Chronic ischemic heart disease is the most prevalent of all cardiovascular diseases. Patients are at high risk of complications. In recent decades, changes may have occurred in the clinical characteristics of the disease, its treatment and control of risk factors.
MethodsA direct comparison of 2 national registries of patients with chronic ischemic heart disease carried out in 2006 (n=1583) and 2014 (n=1110).
ResultsWe observed statistically significant differences between the 2 registries, with a higher percentage of men and smokers in the 2014 registry, but a lower prevalence of diabetes mellitus and hypertension. Heart failure and stroke were more prevalent in the 2006 registry. Patients in the 2014 registry had better results for lipid profile, blood glucose, creatinine, and glomerular filtration rate. We observed higher use of recommended drugs for secondary prevention and an increased percentage of patients receiving optimal medical therapy, from 32.5% to 49.5% (P<.01). Use of high-intensity statin doses also increased from 10.5% to 42.8% (P<.01). We found better control of some risk factors (improved dyslipidemia, heart rate, and blood glucose in patients with diabetes) but worse blood pressure control.
ConclusionsThe clinical profile of patients with chronic ischemic heart disease is similar in the 2 registries. There has been an improvement in patients’ medical therapy and dyslipidemia control, blood glucose, and heart rate, but there is still much room for improvement in the control of other cardiovascular risk factors.
Keywords
Ischemic heart disease (IHD) is largely responsible for cardiovascular diseases still being the leading cause of death in the world.1 The reduced mortality rate in acute IHD2–4 has led to a significant increase in patients with stable IHD5 who are at high cardiovascular risk.6 This population benefits from maximum control of cardiovascular risk factors7 and maximum adherence to medical therapy.8–10
Several publications have highlighted the changes in the clinical profile of patients with acute IHD,2,4,11 but there is less evidence for patients with stable chronic IHD. A comparison of the 2 CARDIOTENS registries showed that, although the prevalence of heart failure and atrial fibrillation has increased by almost 30% among patients seen at cardiology clinics, chronic IHD is still the most prevalent heart disease, accounting for 50% of these patients.12 National data have recently shown that the prevalence of patients with chronic stable angina is less than 3.0% in the general population.13 However, there is an increasing prevalence of asymptomatic patients with a history of acute myocardial infarction5,14,15 or coronary revascularization.15–17 In view of the above data, we conducted a comparative study of 2 large registries of patients with chronic IHD in 2006 and 2014, with the aim of analyzing differences in clinical profiles, treatments, and control of risk factors in chronic IHD.
METHODSStudy DesignWe used the data from 2 registries compiled with a similar method by the Spanish Society of Cardiology. The TRECE registry14 included patients seen in 2006. Its results have already been published. The REPAR registry (Registro de la dislipemia en pacientes de muy alto riesgo cardiovascular [Registry of dyslipidemia in patients at very high cardiovascular risk]) included patients seen in 2014. This article presents the first data from a study that analyzed only patients with chronic IHD. Both registries were compiled from consecutive patients seen at outpatient clinics. Patients were recruited for the TRECE registry from cardiology, internal medicine, and primary care clinics. For the purpose of this study, we analyzed patients recruited by cardiologists only (1583 out of a total of 2897 patients). The inclusion criterion for both registries was stable chronic IHD. The REPAR registry was created to conduct a prospective, observational, multicenter, national study. The aim of this study was to identify the percentage of patients at very high cardiovascular risk who achieve the therapeutic target of a low-density lipoprotein cholesterol value of < 70mg/dL. Inclusion criteria were age > 18 years and very high cardiovascular risk, defined as fulfilment of 1 of the following criteria: SCORE (Systematic COronary Risk Evaluation) > 10%, documented cardiovascular disease, diabetes mellitus with target organ disease, or moderate or severe kidney dysfunction.18 Exclusion criteria were active malignant disease together with chemotherapy, human immunodeficiency virus with antiretroviral therapy, active hepatitis (with positive serology and active disease), any disease that, in the investigator's opinion, could confound the study results, and any situation that prevented the investigator's access to required study data. The final exclusion criterion was patients who had been enrolled in previous registries. The aim of this criterion was to include new patients and thus compare them with patients in other registries. The study protocol and informed consent were approved by at least 1 site in each Spanish autonomous community, except Cantabria, which abstained from participating. The protocol consisted of an enrolment visit and another visit 1 year later to collect all the risk factors, treatments, and routine blood test results from the previous 2 months. For analysis purposes, we used the data from the baseline visit of all patients with IHD. A total of 1291 patients were recruited at the first visit, 33 of whom were ruled out because they fulfilled exclusion criteria. The final cohort consisted of 1258 patients from 15 autonomous communities.
Scientific sections of the Spanish Society of Cardiology developed both registries. The Hypertension, Ischemic Heart Disease, and Clinical and Outpatient Cardiology Sections were responsible for the TRECE registry, and the Cardiology Risk and Cardiac Rehabilitation Section developed the REPAR registry.
Definition of VariablesAll therapies and doses received by patients before the visit were recorded, as well as any changes made. Optimal medical therapy (OMT) was considered as concomitant therapy with an antiplatelet agent, beta-blocker, statin, and an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker.9,10,19 In accordance with the 2013 ACC/AHA (American College of Cardiology/American Heart Association) guideline,20 therapy with high-intensity statin doses was considered as atorvastatin 40mg/d to 80mg/d or rosuvastatin 20mg/d to 40mg/d; moderate-intensity statin doses were considered as atorvastatin 20mg/d or simvastatin 20mg/d to 40mg/d; and low-intensity statin doses, atorvastatin 10mg/d, simvastatin 10mg/d or pravastatin 10mg/d to 40mg/d. To define controlled hypertension (HT), we used the targets established in the 2003 guidelines (< 140/90 mmHg). A controlled heart rate at rest was considered as < 70 bpm measured during the physical examination after 10 min of rest, or recorded in the electrocardiogram at the enrolment visit.9 The target value for dyslipidemia control was low-density lipoprotein cholesterol < 70mg/dL. Glycated hemoglobin was not recorded systematically in the TRECE registry, and therefore we evaluated diabetes mellitus control by means of fasting blood glucose. We considered that diabetes was controlled if the value was < 108mg/dL, and in patients without diabetes, we defined baseline control as < 100mg/dL.21 We considered obesity as a body mass index of > 30 and abdominal obesity as an abdominal girth of > 102cm in men and > 88cm in women. Glomerular filtration was estimated from serum creatinine values using the Modification of Diet in Renal Disease study equation.18
Statistical AnalysisFor the statistical analysis, we used the IBM SPSS 20.0 program (SPSS Inc.; Chicago, Illinois, United States). Quantitative variables are expressed as mean±standard deviation and the comparison of means was performed with the Student t test; qualitative variables are shown as percentages and the comparisons were studied by the chi-square test or Fisher's exact test, as appropriate. We used logistic regression to identify associations with high-intensity therapy. We analyzed logistic regression model goodness of fit by means of the Hosmer-Lemeshow method, and the diagnostic capacity by means of the area under the ROC (receiver operating characteristic) curve to evaluate the probability predicted by the model. Statistical significance was defined as P < .05.
RESULTSAs shown in Table 1, statistically significant differences were observed between the 2 registries, including a higher percentage of men and smokers in the 2014 registry, and a slightly lower prevalence of diabetes mellitus and HT. The combination of heart failure and stroke was higher in the 2006 registry. Patients in the 2014 registry had better blood test results for lipid profile, blood glucose, creatinine, and glomerular filtration rate.
General Characteristics of the Patients in Both Registries
| 2006 | 2014 | P | |
|---|---|---|---|
| Patients | 1583 (58.8) | 1110 (41.2) | |
| Age, y | 66.8±11.4 | 66.7±10.4 | .81 |
| Age > 75 y, % | 27.5 | 26.6 | .41 |
| Men, % | 73.0 | 80.8 | <.01 |
| BMI | 28.2±3.9 | 28.6±4.5 | .02 |
| Abdominal girth, cm | 98.9±11.6 | 99.0±12.2 | .86 |
| DM, % | 38.0 | 34.5 | .06 |
| Hypertension, % | 67.0 | 62.6 | .03 |
| Smoker, % | 12.3 | 15.4 | .02 |
| Time, y | 5.6±6.1 | 5.7±6.0 | .60 |
| Previous AMI, % | 45.8 | 64.4 | < .01 |
| Coronary revascularization, % | 63.4 | 70.2 | < .01 |
| Symptomatic angina, % | 31.1 | 33.1 | .22 |
| Heart failure, % | 15.5 | 9.3 | < .01 |
| Atrial fibrillation, % | 7.6 | 11.0 | < .01 |
| Previous stroke, % | 8.6 | 6.0 | .01 |
| Peripheral arterial disease, % | 15.3 | 13.4 | .22 |
| SBP, mmHg | 132.1±18.6 | 136.7±18.8 | < .01 |
| DBP, mmHg | 75.0±11.0 | 77.7±11.1 | < .01 |
| Heart rate, bpm | 68.7±12.8 | 66.1±11.4 | < .01 |
| Total cholesterol, mg/dL | 187.1±41.2 | 175.5±50.19 | < .01 |
| LDL-C, mg/dL | 112.3±36.2 | 98.0±43.7 | < .01 |
| HDL-C, mg/dL | 45.0±12.19 | 46.5±12.8 | < .01 |
| Triglycerides, mg/dL | 148.7±95.8 | 138.9±76.0 | .01 |
| Blood glucose, mg/dL | 121.9±46.7 | 111.1±28.9 | < .01 |
| Blood glucose in DM, mg/dL | 153.0±51.5 | 134.5±35.0 | < .01 |
| Creatinine, mg/dL | 1.12±0.5 | 1.04±0.5 | < .01 |
| GFR, mL/min/1.72 m2 | 73.7±25.1 | 82.9±65.8 | < .01 |
| GFR < 60 mL/min/1.72 m2, % | 27.9 | 18.2 | .01 |
AMI, acute myocardial infarction; BMI, body mass index; DBP, diastolic, blood pressure; DM, diabetes mellitus; GFR, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SBP, systolic blood pressure.
Unless otherwise indicated, data are expressed as No. (%) or mean ± standard deviation.
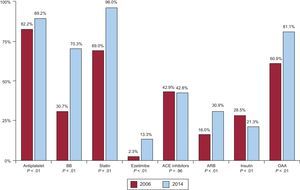
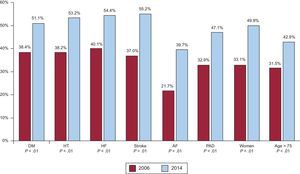
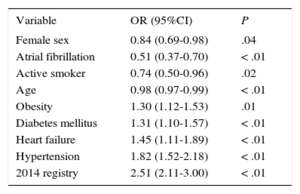
The use of recommended drugs for secondary prevention (Figure 1) was higher in the 2014 registry. Patients with diabetes had a significant increase in the use of oral antidiabetic agents, and reduced insulin use. Although the prevalence of symptomatic angina was similar in both registries, use of dihydropyridine calcium channel antagonists was lower in the 2014 registry (14.2% vs 17.5%; P=.02) and use of nitrates was much higher (19.4% vs 41.3%; P<.01); the same registry showed that ivabradine was used by 5.0% of patients and ranolazine by 3.2%. A higher number of patients (from 514 of 1583 to 550 of 1110) were receiving OMT, representing an increase from 32.5% to 49.5% (P<.01). This increase applied to all clinical scenarios (Figure 2). The highest increase in OMT was found in patients with atrial fibrillation and in women. Table 2 shows the variables associated with OMT. The strongest association was patients included in the 2014 registry.
Variables Associated With Patients Receiving Optimal Medical Therapy
| Variable | OR (95%CI) | P |
|---|---|---|
| Female sex | 0.84 (0.69-0.98) | .04 |
| Atrial fibrillation | 0.51 (0.37-0.70) | < .01 |
| Active smoker | 0.74 (0.50-0.96) | .02 |
| Age | 0.98 (0.97-0.99) | < .01 |
| Obesity | 1.30 (1.12-1.53) | .01 |
| Diabetes mellitus | 1.31 (1.10-1.57) | < .01 |
| Heart failure | 1.45 (1.11-1.89) | < .01 |
| Hypertension | 1.82 (1.52-2.18) | < .01 |
| 2014 registry | 2.51 (2.11-3.00) | < .01 |
95%CI, 95% confidence interval; OR, odds ratio.
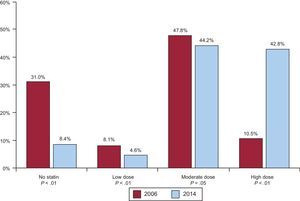
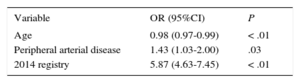
Data on statins showed increased atorvastatin use (from 41.3% to 46.5%; P<.01) and decreased simvastatin use (from 23.7% to 18.5%; P<.01). Rosuvastatin was not marketed at the time of the 2006 registry, while it was the second most commonly used statin (20.0%) in the 2014 registry. There was a significant decrease in the percentage of patients not receiving statin therapy and a marked increase in the use of high-intensity statin doses (Figure 3). Two variables, peripheral arterial disease and patients included in the 2014 registry, were independently associated with high-intensity statin doses (Table 3).
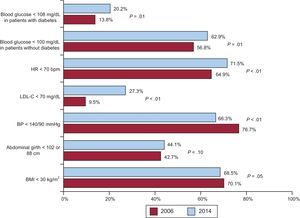
Finally, we analyzed changes in cardiovascular risk factors control and found improved control of dyslipidemia, resting heart rate, and blood glucose in patients with and without diabetes (Figure 4). Control of obesity and abdominal obesity was similar in both registries, while HT control was worse in the 2014 registry.
DISCUSSIONOur comparison of 2 national registries of patients with stable, chronic IHD shows that the main change in these patients is improved medical therapy, which has led to some improvement in the control of most risk factors. Since the general characteristics of the patients included in both registries are similar to those in other publications,4,6–8,10,13,15–17 we believe that our results are representative of daily clinical practice.
We were somewhat surprised by the slight decrease in the prevalence of HT and diabetes mellitus. However, the data from the 2014 registry are similar to the findings in EUROASPIRE IV,22 so this decrease may reflect a global trend among patients with chronic IHD. We were concerned about the increase in patients who admit they still smoke. This increase was also observed in the EUROASPIRE IV survey and the CLARIFY chronic IHD registry.15 A Spanish registry that specifically studied smoking status among patients with acute coronary syndrome showed that 22% of patients continued smoking 1 year after this event23; furthermore, most patients did not receive smoking cessation support or treatment. Smoking cessation is an essential goal in secondary prevention, because it reduces the incidence of complications and death.7 However, registries and studies conducted in patients with chronic IHD generally show that 10% to 20% of these patients are active smokers.15–17,24 Our study not only confirmed that a substantial percentage of patients with chronic IHD still smoke, but also that this percentage appears to be increasing, which is a highly relevant message for professionals who monitor and treat these patients.
The prevalence of symptomatic angina was similar in both registries, despite an increase in coronary revascularization procedures. There was a much lower use of nitrates in the 2014 registry, and this finding was also observed in the CLARIFY registry.15 These changes may reflect the finding in many national registries4,25,26 that a large majority of patients with new-onset IHD are admitted to hospital and receive coronary revascularization, and therefore require fewer anti-anginal agents.15,16 We found a slightly higher prevalence of symptomatic angina than the 21.8% prevalence observed in the CLARIFY registry,15 but a much lower prevalence than the 50% prevalence observed in the AVANCE registry.16 Therefore, our study results appear to represent real clinical practice. To some extent, these results may have been influenced by the type of coronary revascularization, because percutaneous and surgical revascularization were performed in 49.7% and 18.6%, respectively, of patients in the TRECE registry. However, it is hard to draw conclusions from these data.
We observed significant progress in the use of the drugs recommended for secondary prevention in patients with chronic IHD and in the rate of OMT, although the latter remains low. Boden et al19 found that OMT was as effective as percutaneous coronary revascularization in patients with chronic stable angina, while other studies8–10 have found that OMT improves survival and reduces the incidence of complications after acute coronary syndrome. In addition, our data show increased OMT in all clinical scenarios associated with chronic IHD, which sometimes include undertreated subgroups. However, we were unable to analyze the presence of formal contraindications to OMT or drug use in these undertreated subgroups. The TRECE registry showed that atrial fibrillation is one of the main conditions that limits the use of OMT.14 Our comparative analysis with the REPAR registry revealed considerable progress in the treatment of this condition, which may reflect greater awareness of individual risk.27 We also observed a marked increase in OMT among elderly patients and women, which may reflect greater awareness among clinicians treating these patients. Although we also observed increased use of beta-blockers, this therapeutic group is still the least used of all drugs in OMT. Recent registries have questioned their usefulness in improving the prognosis of patients with stable chronic IHD.28 A recent meta-analysis suggests that the real benefit of beta-blockers was attained only in patients with acute myocardial infarction in the prereperfusion era.29 However, Spanish data continue to show that beta-blocker therapy is of prognostic benefit in patients with acute coronary syndrome.26
We observed an important change in the use of statins from one registry to the other. The percentage of patients not receiving statins decreased to less than 9%, which may still appear to be too high, but coincides with other registries of patients with chronic IHD.15–17,22 A novel aspect of statin use is changed dose intensity. There was a marked increase in high-intensity statin doses, and moderate-intensity statin doses were most commonly used in both registries. The ACC/AHA guideline on dyslipidemia published in 201420 proposed using high-intensity statin doses for all patients with chronic IHD, regardless of their baseline low-density lipoprotein cholesterol, and without a specific treat-to-target strategy. This paradigm shift was criticized in the context of primary prevention, but received less opposition as a recommendation for patients with established IHD.30 Our results show a low rate of low-density lipoprotein cholesterol control, despite a marked increase in the use of statins and high doses. This low rate of control could be attributed to low-intensity statin doses,31 lack of patient adherence, or limited treatment with combined lipid-lowering agents.17 In general, we found that dyslipidemia has undergone the greatest increase in control out of all risk factors, and this finding coincides with other publications.14,24 However, dyslipidemia is still the least controlled risk factor, reflecting the complexity of controlling dyslipidemia in patients at very high cardiovascular risk.
The increased use of drugs and higher rate of OMT have led to greater control of some risk factors, such as dyslipidemia and heart rate, but have not improved HT control. The prevalence of obesity was very high and was similar in both registries. This persistently high prevalence may be explained by a lack of initiatives and practical recommendations for patients with obesity. Our data for obesity and abdominal girth largely coincide with the recent results of the EUROASPIRE IV survey.22 Hypertension control appears to be decreasing. The CARDIOTENS 2009 registry32 showed that HT was controlled in 55% of patients with heart disease and that the main factors associated with HT were diabetes mellitus, obesity, and smoking. Unlike the dyslipidemia guideline, the latest Eighth Joint National Committee guideline for HT recommends more lenient control targets for some patient groups, such as patients older than 60 years without cardiovascular disease or diabetes mellitus.33 This recommendation has been criticized widely and some publications have already responded that these more lenient control targets are associated with lower cardiovascular protection.34 Our study suggests that efforts to control blood pressure may have relaxed somewhat, which may also be influenced by the absence of therapeutic developments.
LimitationsThis study has some limitations. First, our comparison of 2 independent registries simply analyzed changes in the clinical profile of patients with IHD and the treatment they received at a given moment, rather than following the clinical course of these patients. Second, some data (eg, type of revascularization, ejection fraction, and some drugs) were available only in 1 registry, and therefore our analysis may have overlooked some confounding factors and interactions.
CONCLUSIONSThe clinical profile of patients with chronic IHD varied only slightly between 2006 and 2014, but we observed significant progress in the use of drugs recommended for secondary prevention in guidelines. We also found that a higher percentage of patients now receive OMT for chronic IHD. Despite progress in the control of some cardiovascular risk factors (eg, dyslipidemia and heart rate), obesity, smoking, and hypertension remain major challenges in secondary prevention among patients with chronic IHD.
FUNDINGThe TRECE and REPAR registries were funded by unrestricted research grants from Laboratorios Servier and Laboratorios Ferrer, respectively.
CONFLICTS OF INTERESTNone declared.