% and 10%, respectively, similar to those obtained with dobutamine.19 Measurement of MR in a single view, as in the present study, may be simplistic as it only evaluates one jet direction. For this purpose, proximal isovelocity surface area (PISA) would be more precise. While this method would be applicable in supine bicycle exercise,5,6,18 it would not serve with the treadmill.
Given that the results of EE were utilized by the responsible center, the apparent prognastic value of EE may be underestimated since the majority of those patients with strongly positive tests who underwent revascularization might have suffered events if they had not been revascularized.
In most cases, the definition of nonfatal AMI was based on criteria applied prior to the availability of troponin. Thus, AMI likely represents infarctions with true entity. If we had based our evaluation on current, more sensitive criteria, we would have recorded more AMIs, but they would be of less entity.
The LVEF was estimated visually in most of the patients. Although this approach is suitable for clinical use,14 it may not be adequate for a research study. However, it corresponds to reality in the majority of laboratories. Our group reported an intraobserver variability in the visual determination of LVEF at rest and during exercise in patients with different degrees of ventricular function of 9% (9%) and of 10% (10%), respectively.2
Approximately 25% of the EE involved fundamental imaging. The technology has improved considerably with the development of harmonic imaging and continuous image acquisition, which may signify a greater sensitivity. Unfortunately, this is a common problem that affects the longitudinal studies performed in this field.
Finally, although the relationship between the exacerbation of MR during exercise and hospital admissions for heart failure has been reported previously,6,18 and it would be an interesting issue to be confirmed, we unfortunately don't have this information available.
Clinical Implications
The severity of resting MR exhibits independent prognostic value for events and for cardiac death. The EE maintains its incremental prognostic value over resting echocardiography even when the latter includes information on the resting MR. The exacerbation or onset of MR during exercise has greater independent prognostic value for cardiac death than EE. These results provide additional evidence of the importance of the measurement of MR during EE for the determination of the prognosis.
ABBREVIATIONS
AMI: acute myocardial infarction
CI: confidence interval
ECG: electrocardiogram
EE: exercise echocardiography
HR: hazard ratio
LVEF: left ventricular ejection fraction
MR: mitral regurgitation
SMD: segmental motility disorder
See editorial on pages 228-30
Study financed by the Red Cardiovascular RECAVA.
Correspondence: Jesús Peteiro.
Ronda, 5, 4.o izqda. 15011 A Coruña. España.
E-mail: pete@canalejo.org
Received April 28, 2006.
Accepted for publication November 2, 2006.