Vasospastic angina (VSA) can result in endothelial damage and thrombus formation. The aim of this study was to evaluate the incidence of thrombus and plaque characteristics at coronary spasm segments compared with nonspasm segments by using optical coherence tomography (OCT) in patients with suspected VSA.
MethodsOne hundred and eighty-three patients with suspected VSA were enrolled in this study. The ergonovine provocation test was performed in all patients for the diagnosis of VSA except in patients with spontaneous spasm. All target lesions were analyzed by OCT. Plaque erosion was defined as the presence of attached thrombus overlying an intact fibrous cap and visualized plaque on multiple adjacent OCT frames.
ResultsOne hundred and nine spasm segments (93 patients) were compared with 55 nonspasm segments (39 patients). Thrombus was more frequently seen at spasm segments than at nonspasm segments (28.4% vs 7.3%; P = .026) and thrombus size was larger at spasm segments than at nonspasm segments (0.26 ± 0.50 mm2 vs 0.04 ± 0.01 mm2; P = .023). Thin-cap fibroatheroma was more frequently seen at nonspasm segments than at spasm segments (16.4% vs 1.8%; P = .006). Plaque erosion was more prevalent at spasm segments than at nonspasm segments (25.7% vs 5.4%; P = .001).
ConclusionsThrombus and plaque erosion were more common at spasm segments than at nonspasm segments assessed by OCT in patients with suspected VSA. These findings suggest the potential benefit and treatment role of antiplatelet therapy in vasospastic angina.
Keywords
Coronary artery spasm plays an important role in the pathogenesis of variant angina, as well as in various types of ischemic heart disease, including acute coronary syndrome.1 Although fibrous cap disruption complicated by thrombosis is considered to be the most important mechanism for the development of acute coronary syndrome,2,3 spasms of the coronary artery can also compress atherosclerotic plaques, causing vascular injuries and thrombus formation.4,5 Through postmortem examination, Maseri et al.6 revealed fresh thrombi at spasm sites and suggested that blood stagnation caused by spasm may result in thrombus deposition at the site of the damaged intima. In an animal experiment using electron microscopy, partial arterial constriction (40%-60% reduction in luminal diameter, which is insufficient to reduce the rate of distal coronary flow) resulted in endothelial denudation, platelet deposition, and microthrombus formation in areas proximal to the point of maximum constriction.7 Therefore, focal spasm can induce local hemodynamic changes that may result in endothelial damage and thrombus formation. Recently, we reported that optical coherence tomography (OCT)-defined erosion with thrombus occurred in more than one fourth of patients with vasospastic angina (VSA).8 However, these changes have not been studied by comparing spasm and nonspasm segments.
We therefore aimed to evaluate the in vivo morphological characteristics and thrombus formation at coronary spasm segments compared with nonspasm segments by using OCT in patients presenting with suspected VSA.
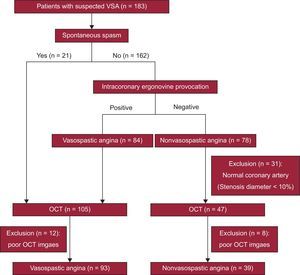
METHODSStudy PopulationThis study was conducted at Ulsan University Hospital. Patients were enrolled between October 2011 and December 2014. The OCT findings in patients diagnosed with VSA during this period have already been published; among these, 62 patients in Ulsan University Hospital were included in this study.8 We included consecutive patients with suspected VSA presenting with resting chest pain who underwent elective coronary angiography, an ergonovine provocation test if spontaneous spasm was absent, and OCT imaging. The study flowchart is shown in Figure 1. Patients with angiographically significant coronary artery disease (stenosis diameter ≥ 50%) were excluded from this study. To diagnose VSA, the following 2 criteria were required9; a) spontaneous or ergonovine-induced coronary artery spasm (producing > 90% narrowing of coronary lumen diameter by angiography) associated with chest pain and ischemic ST-segment changes (transient ST-segment elevation or depression of ≥ 0.1mV, recorded on at least 2 contiguous leads on 12-lead electrocardiography), and b) insignificant coronary artery disease (stenosis diameter < 50%) after intracoronary nitroglycerine injection. Patients who did not meet the above-mentioned criteria for VSA diagnosis were grouped as non-VSA. Although all included patients had clinically-suspected VSA, nonspasm segments were defined as those not meeting the criteria for spasm segments. However, it is difficult to distinguish spasm from nonspasm segments on coronary angiography if the stenosis diameter is < 10% after a provocation test. For the same reason, because it was difficult to determine the target site (nonspasm segment) of OCT, it was excluded. Therefore, for nonspasm segments, OCT was performed in segments with a stenosis diameter ≥ 10%, which could be distinguished by the naked eye, as a target. Only 1 nonspasm segment was taken from each vessel. Calcium channel blockers and nitrates were stopped for at least 48hours before the ergonovine provocation test. All patients were prescribed a loading aspirin dose of 200mg and 300mg of clopidogrel. Unfractionated heparin (100 U/kg) was injected intravenously to maintain an activated clotting time ≥ 250s throughout the procedure. After baseline angiography of the left and right coronary artery, the operator proceeded with the ergonovine provocation test if no significant angiographic stenosis was seen at multiple angiographic projections. Intracoronary ergonovine was used in the left and right coronary arteries, respectively, at incremental doses of 20μg, 40μg and 60μg with 2-minute intervals between doses.10 If angiographic findings showed focal luminal narrowing of more than 90% with chest pain and electrocardiography changes (ST elevation or depression ≥ 0.1mV on at least 2 contiguous leads), 200μg of intracoronary nitroglycerine was used to confirm the diagnosis of VSA.10 There were no complications such as arrhythmia and myocardial infarction during the ergonovine provocation test.
We excluded patients with comorbidities such as congestive heart failure, cardiomyopathy, chronic kidney disease, a past history of fatal arrhythmias, prior myocardial infarction, previous percutaneous coronary intervention, and cardiogenic shock. This study complied with the Declaration of Helsinki and was approved by the Institutional Review Board ethics committee (number 2014-08-019). Written informed consent was obtained from all participants before they participated in any part of the study.
Quantitative Coronary AngiographyCoronary angiographies were analyzed with the Cardiovascular Angiography Analysis System (CAAS 5.10, Pie Medical Imaging B.V., Maastricht, Netherlands) by an independent investigator (JH Lee) who was blinded to the OCT analysis. The reference vessel diameter, minimum lumen diameter, stenosis diameter, and spasm segment length were measured.
Optical Coherence Tomography Image AcquisitionUnfractionated heparin at a dose of 100 U/kg was injected intravenously to maintain an activated clotting time ≥ 250s throughout the OCT procedure. Optical coherence tomography was performed in all patients after administration of 200μg of intracoronary nitroglycerine, and images were acquired using the commercially available Fourier-domain OCT (C7XR and Dragon Fly catheter, Lightlab Imaging/S. Jude Medical, Westford, Massachusetts, United States). A 2.7-Fr OCT imaging catheter was carefully advanced distal to the target spasm segment or nonspasm segment along an 0.014-inch guidewire. Using the nonocclusive technique, automated pullback was performed at a rate of 20mm/s, while blood was displaced by a short injection of contrast media through the guiding catheter. The images were digitally stored for off-line analysis.
Optical Coherence Tomography Image AnalysisOptical coherence tomography images of spasm and nonspasm segments were analyzed at 0.2-mm intervals by 2 independent investigators (A.Y. Her and S.H. Ann), who were blinded to clinical presentations. When there was discordance between the investigators, a consensus reading was obtained from a third investigator (E.S. Shin). The OCT images were analyzed 5-mm proximally and distally from the maximum spasm site in VSA and from the minimal atherosclerotic lesions in nonspasm segments, respectively. This was confirmed with the corresponding coronary angiography using side branches as markers by an independent, blinded investigator (E.R. Cho).
Study OutcomesThe study outcome was the incidence of thrombus and the plaque characteristics at coronary spasm segments compared with nonspasm segments assessed by OCT. Thrombus was defined as a floating or protruding mass into the lumen of a size > 200μm and was categorized as platelet-rich (white) thrombus, defined by homogeneous backscattering with low attenuation, or as erythrocyte-rich (red) thrombus, defined by high backscattering and high attenuation.11 The largest thrombus visualized was measured for area and maximal and minimal diameter. Plaque erosion was defined as the presence of attached thrombus with or without lumen irregularity overlying an intact fibrous cap and visualized plaque on multiple adjacent OCT frames.12 Fibrous cap disruption was identified by discontinuation of the fibrous cap with or without intraplaque cavity formation. In this study, the presence of plaque at the spasm segments or nonspasm segments was defined as intimal thickening of ≥ 500μm observed by OCT. Tissue characteristics of underlying plaque were defined by using previously established criteria.13 Plaque was classified as: a) fibrous plaque (homogeneous, high backscattering region), or b) lipid laden plaque (≥ 1 quadrant of regions with low backscattering and diffuse borders); if, in addition, the plaque had a fibrous cap < 65μm, it was defined as thin-cap fibroatheroma. Interobserver variability was assessed by evaluation of 12% of the random images by 2 independent observers. Intraobserver variability was assessed at 2-week intervals by evaluation of the random images by an independent investigator. The intraobserver kappa coefficients for plaque disruption, lumen irregularity, thrombus, and plaque classification were 1.000, 1.000, 0.918, and 0.940, respectively. The interobserver kappa coefficients for plaque disruption, lumen irregularity, thrombus, and plaque classification were 1.000, 0.834, 0.918, and 0.913, respectively.
Statistical AnalysisAll statistical analyses were done using SPSS (version 18.0; SPSS Inc, Chicago, Illinois, United States). Categorical variables are expressed as counts and proportions and comparisons were performed with chi-square tests or the Fisher exact test. Continuous variables are presented as means ± standard deviation. Differences in the means of continuous measurements were examined using the independent-samples t-test and nonparametric Mann-Whitney U-test for 2-group comparisons. All P values were 2-sided with a statistical significance level of .05.
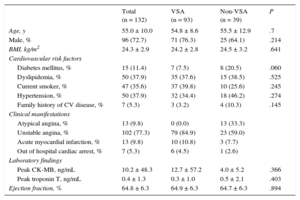
RESULTSPatient CharacteristicsAmong 183 patients with suspected VSA, the intracoronary ergonovine provocation test was performed in all but 21 patients who showed spontaneous spasm. Twelve patients with a positive ergonovine test were excluded due to poor OCT images, making it impossible to obtain an adequate interpretation. Among those with a negative ergonovine test, a total of 39 were excluded; 8 because of poor OCT images and 31 because of a normal coronary artery (stenosis diameter < 10%). Finally, 93 patients with spasm segments and 39 patients without spasm segments were included in the analysis (Figure 1). Baseline characteristics and risk factors are shown in Table 1. Mean age was 55.0 ± 10.0 years and 72.7% were male. Eleven patients had multivessel spasm, 37.9% had hypertension, 35.6% were current smokers, and 11.4% had diabetes mellitus. There were no significant differences in cardiovascular risk factors between the 2 groups.
Baseline Characteristics of Study Population
| Total (n = 132) | VSA (n = 93) | Non-VSA (n = 39) | P | |
|---|---|---|---|---|
| Age, y | 55.0 ± 10.0 | 54.8 ± 8.6 | 55.5 ± 12.9 | .7 |
| Male, % | 96 (72.7) | 71 (76.3) | 25 (64.1) | .214 |
| BMI, kg/m2 | 24.3 ± 2.9 | 24.2 ± 2.8 | 24.5 ± 3.2 | .641 |
| Cardiovascular risk factors | ||||
| Diabetes mellitus, % | 15 (11.4) | 7 (7.5) | 8 (20.5) | .060 |
| Dyslipidemia, % | 50 (37.9) | 35 (37.6) | 15 (38.5) | .525 |
| Current smoker, % | 47 (35.6) | 37 (39.8) | 10 (25.6) | .245 |
| Hypertension, % | 50 (37.9) | 32 (34.4) | 18 (46.2) | .274 |
| Family history of CV disease, % | 7 (5.3) | 3 (3.2) | 4 (10.3) | .145 |
| Clinical manifestations | ||||
| Atypical angina, % | 13 (9.8) | 0 (0.0) | 13 (33.3) | |
| Unstable angina, % | 102 (77.3) | 79 (84.9) | 23 (59.0) | |
| Acute myocardial infarction, % | 13 (9.8) | 10 (10.8) | 3 (7.7) | |
| Out of hospital cardiac arrest, % | 7 (5.3) | 6 (4.5) | 1 (2.6) | |
| Laboratory findings | ||||
| Peak CK-MB, ng/mL | 10.2 ± 48.3 | 12.7 ± 57.2 | 4.0 ± 5.2 | .366 |
| Peak troponin T, ng/mL | 0.4 ± 1.3 | 0.3 ± 1.0 | 0.5 ± 2.1 | .403 |
| Ejection fraction, % | 64.8 ± 6.3 | 64.9 ± 6.3 | 64.7 ± 6.3 | .894 |
BMI, body mass index; CK-MB, creatinine kinase-isoenzyme MB; CV, cardiovascular; VSA, vasospastic angina.
Values are expressed as No. (%) or mean ± standard deviation.
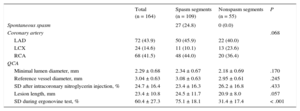
A total of 164 angiographic lesions were analyzed with quantitative coronary angiography and OCT. One hundred and nine were from spasm segments in VSA patients and 55 were from nonspasm segments in non-VSA patients. Angiographic lesion characteristics are listed in Table 2. Of the 109 spasm segments, 27 were spontaneous and 82 were provoked with ergonovine. Spasm segments were most frequent at the left anterior descending artery followed by the right coronary artery and left circumflex artery (45.9%, 44.0%, and 10.1%, respectively). Among the target lesions in non-VSA patients, 40.0% of lesions were located in the left anterior descending artery, 36.4%, in the right coronary artery, and 23.6% in the left circumflex artery. There was no difference in stenosis diameter after intracoronary nitroglycerin injection in spasm segments and nonspasm segments (23.4 ± 16.3% vs 26.2 ± 16.8%; P = .433). Maximal luminal narrowing during the ergonovine provocation test was higher at spasm segments than at nonspasm segments (75.1 ± 18.1% vs 31.4 ± 17.4%; P < .001).
Angiographic Characteristics of Spasm and Nonspasm Segments
| Total (n = 164) | Spasm segments (n = 109) | Nonspasm segments (n = 55) | P | |
|---|---|---|---|---|
| Spontaneous spasm | 27 (24.8) | 0 (0.0) | ||
| Coronary artery | .068 | |||
| LAD | 72 (43.9) | 50 (45.9) | 22 (40.0) | |
| LCX | 24 (14.6) | 11 (10.1) | 13 (23.6) | |
| RCA | 68 (41.5) | 48 (44.0) | 20 (36.4) | |
| QCA | ||||
| Minimal lumen diameter, mm | 2.29 ± 0.68 | 2.34 ± 0.67 | 2.18 ± 0.69 | .170 |
| Reference vessel diameter, mm | 3.04 ± 0.63 | 3.08 ± 0.63 | 2.95 ± 0.61 | .245 |
| SD after intracoronary nitroglycerin injection, % | 24.7 ± 16.4 | 23.4 ± 16.3 | 26.2 ± 16.8 | .433 |
| Lesion length, mm | 23.4 ± 10.8 | 24.5 ± 11.7 | 20.9 ± 8.0 | .057 |
| SD during ergonovine test, % | 60.4 ± 27.3 | 75.1 ± 18.1 | 31.4 ± 17.4 | < .001 |
SD, stenosis diameter; LAD, left anterior descending artery; LCX, left circumflex artery; RCA, right coronary artery; QCA, quantitative coronary angiography.
Values are presented as No. (%) and mean ± standard deviation.
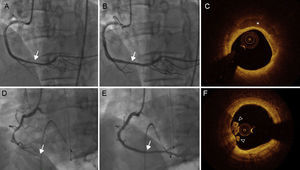
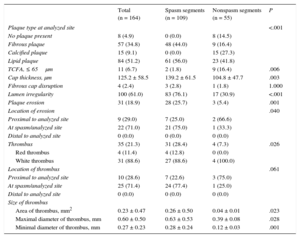
Optical coherence tomography findings are shown in Table 3. Thrombus was more frequently seen at spasm segments than at nonspasm segments (28.4% vs 7.3%; P = .026) with the majority being white thrombus for both groups. The size of thrombus was larger at spasm segments than at nonspasm segments (0.26 ± 0.50mm2 vs 0.04 ± 0.01mm2; P = .023). Among spasm segments, thrombus was most frequently located at spasm sites (77.4%) followed by upstream of spasm segments (22.6%). No thrombus was seen downstream of spasm segments in either group. Thrombus was found at 4 nonspasm segments in non-VSA patients. Fibrous cap disruption was found in both groups, at 3 spasm segments, and 1 nonspasm segment. Lumen irregularity was more common at spasm segments (76.1% vs 30.9%; P < .001). There were significant differences in plaque characteristics between spasm and nonspasm segments. A total of 44.0% of the spasm segments were composed of fibrous plaque, whereas 27.3% of the nonspasm segments had calcific plaque. No calcified plaque was seen in spasm segments. Thin-cap fibroatheroma was more frequently seen in nonspasm segments than in spasm segments (16.4% vs 1.8%; P = .006) and the maximal cap thickness was also smaller in nonspasm segments than in spasm segments (104.8 ± 47.7μm vs 139.2 ± 61.5μm; P = .001). Plaque erosion, however, was more common at spasm segments than at nonspasm segments (25.7% vs 5.4%; P = .001). A representative case of non-VSA and VSA is shown in Figure 2.
Optical Coherence Tomography Findings of Spasm and Nonspasm Segments
| Total (n = 164) | Spasm segments (n = 109) | Nonspasm segments (n = 55) | P | |
|---|---|---|---|---|
| Plaque type at analyzed site | <.001 | |||
| No plaque present | 8 (4.9) | 0 (0.0) | 8 (14.5) | |
| Fibrous plaque | 57 (34.8) | 48 (44.0) | 9 (16.4) | |
| Calcified plaque | 15 (9.1) | 0 (0.0) | 15 (27.3) | |
| Lipid plaque | 84 (51.2) | 61 (56.0) | 23 (41.8) | |
| TCFA, ≤ 65μm | 11 (6.7) | 2 (1.8) | 9 (16.4) | .006 |
| Cap thickness, μm | 125.2 ± 58.5 | 139.2 ± 61.5 | 104.8 ± 47.7 | .003 |
| Fibrous cap disruption | 4 (2.4) | 3 (2.8) | 1 (1.8) | 1.000 |
| Lumen irregularity | 100 (61.0) | 83 (76.1) | 17 (30.9) | <.001 |
| Plaque erosion | 31 (18.9) | 28 (25.7) | 3 (5.4) | .001 |
| Location of erosion | .040 | |||
| Proximal to analyzed site | 9 (29.0) | 7 (25.0) | 2 (66.6) | |
| At spasm/analyzed site | 22 (71.0) | 21 (75.0) | 1 (33.3) | |
| Distal to analyzed site | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Thrombus | 35 (21.3) | 31 (28.4) | 4 (7.3) | .026 |
| Red thrombus | 4 (11.4) | 4 (12.8) | 0 (0.0) | |
| White thrombus | 31 (88.6) | 27 (88.6) | 4 (100.0) | |
| Location of thrombus | .061 | |||
| Proximal to analyzed site | 10 (28.6) | 7 (22.6) | 3 (75.0) | |
| At spasm/analyzed site | 25 (71.4) | 24 (77.4) | 1 (25.0) | |
| Distal to analyzed site | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Size of thrombus | ||||
| Area of thrombus, mm2 | 0.23 ± 0.47 | 0.26 ± 0.50 | 0.04 ± 0.01 | .023 |
| Maximal diameter of thrombus, mm | 0.60 ± 0.50 | 0.63 ± 0.53 | 0.39 ± 0.08 | .028 |
| Minimal diameter of thrombus, mm | 0.27 ± 0.23 | 0.28 ± 0.24 | 0.12 ± 0.03 | .001 |
TCFA, thin-cap fibroatheroma.
Values are presented as No. (%) or mean ± standard deviation.
Coronary angiography and OCT images of a representative case of nonvasospastic angina (A, B and C) and vasospastic angina (D, E and F). Coronary angiography shows nonsignificant stenosis in the dRCA, which was diagnosed as non-VSA after intracoronary ergonovine injection (A) and nitroglycerin (B). C: OCT revealed superficial calcium (asterisk) on plaque without evidence of thrombus. D: Intracoronary ergonovine injection resulted in complete occlusion of the dRCA. E: This normalized with 200μg of intracoronary nitroglycerine administration. F: OCT revealed a protruding mass into the lumen of white thrombus (arrow head) with an intact fibrous cap and an irregular luminal surface. dRCA, distal portion of the right coronary artery; OCT, optical coherence tomography.
This study aimed to evaluate the incidence of thrombus and plaque characteristics at coronary spasm segments compared with nonspasm segments by using OCT. The major findings are: a) thrombus was more frequently observed at spasm segments than at nonspasm segments; b) thrombus was mainly located at the site of spasm followed by upstream of the spasm segment, with no thrombus observed downstream of the spasm segment, and c) plaque erosion was more common at spasm segments than at nonspasm segments.
In this study, spasm was associated with more frequent thrombus formation and plaque erosion. The acute disturbance of blood flow caused by acute vascular narrowing induces endothelial damage or erosive injury to plaque with consequent thrombus formation.14 In an animal study using electron microscopy, a 40% to 60% reduction in the luminal diameter of the left anterior descending coronary arteries (by 1 hour partial ligation resulting in no substantial change in the rate of distal blood flow) resulted in endothelial denudation, platelet deposition, and thrombus formation in areas proximal to the point of maximum constriction.7 In a further animal study, the sites of provoked spasm showed intimal injuries (up to 60.9%) in the form of endothelial cell protrusions, denudation, and macrophage extravasation.15 It was suggested that vasospasm contributed to both superficial plaque injury and thrombus formation. The interaction of platelets with the damaged vessel wall and the ensuing reaction might further potentiate the coronary spasm.6 In a recent study performed by our group, the morphological features of 80 coronary artery spasm sites from patients with confirmed VSA were investigated using OCT, and 26% of the spasm sites had plaque erosion with thrombus present.8 The causal relationship between spasm and thrombus cannot be explained entirely by our study. However, to our knowledge, this is the first study to demonstrate that, despite the similar degree of stenosis diameter, spasm sites more frequently had thrombus than nonspasm sites.
Wall shear stress is one of the parameters of force that directly acts on the vascular luminal surface. Low-magnitude wall shear stress tends to be present in regions where plaques form, whereas higher magnitudes of wall shear stress are atheroprotective, as long as the magnitude is below the threshold that causes endothelial damage (typically when > 70 dynes/cm2) or acute denudation (around 400 dynes/cm2).7,16,17 In addition, high shear stress activates von Willebrand factor resulting in platelet adhesion.18 It is well established that von Willebrand factor plays an important role in platelet adhesion and aggregation under high blood-flow velocity conditions observed in stenotic atherosclerotic arteries.19 Given these relationships and the fact that solid mechanics alone have not explained why certain plaques suddenly form thrombus and plaque erosion, the role of fluid mechanics in vasospasm warrants consideration. In the present study, although the stenosis diameter after intracoronary nitroglycerin injection in spasm segments and nonspasm segments showed no difference, thrombus was more frequently seen at spasm segments than at nonspasm segments, suggesting that the high shear stress transiently induced by vasospasm may have contributed to thrombus formation. Plaque erosion is the formation of thrombus over an atherosclerotic plaque without rupture of the fibrous cap, and the surface endothelium beneath the thrombus is usually absent.20,21 Vasospasm is known to be a cause of endothelial damage and may thus be involved in the pathophysiology of erosion.20,21 Even with the identification of plaque erosion, the exact mechanism responsible for thrombus formation is not known.3 In histological studies, endothelial cells tend to be apoptotic or absent at the site of erosion, suggesting that denudation has occurred.22,23
Although thrombotic events, such as acute coronary syndrome, commonly arise from thin-cap fibroatheroma, thrombus in VSA arises from specific types of atherosclerotic plaques, mainly early and stable plaque in nonobstructed lesions. Our results suggest that coronary spasm may cause myocardial ischemia by endothelial damage and thrombus formation, which may occur on stable plaque at the site of spasm.
Although thrombus and plaque erosion were more common at spasm segments than at nonspasm segments, all spasm segments failed to show thrombus in similar high wall shear stress environments. Therefore, research is needed to investigate the mechanisms that can influence thrombus formation through various internal and external modifiers both locally and systemically. Specifically, we need to understand and potentially be able to predict thrombus formation occurring with atherosclerotic plaque alterations.
There is no consensus on the use of antiplatelet therapies for VSA. Although thrombus size complicated by plaque erosion is considered to be small in VSA, prolonged vasospasm may risk the development of a large thrombus resulting in acute myocardial infarction in VSA patients. Based on our findings, this study suggests the potential benefit and treatment role of not only vasodilating drugs but also antiplatelet therapy in VSA. Recent studies have also proposed the use of cilostazol for the treatment of VSA.24 In our published STELLA trial,25 patients with VSA were randomized to receive cilostazol in addition to amlodipine with significant improvement in angina frequency and intensity. In addition to vasodilatory properties, cilostazol also has antiplatelet actions, which may prevent thrombotic complications. However, the effect of cilostazol on VSA should be investigated in randomized controlled trials; in addition, more studies are needed that focus on the use of agents with antiplatelet properties in VSA patients.
LimitationsThis study has some limitations. First, selection bias may have occurred in individual cases. Although patients with suspected VSA and the same degree of angiographic stenosis were enrolled, normal coronary arteries were excluded from the control group excluded. In our opinion, this was justified, as it is impractical to perform OCT in these non-VSA patients with normal coronary arteries. Additionally, previous data have shown that VSA lesions have insignificant coronary stenosis but mild stenosis diameter26 (26% ± 10%), which was similar in both groups in our study population. Second, vasospasm should be considered in patients who have used cocaine, but it is strictly prohibited by law in Korea and cannot be purchased by individuals. Therefore, a drug test for cocaine is not usually performed, and was not performed in this study. Third, because OCT was performed after a spasm provocation test or spontaneous spasm, it is theoretically possible that thrombus might have increased or appeared with the coronary artery spasm. Fourth, there is uncertainty about the cause-effect relationship between the occurrence of vasospasm and denudation of the endothelium, followed by thrombus formation. In other words, denudation of the endothelium with or without thrombus formation may have caused the vasospasm. Fifth, erosion is beyond the resolution of OCT. Therefore, plaque erosion was defined as the presence of attached thrombus overlying an intact fibrous cap by OCT. Thrombus at the spasm site is different from that of acute coronary syndrome. As most of them were white thrombus and the size was small, no underlying plaque could be identified in any of the patients. Last, the number of patients included was relatively small. However, this study used highly sensitive techniques that allowed accurate assessment of plaque morphology and thrombus.
CONCLUSIONSOur results show that thrombus and plaque erosion are common OCT findings at spasm segments compared with nonspasm segments in patients with suspected VSA. Transient high shear stress caused by stenosis induced by vasospasm may play an important role in the formation of thrombus and plaque erosion in patients with VSA. These findings suggest the potential benefit and treatment role not only of vasodilating drugs but also of antiplatelet therapy in VSA.
AknowledgementsThe authors wish to thank Eok-Rae Cho and Jin-Hee Lee for their efforts in analyzing the coronary angiography and collection of quantitative coronary angiography data.
CONFLICTS OF INTERESTT. Akasaka has received research grants from Abbott Vascular Japan, St. Jude Medical Japan, Goodman Inc., Terumo Inc., and Daiichi-Sankyo Pharmaceutical Co.; and has served on the advisory boards of St. Jude Medical Japan and Terumo Inc. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
- –
Thrombus and plaque erosion defined by OCT are commonly observed at the site of coronary artery spasm in patients with VSA.
- –
This study evaluated the incidence of thrombus and plaque characteristics at coronary spasm segments compared with nonspasm segments in patients with suspected VSA by using OCT.
- –
In this study, we were able to provide evidence that thrombus and plaque erosion were more prevalent at spasm segments than at nonspasm segments.
- –
These findings suggest the potential benefit and treatment role of antiplatelet therapy in VSA.