From an epidemiological point of view, new data have been obtained from the EUROASPIRE IV registry.1 This 24-country registry included 16 426 patients younger than 80 years who were admitted for acute coronary syndrome (ACS) or underwent a coronary, surgical, or percutaneous intervention with at least 6 months’ follow-up.
The results were unmistakably negative. Although the patients were in secondary prevention, with a consequently more intensive follow-up and risk factor treatment, 48.6% of smokers continued to smoke, 37.6% were still obese (body mass index ≥ 30), 42.7% had blood pressure ≥ 140/90mmHg, 26.8% were diabetic, 80.5% showed a low-density lipoprotein-cholesterol level ≥ 70mg/dL, and less than half had been referred to a cardiac rehabilitation program.
In the field of cardiovascular prevention, the most important study of 2015 was probably the IMPROVE-IT trial.2 This study randomized 18 144 ACS patients to either simvastatin 40mg or simvastatin 40mg plus ezetimibe 10mg. Patients had to have been admitted for ACS in the 10 days before their randomization, be older than 50 years, and have one of the following: new ST-segment alteration, elevated troponins, diabetes mellitus (DM), previous infarction, peripheral arterial disease, cerebrovascular disease, or bypass surgery more than 3 years prior to entry. The mean follow-up duration was 57 months.
The primary composite end point of cardiovascular death, nonfatal myocardial infarction, unstable angina, and coronary revascularization showed an absolute risk reduction of 2.0%. At the European Society of Cardiology (ESC) congress of 2015, different subanalyses were presented showing that ezetimibe treatment did not increase the risk of diabetes mellitus or cancer during follow-up and might even have an added benefit in diabetic patients. Thus, the study showed that lower low-density lipoprotein-cholesterol levels (even<50mg/dL) lead to fewer cardiovascular events.
In the ODYSSEY LONG TERM study,3 alirocumab, a member of the family of new lipid-lowering PCSK-9 inhibitors, significantly decreased low-density lipoprotein-cholesterol after 24 weeks of treatment (–62%; P<.001). In post-hoc analysis, the rate of cardiovascular events was lower in the alirocumab group (1.7% vs 3.3%; P=.02). These good results were even seen after comparison with the combination of maximum dose statins+ezetimibe and in patients with heterozygous familial hypercholesterolemia.4,5
In the area of DM, the TECOS study6 included 14 671 patients with type 2 diabetes mellitus and established cardiovascular disease and showed that addition of sitagliptin to standard antihyperglycemic therapy did not increase the number of cardiovascular events (cardiovascular death, nonfatal infarction or stroke, hospitalization for unstable angina) during a median follow-up of 3 years (11.4% with sitagliptin vs 11.6% with placebo). In the ESC congress, a preplanned subanalysis was presented that concluded that this approach did not increase the rate of admissions for heart failure (7.4% vs 7.0%). Similarly, lixisenatide (the ELIXA study7) did not increase the number of cardiovascular events.
BIOMARKERS AND DIAGNOSTIC TECHNIQUESTwo contributions have to be highlighted regarding biomarkers of ischemic heart disease. First, new data on their usefulness, but also a difficulty caused by the widespread use of troponin measurement in patients admitted to the emergency room. The problem arises when elevated troponins are detected and the clinical history permits an alternative diagnosis to infarction. This aspect and its serious repercussions on the prognosis of patients with elevated troponin who are not classified as having ACS are discussed in the article by Bardají et al,8 which presents a consecutive series of 1032 patients admitted to the emergency room and with a follow-up of 1 year.
Second, new biomarkers could be useful for patients with infarction. Peroxisome proliferator-activated receptor gamma coactivator 1-alfa is a metabolic regulator induced during ischemia that prevents cardiac remodeling in animal models. In humans, the baseline expression of this coactivator and an attenuated systemic response after acute myocardial infarction (AMI) are associated with greater myocardial salvage and predict less ventricular remodeling.9
Highlights related to ischemic heart disease imaging include new contributions from the SCOT-HEART study,10 involving 9847 patients with chest pain indicative of angina pectoris. These patients were randomized to the standard evaluation of suspected ischemic heart disease vs additional computed tomography (CT) coronary angiography. The use of CT coronary angiography changed the planned investigations (15% vs 1%; P<.0001) and treatments (23% vs 5%; P<.0001) but failed to decrease 6-week symptom severity or subsequent rehospitalizations for chest pain. After 1.7 years, the use of CT coronary angiography was nonsignificantly associated with a 38% reduction in fatal and nonfatal AMI.
A similar study was PROMISE,11 which randomized 10 003 patients with chest pain to a strategy of initial anatomical testing with CT coronary angiography or a strategy of functional testing (exercise electrocardiography, nuclear stress testing, or stress echocardiography). The CT coronary angiography strategy failed to improve the clinical results at a median follow-up of 2 years vs functional testing. These 2 studies are complemented by a publication by a group from Hospital Clínic in Barcelona.12 This study compared the usefulness of coronary CT with that of stress echocardiography in patients with acute chest pain, normal troponins, and normal electrocardiography. Both techniques showed excellent sensitivity and acceptable specificity, although the study did not evaluate the impact of more simple strategies such as conventional stress testing in terms of avoiding significant clinical events. Finally, stress cardiac magnetic resonance imaging was shown to be a useful technique for prognosis determination in patients with reduced ventricular function,13 with only a perfusion defect predicting clinical events in a multivariate regression model.
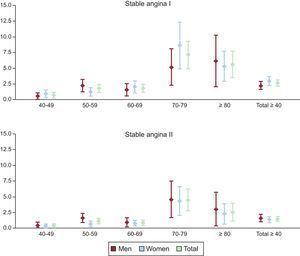
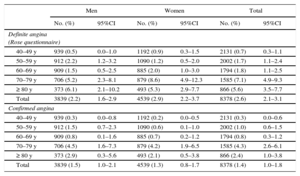
STABLE CHRONIC ISCHEMIC HEART DISEASEAnother recent publication was that of the OFRECE study.14 One of its objectives was to estimate the prevalence of stable angina in the Spanish population ≥ 40 years. In a representative sample of 8400 people, the prevalence of stable angina in Spain was low (definite angina according to the Rose questionnaire, 2.6%; confirmed angina, 1.4%) (Table), but increased with age, reaching 7.1% in individuals aged between 70 and 80 years (Figure). This figure is lower than previous estimates made more than 15 years ago in Spain and than European data as a whole and thus agrees with the lower cardiovascular mortality seen in Spain and other Mediterranean countries. The study found that 4.9% of the Spanish population had a history of acute ischemic heart disease that became chronic.14 Thus, there are about 1 100 000 patients with chronic coronary disease in Spain, although only 24% would have clinically overt disease; the rest, more than 850 000, would require health care centered on secondary prevention.
Prevalence of Stable Angina (Definite Angina According to the Rose Questionnaire and Confirmed Angina) by Sex and Age Group*
| Men | Women | Total | ||||
|---|---|---|---|---|---|---|
| No. (%) | 95%CI | No. (%) | 95%CI | No. (%) | 95%CI | |
| Definite angina (Rose questionnaire) | ||||||
| 40–49 y | 939 (0.5) | 0.0–1.0 | 1192 (0.9) | 0.3–1.5 | 2131 (0.7) | 0.3–1.1 |
| 50–59 y | 912 (2.2) | 1.2–3.2 | 1090 (1.2) | 0.5–2.0 | 2002 (1.7) | 1.1–2.4 |
| 60–69 y | 909 (1.5) | 0.5–2.5 | 885 (2.0) | 1.0–3.0 | 1794 (1.8) | 1.1–2.5 |
| 70–79 y | 706 (5.2) | 2.3–8.1 | 879 (8.6) | 4.9–12.3 | 1585 (7.1) | 4.9–9.3 |
| ≥ 80 y | 373 (6.1) | 2.1–10.2 | 493 (5.3) | 2.9–7.7 | 866 (5.6) | 3.5–7.7 |
| Total | 3839 (2.2) | 1.6–2.9 | 4539 (2.9) | 2.2–3.7 | 8378 (2.6) | 2.1–3.1 |
| Confirmed angina | ||||||
| 40–49 y | 939 (0.3) | 0.0–0.8 | 1192 (0.2) | 0.0–0.5 | 2131 (0.3) | 0.0–0.6 |
| 50–59 y | 912 (1.5) | 0.7–2.3 | 1090 (0.6) | 0.1–1.0 | 2002 (1.0) | 0.6–1.5 |
| 60–69 y | 909 (0.8) | 0.1–1.6 | 885 (0.7) | 0.2–1.2 | 1794 (0.8) | 0.3–1.2 |
| 70–79 y | 706 (4.5) | 1.6–7.3 | 879 (4.2) | 1.9–6.5 | 1585 (4.3) | 2.6–6.1 |
| ≥ 80 y | 373 (2.9) | 0.3–5.6 | 493 (2.1) | 0.5–3.8 | 866 (2.4) | 1.0–3.8 |
| Total | 3839 (1.5) | 1.0–2.1 | 4539 (1.3) | 0.8–1.7 | 8378 (1.4) | 1.0–1.8 |
95%CI, 95% confidence interval.
Prevalence of definite angina according to the Rose questionnaire (stable angina I) and confirmed angina (stable angina II) by sex and age group. OFRECE study. Reproduced with the permission of Alonso et al.14
In the 3 main congresses held in the last year, various clinical trials were published on the duration of dual antiplatelet therapy (DAPT) in patients with coronary heart disease. Three studies provided the most important information on this subject. The first was the DAPT study,15 a clinical trial of almost 10 000 patients who had received a stent (most stents were covered and only 26% of the patients had a history of ACS) and had completed the first year with DAPT without problems. The DAPT consisted of with clopidogrel (65%) or prasugrel (35%). In the follow-up from the end of the first year to 30 months after stenting, there were fewer stent thrombosis incidents (0.4% vs 1.4%) and major adverse cardiovascular events (myocardial infarction, stroke, or death, 4.3% vs 5.9%) in the group assigned to DAPT, albeit at the expense of more moderate or severe hemorrhagic complications (2.5% vs 1.6%). However, the finding of a slight significant increase in mortality (particularly cancer mortality) overshadowed the strategy (in the article, this finding was described as being of unknown significance).
In the PEGASUS-TIMI 54 study,16 more than 21 000 patients with history of infarction 1 to 3 years before inclusion were randomized to acetylsalicylic acid (ASA) or ASA plus ticagrelor (90mg or 60mg) twice a day. Those assigned to DAPT showed a lower incidence of major adverse events at 3 years (cardiovascular death, myocardial infarction, or stroke), with an absolute reduction of 1.2%, and lower rates of myocardial infarction and cardiac death. There was no increase in overall mortality, contrary to the DAPT study. As expected, the risk of major hemorrhagic events increased, but not the rate of intracranial and fatal bleeding. Finally, the French study OPTIDUAL17 was presented at the 2015 ESC meeting. This study involved 1398 patients with chronic heart disease or ACS who had received a stent and had been treated for 1 year with ASA and clopidogrel. These patients were randomized to continue with DAPT or with ASA alone. There were no differences in the primary outcome (cardiac mortality, ischemic events, and major bleeding), although there was a tendency for fewer ischemic events in the DAPT group.
Based on the data presented this year, it seems reasonable to conclude that DAPT reduces ischemic events in patients with chronic heart disease at the expense of increased major bleeding events, and that improvements should be made to the tools available for stratifying and identifying suitable patients, namely, those with greater thrombocytic risk and lower risk of bleeding.
The follow-up data of all of these studies indicate that patients with chronic heart disease continue to have an excellent prognosis. Even higher-risk patients, such as those in the PEGASUS study,16 who had history of infarction, show a cardiovascular mortality of only 2.9% and an infarction rate of 4.45% at 3 years. At 3.5 years, the patients in the OPTIDUAL study17 showed a rate of death, stroke, or myocardial infarction of 6.4% in those assigned to ASA alone and 4.2% in those treated with DAPT.
NON—ST-SEGMENT ELEVATION ACUTE MYOCARDIAL INFARCTIONThe first clinical trial was published on manual thrombus aspiration followed by percutaneous coronary intervention (PCI) in patients with non—ST-segment elevation AMI.18
This study included 440 patients and used cardiac magnetic resonance imaging to quantify the primary end point of microvascular obstruction. The infarct size and degree of reperfusion were secondary end points. Adjunctive thrombectomy with PCI was not better than PCI alone.
The safety of PCI in real-world practice was confirmed in centers without on-site cardiac surgery.19 The mortality and rate of AMI at 1 year were similar in 6900 patients who underwent PCI in centers without on-site cardiac surgery and in 17 487 patients treated in centers with surgery. However, the need for subsequent revascularization was higher in centers without cardiac surgery (hazard ratio =1.21; 95% confidence interval [95%CI], 1.03-1.42).
The efficacy and safety of prasugrel (n=1394) and placebo (n=1376) were compared in a subanalysis of the ACCOAST study20 including patients with non—ST-segment elevation AMI who underwent PCI. The 2 groups showed similar rates of cardiovascular death, AMI, stroke, urgent revascularization, and use of glycoprotein IIb/IIIa inhibitor bailout. However, a higher bleeding rate was recorded in patients pretreated with prasugrel (4.2% vs 1.4%; P<.001).
For the first time, data are available on the use of fondaparinux outside of clinical trials. In a registry of 40 616 patients with non—ST-segment elevation AMI,21 the rates of severe bleeding and in-hospital death were compared between fondaparinux (n=14 791; 36.4%) and low-molecular-weight heparin. The study also compared the 30- and 180-day incidence of death, AMI, stroke, and severe bleeding. There was less in-hospital severe bleeding with fondaparinux (adjusted odds ratio [OR]=0.54; 95%CI, 0.42-0.70), as well as lower mortality (adjusted OR=0.75; 95%CI, 0.63-0.89). These differences were maintained at 180 days. There were no differences in the rate of AMI or stroke at 30 and 180 days.
Adherence to the guidelines on non—ST-segment elevation ACS was accompanied by a lower rate of in-hospital mortality and bleeding complications in centers participating in the CRUSADE study.22
The optimum time for coronary revascularization surgery after non—ST-segment elevation AMI is unclear. In a study of 758 patients, patients who underwent surgery in the first 24hours showed a similar rate of in-hospital and 5-year mortality as those who underwent surgery after 72hours, despite the worse risk profile of the first group of patients.23 A delay in the surgery to between 24 and 72hours was associated with worse results.
In a meta-analysis of 10 recent clinical trials24 with 32 287 patients treated with PCI and a drug-eluting stent, a standard guideline of 12-month DAPT showed equal rates of ischemic complications but less bleeding (OR=0.58; 95%CI, 0.36-0.92) vs>12-month DAPT. In patients with low bleeding risk but high ischemic risk, DAPT reduced reinfarctions (OR=0.53; 95%CI, 0.42-0.66) and stent thrombosis (OR=0.33; 95%CI, 0.21-0.51) at the expense of higher risk of bleeding (OR=1.62; 95%CI, 1.26-2.09). There was higher overall mortality (OR=1.30; 95%CI, 1.02-1.66) with the>12-month DAPT guideline. However, another meta-analysis of 14 clinical trials and 69 644 patients showed neutral mortality results with>12-month DAPT.25
The ISAR-SAFE study26 randomized 614 patients (31.2% with non-ST elevation ACS) treated with ASA and oral anticoagulation to additional therapy with clopidogrel for 6 weeks or 6 months. The prolonged strategy was not better with respect to the composite outcome of death, AMI, stent thrombosis, stroke, or major bleeding.
The MATRIX study27 randomly assigned to femoral or radial access 8404 patients with ACS who underwent coronary catheterization and PCI. The study compared the coprimary objective of death, AMI, or stroke and net adverse clinical events, defined as major adverse cardiovascular events or Bleeding Academic Research Consortium major bleeding unrelated to the coronary surgery. Radial access significantly reduced net adverse clinical events by reducing major bleeding events and overall mortality.
An exploratory nonrandomized analysis of the MATRIX study28 compared bivalirudin infusion during PCI to infusion during and after PCI in 2987 patients with ACS. Both strategies showed similar efficacy, but there was more bleeding with prolonged infusion (1.0% vs 1.8%; P=.03).
Finally, new guidelines on non-ST elevation ACS have been published by both the American College of Cardiology/American Heart Association and the ESC.
ST-SEGMENT ELEVATION ACUTE CORONARY SYNDROMEThe development of regional health care systems to improve the time to reperfusion of patients with ST-segment elevation acute coronary syndrome (STEACS) remains a priority. In this setting, the final results of the STEMI-ACCELERATOR study29 were published: after optimization of the health care system in 16 regions of the United States and evaluation of 3538 patients with STEACS, collaboration between the emergency services and the cardiology and catheterization teams was found to improve survival and response times.
Most studies presented in 2015 failed to show clinical benefits from drug therapies. Thus, the effect of oxygen administration during STEACS was analyzed in the AVOID study.30 Of 638 randomized patients, 441 were included in the end point analysis, which involved infarct size measurement with biomarkers of necrosis and magnetic resonance imaging. The group treated with oxygen therapy showed a greater increase in creatine kinase, but not troponin. Curiously, the rates of reinfarction and ventricular arrhythmias in the oxygen therapy group were significantly higher than in those not treated with oxygen. In addition, at 6 months, the size of the infarct measured by magnetic resonance imaging was significantly higher in the oxygen therapy group. The ALBATROSS study31 evaluated the early addition of aldosterone antagonists in 1622 patients with ACS without heart failure. The primary end point of the study was a combination of sudden cardiac death, significant ventricular arrhythmias, defibrillator implantation, or worsening heart failure at 6 months; no differences were seen between the 2 study groups. In a subgroup analysis of patients with STEACS, aldosterone antagonist therapy reduced death.
In the field of reperfusion-ischemia, the EMBRACE-STEMI trial32 evaluated the safety, tolerability, and effectiveness of Bendavia, an intravenously administered mitochondrially-targeted peptide. After the inclusion of 118 patients with STEACS (58 randomized to Bendavia and 60 to placebo), the researchers failed to detect differences in infarct size. In the recently published CIRCUS study,33 cyclosporin failed to decrease reperfusion damage. The study, which included 970 patients with previous STEACS treated with primary angioplasty in the first 12hours, found no beneficial effect of intravenous cyclosporin on cardiovascular events (death, heart failure, rehospitalization, and left ventricular remodeling).33
One notable study of coronary revascularization and stents was the ABSORB STEMI-TROFI II trial,34 presented in the ESC congress of 2015, which showed the noninferiority of a bioabsorbable device vs the XIENCE stent.
Finally, 2 preclinical Spanish studies have to be mentioned: the first analyzed the ischemia-reperfusion pattern in pigs after STEACS induction.35 Via magnetic resonance imaging, the authors found a less stable than expected ischemia-reperfusion pattern: it followed a “bimodal” pattern, with a first wave secondary to the reperfusion and a second wave that seemed to be due to the myocardial repair process. The other, the ECCLIPSE study36 of inhibition of platelet aggregation in healthy volunteers, compared the effect of oral ASA with that of intravenous administration of lysine acetylsalicylate, with a loading dose of prasugrel in both study groups. Lysine acetylsalicylate achieved faster and greater inhibition of platelet aggregation, with less intraindividual and interindividual variability. If these data are confirmed in ischemic patients, there would be a potential benefit for patients with STEACS.
CARDIOGENIC SHOCKThis year saw the publication of the results of the CardShock study,37 an international multicenter prospective registry that included all patients with cardiogenic shock of any cause seen in 9 tertiary hospitals. In about 1 of every 5 patients, the cardiogenic shock was not secondary to ACS. The in-hospital mortality rate was 37%, lower than in other series. This difference was largely due to lower mortality in patients with cardiogenic shock not secondary to ACS (mortality in ACS cardiogenic shock, 40%; mortality in non-ACS cardiogenic shock, 24%). Thus, there are major differences in the prognosis of cardiogenic shock according to cause. Another interesting contribution of the study is the CardShock risk scale. This tool uses clinical and biochemical variables easily obtained upon patient admission to stratify the short-term risk of death and could facilitate decision-making in these patients.
Since the publication of the IABP-SHOCK II study in 2012,38 the use of the intra-aortic balloon pump in patients with cardiogenic shock secondary to infarction has markedly deceased in most countries. The results of the study have been supported by a recent meta-analysis of 12 randomized clinical trials that also failed to show an association between the intra-aortic balloon pump and reduced mortality.39 A recent analysis of the National Data Cardiovascular Registry covering the period from 2009 to 2013 showed a progressive reduction in pump use of 0.3% per trimester.40 At the same time, there has been a significant increase in the use of other circulatory assist devices.41 However, there is a considerable uncertainty about whether circulatory assist devices have superior efficacy in important clinical results such as mortality and prevention of multiorgan failure. Recently, in a propensity score-matched analysis, treatment with circulatory assist devices was associated with higher mortality than intra-aortic balloon pumps (OR=1.23; 95%CI, 1.06-1.43; P=.007).41
The most promising circulatory assist device seems to be extracorporeal membrane oxygenation (ECMO). Analysis of an international cohort of 3846 patients treated with ECMO showed a promising rate of survival to hospital discharge (42%). At the same time, the main preimplantation factors associated with hospital survival were identified, in addition to the creation and validation of the SAVE prognosis score.42
CARDIAC ARREST CARE AND HYPOTHERMIATwo randomized trials of care during cardiac arrest compared manual chest compression and mechanical compression with the LUCAS system.43,44 Both studies concluded that the mechanically-assisted chest compression system was not superior to manual compressions in improving survival. Similarly, another work showed a higher incidence of injuries and rib fractures with the LUCAS device using autopsies of individuals who failed to recover from cardiac arrest.45
An interesting work, performed in France with 1134 survivors of a cardiac arrest, has questioned the use of adrenaline during cardiopulmonary reanimation,46 because it might worsen prognosis during postcardiac arrest syndrome by worsening myocardial function, increasing oxygen requirements and causing microvascular dysfunction. The primary outcome was survival with an acceptable neurological status of grade 1-2 with the Cerebral Performance Category scale. After adjustment for confounders (total time to return of spontaneous circulation and use of hypothermia or coronary revascularization), adrenaline was associated in a dose-dependent manner with worse neurological prognosis. These results should be considered hypothesis generators.
A Spanish group studying the neurological evaluation of patients in coma receiving therapeutic hypothermia designed a model to predict severe neurological damage (Cerebral Performance Category grades 3-5 or death during hypothermia) in a sample of 100 patients treated with hypothermia.47 Three variables (age, initial lactate level, myoclonus on admission) were associated with worse neurological prognosis. Similarly, the role of continuous electroencephalogram as a neurological assessment method was studied in 83 patients treated with hypothermia.48 Three patterns were associated with worse prognosis: burst suppression, isoelectric, and low-voltage wave (< 10 μV), particularly if they lasted more than 24hours after the cardiac arrest.
Due to the TTM (Targeted Temperature Management) trial, controversy continues to surround therapeutic hypothermia. Accordingly, various authors have written opinion pieces. One of these articles discusses the many limitations of the TTM trial,49 highlighting a possible selection bias, the delay between the cardiac arrest and hypothermia initiation (> 4 h), the long time to target temperature in the 33°C group, the accelerated reheating time, and the worse risk profile of the patients assigned to the 33°C group. Thus, a Spanish study presented in the last ESC congress reported that patients cooled to lower target temperatures could have a more delayed neurological recovery, so that any decision regarding limitation of therapeutic effort should be delayed to more than 5 days.50 In light of the evidence, strict maintenance of normothermia might be sufficient for some patients, such as those at high-risk of the secondary effects of hypothermia, but no method is currently available for selecting the target temperature; the ongoing FROST-I trial (NCT02035839)51 aims to obtain information on the optimum cooling temperature.
GENERAL ACUTE CARDIAC CAREFrat et al52 have published an open multicenter study of nonhypercapnic acute respiratory failure. Patients were randomized to standard oxygen, high-flow oxygen, or noninvasive mechanical ventilation. Although there were no statistically significant differences among the 3 groups in the intubation rate (38% with high-flow oxygen, 47% with standard oxygen, and 50% with noninvasive mechanical ventilation), the high-flow oxygen group required fewer days of invasive mechanical ventilation and showed a lower 90-day mortality (standard oxygen vs high-flow, hazard ratio=2.01; 95%CI, 1.01-3.99; noninvasive mechanical ventilation vs high-flow oxygen, hazard ratio=2.5; 95%CI, 1.31-4.78). Another trial of 830 patients compared high-flow oxygen with intermittent noninvasive mechanical ventilation after cardiothoracic surgery. Despite the complexity due to its noninferiority design, high-flow oxygen was not inferior to noninvasive mechanical ventilation.53
Two papers on the nutritional support of critical patients stand out. The PermiT clinical trial54 of 894 patients compared the impact of a reduced enteral caloric intake (40%-60% of the calculated caloric requirements) on 90-day mortality with that of full intake (70%-100%) during the first 14 days; both groups had a similar protein intake. There were no differences in mortality or the incidence of complications. The CALORIES study55 analyzed the route of delivery of nutritional support in 2388 critical patients randomized to parenteral or enteral routes; the support was initiated in the first 36hours and continued for 5 days. The primary end point was 30-day mortality. There were no differences in mortality between the 2 routes of delivery or in the rate of infectious complications or 90-day mortality. Parenteral nutrition was superior only in reducing hypoglycemia and vomiting.
In a population registry of 16 524 patients admitted to the emergency department due to acute heart failure, 30-day risk of death and new diabetes mellitus diagnosis and in-hospital complications were analyzed according to the blood glucose concentration at admission. The reference glucose value was 3.9-6.1 mmol/L. Crucially, glucose cutoff points indicating a higher risk of complications differed in diabetic and nondiabetic patients. In nondiabetic patients, blood glucose>6.1 mmol/L was associated with higher cardiovascular and all-cause death, with baseline values greater than>11.1 mmol/L increasing all-cause mortality in diabetic patients. In contrast, the blood glucose value showing the greatest risk of hospitalization due to heart failure or other cardiovascular causes was the same (> 9.4 mmol/L) for both known diabetic patients and those without diabetes.56
CONFLICTS OF INTERESTNone declared.