To the Editor,
The diagnosis of apical hypertrophic cardiomyopathy (AHC) is based on the demonstration of myocardial hypertrophy in the apical region of the left ventricle, usually by echocardiogram.1 However, the ultrasound diagnosis is not always possible, unless a contrast agent is used to render the ventricular chamber opaque and thus obtain a typical "ace of spades" configuration of the left ventricle.2 On the other hand, in patients with AHC, coronary disease is frequently suspected.3 Given the limitations of ultrasound and other non-invasive tests for the detection of ischaemia in these cases, multidetector computed tomography (CT), which makes it possible both to study the ventricular myocardium and the coronary arterial tree, is seen as a particularly interesting tool for the integral assessment of these patients.
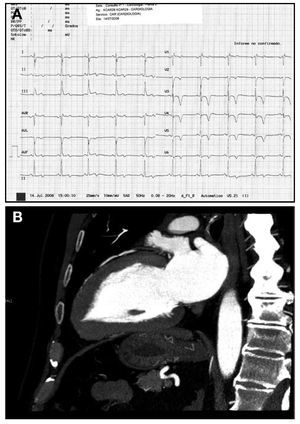
We present 3 patients with AHC who had a heart CT in our centre to rule out coronary disease. The first is a male who had previously had an echocardiogram for screening for hypertrophic cardiomyopathy (as he had a child diagnosed with this condition) and he was reported to be normal. Three years before he had consulted due to chest pain compatible with stress angina, but the echocardiogram test was negative. On this occasion the patient consulted due to progression of his angina. The echocardiogram showed a sinus rhythm, incomplete right bundle block and negative T waves of high amplitude in V4-V5 (Figure 1). A cardiac CT was indicated to rule out coronary disease. There was no significant coronary stenosis. Left ventriculography during cardiac CT showed a localized thickening of the apical segments of the left ventricular myocardium (Figure 1), which gave rise to a diagnosis of AHC.
Figure 1. A: 12 lead ECG in which it is possible to see deep inverted T waves in precordial leads. B: vertical long axis projection of two chambers obtained by computed tomography during diastole; it is possible to see the hypertrophy of the apical segments of the left ventricular myocardium and the typical "ace of spades" configuration seen in a ventriculography.
The second case is that of a 67-year-old woman, with a previous hospitalization due to chest pain. During this prior admittance her ECG showed a low amplitude T wave inversion, the echocardiogram did not show any significant alterations and a myocardial perfusion gamma scan ruled out ischaemia. In this case the patient consulted due to persistence of chest pain. The ECG showed a sinus rhythm, with criteria of left ventricle hypertrophy, T wave inversion in a precordial series of an amplitude >0.5 mV in V4-V5. A new echocardiogram was performed in which, suspecting AHC, contrast was given and the "ace of spades" image compatible with AHC was seen. To rule out coronary disease a non-invasive coronary angiography was performed with cardiac CT, which excluded significant arterial stenosis and confirmed thickening of the myocardium in an exclusively apical location compatible with AHC.
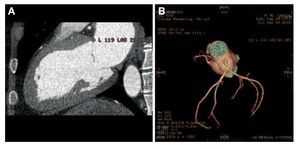
The third case was a 35-year-old male who was admitted with epigastric pain that irradiated upwards. The patient had previously been diagnosed with hypertrophic cardiomyopathy. In the echocardiogram it is possible to see a descent of ST of 2 mm in V3-V5 and negative T waves in DIII, aVF, and V3-V6. A cardiac US was performed and as AHC was suspected contrast was administered for confirmation. To rule out coronary disease, a non-invasive coronary angiography was performed using CT. In this study, there were no significant coronary stenosis and AHC was confirmed (Figure 2).
Figure 2. A: left ventriculography obtained by computed tomography of the heart, with the characteristic image of apical hypertrophic cardiomyopathy. B: 3D reconstruction (volume rendering) of the coronary tree, in which no significant stenoses are seen.
The first case studied serves to underline the importance of completing a cardiac CT with a study of the left ventricle in patients sent for noninvasive coronary angiography, especially if there were no significant coronary stenosis and changes have been seen in the ECG compatible with AHC. The utility of a cardiac CT for an integral assessment of AHC has already been pointed out in a clinical case in which the authors described a patient with known AHC and chest pain in whom non-invasive coronary angiography showed an intramyocardial trajectory of the LAD.4 Our experience confirmed the potential usefulness of cardiac CT in patients with chest pain in whom, due to their clinical profile and ECG alterations, for a differential diagnosis of AHC or a diagnosis of coexistence of AHC and coronary disease. In these, cardiac CT could be the proposed as the diagnostic exploration tool of choice, since it makes it possible to study both myocardial and coronary anatomy.