To the Editor:
Cardiac constriction is classically understood as a chronic disease which, in most cases, is resolved definitively by surgery.1 Modern imaging techniques have led to a change in this point of view by identifying cases in which this disease can be reversed.
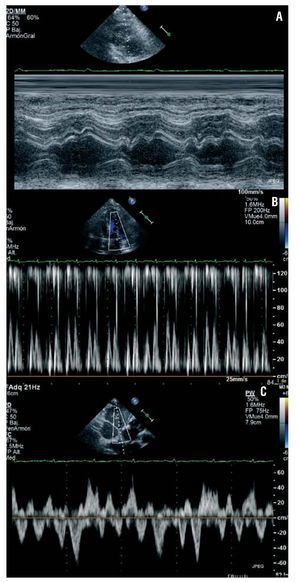
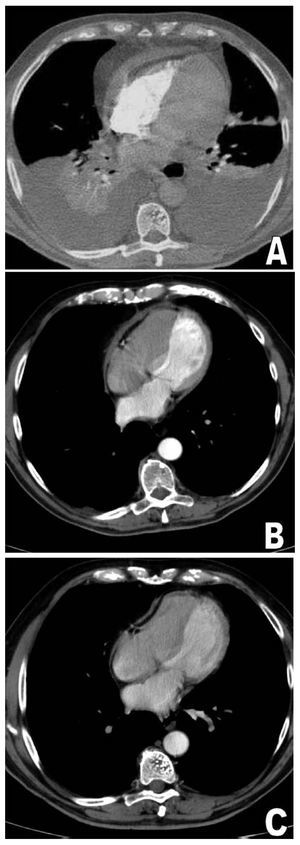
A male patient, 73 years of age, a former smoker with dyslipidemia, had been admitted at another centre 2 weeks before with a febrile disorder and a slight left-sided pleural effusion. He did not experience chest pain, nor could a pericardial friction rub be heard. Using computed tomography (CT) and an echocardiogram, a moderate pericardial effusion was detected with no signs of haemodynamic deterioration, and a full etiological study was carried out, which gave negative results. Pericardiocentesis was not performed. The patient became asymptomatic and afebrile, and was discharged 6 days later with a diagnosis of self-limited febrile syndrome. He was readmitted for dyspnoea, orthopnoea, and oedemas. The patient was afebrile, with a blood pressure of 118/80 mmHg and an oxygen saturation level of 92%. Auscultation revealed sinus rhythm at a rate of 100 beats/min, without murmurs or friction rubs, and signs of a bilateral pleural effusion. He presented jugular vein engorgement and significant oedema in both legs. The chest radiography confirmed cardiomegaly and bilateral pleural effusion. Thoracentesis drained a serous fluid with transudate characteristics and an ADA of 6.2 U/L. The echocardiogram showed alterations compatible with pericardial constriction (Figure 1) without effusion. Both the CT and the cardiac MRI confirmed a significant pericardial thickenning, with a maximum thickness of 20 mm in the anterobasal area (Figure 2A). Treatment was started with anti-inflammatory drugs, intravenous furosemide, and spironolactone, and various thoracentesis draining procedures were necessary. The need for pericardiectomy was considered, but in the following weeks the patient recovered significantly; the oedemas and the pleural effusion subsided progressively until resolution was complete. His dose of diuretics could be reduced. The CT performed 5 weeks later showed that the pericardial thickness had been reduced to 7 mm (Figure 2B) and that there was no pleural effusion. Six months after the episode, the patient is asymptomatic with no signs of heart failure and being treated with 20 mg furosemide and 25 mg spironolactone daily. The maximum pericardial thickness is 4 mm (Figure 2C) and the Doppler echocardiogram continues to show mild signs of constriction, such as abnormal septal movement and venous flow with a high diastolic component. The size and the respiratory oscillation of the inferior vena cava are normal, however, and no variations in transvalvular velocities are present with respiration.
Figure 1. A: anomalous movement of the interventricular septum, typical of constriction. B: cyclic variation in the transmitral flow E wave velocity with respiration. C: flow from suprahepatic veins with high diastolic pressure and marked inversions at the beginning of expiration.
Figure 2. A: anterobasal pericardial thickening of up to 20 mm. B: thickening of 7 mm. C: thickening of 4 mm.
Pericardial inflammation of any etiology can spark a process of thickening, fibrosis, and occasionally, calcification, which can lead to manifestations of cardiac constriction. This syndrome is characterised by resistant congestive heart failure, whose definitive treatment includes pericardiectomy.1 In 1987, Sagristá-Sauleda et al2 published a study of 177 patients with acute effusive pericarditis, 16 of wkom developed echocardiographic signs of constriction that resolved over a few weeks with no need for surgical intervention. Only 2 of them presented heart failure. This profile was called transient constrictive pericarditis (TCP) and since then, cases of TCP with varying aetiologies have been reported. Subsequently, Haley et al3 published a retrospective study of 36 patients with echocardiographic findings of constriction that resolved without pericardiectomy. Few of them had right heart failure. In this study, the most frequent causes of TCP were pericardiotomy-related (25%), idiopathic (22%), viral (19%), connective tissue disease-related (14%), and bacterial (11%). In both studies, the average resolution time for the constriction was between 8 and 12 weeks, with no recurrence observed.
In this case, the patient presented transient symptoms and findings of serious heart failure, with oedemas and abundant bilateral pleural effusion, which were not typical of those patients in the studies described.2,3 Also worthy of note was the magnitude of the pericardial thickening observed in this patient, reaching 20 mm, keeping in mind that thicknesses exceeding 3-4 mm are highly indicative of constriction in a compatible clinical profile. The present case indicates that the possibility of transient manifestation of constriction should not be discarded, even in cases of marked pericardial thickening and/or serious heart failure. It has been indicated that in cases of subacute constriction, before prescribing pericardiectomy, the option of medical treatment during 8 to 12 weeks should be considered, provided that the clinical situation permits it.3