It is uncertain whether side branch predilatation before main vessel stenting is necessary. We evaluated the effect of side branch predilatation on outcomes in percutaneous coronary intervention for true nonleft main bifurcation determined by the Medina classification using the provisional approach.
MethodsTarget vessel failures (composite of cardiac death, myocardial infarction, or target vessel revascularization) were compared between patients who underwent side branch predilatation (predilatation group, n = 175) and those who did not (nonpredilatation group, n = 662).
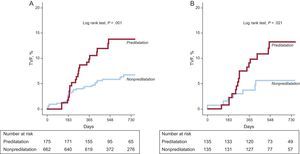
ResultsFinal kissing-balloon inflation (57.1% vs 35.8%; P < .001) was performed more frequently and the cross-over rate to a 2-stent technique (14.9% vs 5.1%; P < .001) was higher in the predilatation group. During a median follow-up of 21 months, the predilatation group had a higher incidence of target vessel failures (14.3% vs 6.8%; P = .002) and target vessel revascularization (12.0% vs 5.6%; P = .003), but not of cardiac death or myocardial infarction compared with the nonpredilatation group. On multivariate analysis, side branch predilatation was associated with a higher occurrence of target vessel failures (adjusted hazard ratio = 2.11; 95% confidence interval, 1.27-3.50; P = .004). These results remained consistent after a propensity score-matched population analysis (for target vessel failures, adjusted hazard ratio = 2.63; 95% confidence interval, 1.09-6.34; P = .0031) and they were also constant among the various subgroups, according to the bifurcation angle, calcification, and diameter stenosis of the side branch.
ConclusionsSide branch predilatation before main vessel stenting may be associated with an increased risk of repeat revascularization in patients with true nonleft main bifurcation treated by the provisional approach.
Trial registration: ClinicalTrials.gov number: NCT00851526.
Keywords
Based on the results of numerous randomized trials, the provisional approach of selective side branch (SB) intervention after main vessel stenting is now considered the first-line treatment for most bifurcation lesions.1–5 However, it is unclear whether predilatation of a SB before main vessel stenting can improve procedural and clinical outcomes in percutaneous coronary intervention (PCI) for a bifurcation lesion using the provisional approach. The aim of the present study was to assess the impact of SB predilatation before main vessel stenting on procedural and long-term clinical outcomes in patients with true nonleft main coronary bifurcation lesions, using a large, dedicated bifurcation registry.
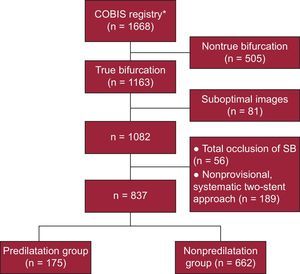
METHODSStudy PopulationThe COBIS6,7 registry is a retrospective multicenter registry of patients with coronary bifurcation lesions undergoing PCI with drug-eluting stents. A total of 1668 consecutive patients from 16 major coronary intervention centers in South Korea were enrolled between January 2004 and June 2006. Details of the COBIS registry have previously been published and the registry has been used for other retrospective analyses.6,7
To assess the effect of SB predilatation before main vessel stenting on procedural and clinical outcomes, we selected 1163 patients with true nonleft main bifurcation, as determined by the Medina classification.8 Eighty-one patients were excluded due to suboptimal images that were insufficient to evaluate SB predilatation. Of the remaining patients (n = 1082), 245 were excluded; 56 patients were excluded due to the presence of total SB occlusion on the preprocedural evaluation; we also excluded 189 patients who underwent a nonprovisional, 22-stent procedure of the SB. A total of 837 patients were finally included in this study (Figure 1).
Percutaneous Coronary InterventionAll patients were prescribed acetylsalicylic acid (300mg) and clopidogrel (300 or 600mg) unless these antiplatelet medications had previously been administered. Decisions to perform SB predilatation, the 2-stent procedure, or final kissing-balloon inflation were made by the individual operators.
Data Collection and Angiographic AnalysisDemographic, clinical, angiographic, procedural, and outcome data were collected with the use of a web-based reporting system. Additional information was obtained from the medical records or by telephone contact, if necessary. All outcome data reported from the participating center were reviewed by an independent clinical event adjudicating committee. Angiographic and procedural characteristics of all cine-angiograms were reviewed and analyzed at the angiographic core laboratory (Cardiac and Vascular Center, Samsung Medical Center, Seoul, South Korea) with an automated edge-detection system (Centricity CA1000, GE; Waukesha, Wisconsin, United States) using standard definitions.9,10
Bifurcation lesions were classified according to the Medina classification.8 Medina classification (1,1,1), (1,0,1) or (0,1,1) lesions were categorized as true bifurcation lesions. For quantitative coronary angiographic analysis, bifurcation lesions were divided into 8 segments (Figure 1 of supplementary material).11 For the main vessel, the reference diameter was defined as the average of the proximal and distal reference lumen diameters. For the SB, the reference diameter was the distal reference lumen diameter.
Study Outcomes and DefinitionsThe primary objective of this study was to compare the incidence of target vessel failure (TVF) in patients treated with or without predilatation of the SB before main vessel stenting. Target vessel failure was defined as the composite of cardiac death, myocardial infarction, or target vessel revascularization (TVR). Clinical events were defined based on the recommendations of the Academic Research Consortium.12 The bifurcation angle was defined as the angle between the axis of the main vessel and the axis of the SB at its origin. The diameter of the stenosis in the SB ostium was calculated by the following equation: 100 × (reference diameter of distal SB – minimum lumen diameter of SB ostium) / reference diameter of distal SB. Calcifications were identified as apparent radio-opacities within the vascular wall at the site of the stenosis and were classified as moderate (radio-opacities noted only during the cardiac cycle before the contrast injection) or severe (radio-opacities noted without cardiac motion before the contrast injection and generally compromising both sides of the arterial lumen).13 We defined PCI-related acute closure as the development of Thrombolysis In Myocardial Infarction flow grade < 3 during the index procedure. Angiographic success was defined as the achievement of Thrombolysis In Myocardial Infarction 3 flow with a final residual stenosis < 30% for the main vessel or < 50% for the SB. Procedural success was defined as angiographic success without major adverse cardiac events during the hospital stay. Periprocedural myocardial infarction was defined as a rise in the creatine kinase-myocardial band ≥ 3 times the upper limit of normal after the index PCI. The periprocedural period included the first 48h after the PCI, and periprocedural myocardial infarction was not considered to be a primary endpoint in our study.
Statistical AnalysisContinuous variables are presented as means (standard deviations) or medians [interquartile ranges]. Categorical variables are presented as frequencies with percentages. Continuous variables were analyzed using the independent sample Student t test or the Mann-Whitney test, and categorical variables were analyzed with the chi-square test or Fisher's exact test. Cumulative event rates were estimated using Kaplan-Meier methods and were compared by the log rank test. The Cox proportional hazards model was used to identify independent predictors of individual outcomes. The covariates that were statistically significant on univariate analysis (P <.05) and/or those that were clinically relevant were considered candidate variables in the multivariate models. The following variables were selected for analysis of TVF with the Cox proportional hazards model: diabetes mellitus, acute coronary syndrome as a presentation, creatinine, bifurcation angle, diameter stenosis of the SB ostium, lesion length of the SB, moderate to severe calcification in the SB, type of drug-eluting stent, total stent length in the main vessel, final kissing-balloon inflation, and predilatation of the SB before main vessel stenting.
To reduce treatment-selection bias for predilatation of the SB and potential confounding factors, we performed rigorous adjustments for the baseline characteristics of the patients using their propensity scores. The propensity scores were estimated using multiple logistic-regression analysis. A full nonparsimonious model was developed that included almost all of the variables listed in Tables 1 and 2, and baseline quantitative coronary angiographic data in Table 3. The discrimination and calibration abilities of the propensity score model were assessed with c-statistics and the Hosmer-Lemeshow statistic. We assessed the balance in baseline covariates between the 2 groups in a propensity score-matched population. We compared the continuous variables with paired Student t test or the Mann-Whitney test as appropriate, and categorical variables with McNemar's or Bhapkar's tests of symmetry, as appropriate. In the propensity score-matched population, hazard ratios (HRs) for outcomes were compared by a stratified Cox regression model. Statistical significance was accepted for a 2-sided P value <.05. All analyses were performed using a SAS (Statistical Analysis System) version 9.1 package (SAS Institute; Cary, North Carolina, United States).
Baseline Clinical Characteristics
| Overall (n = 837) | Propensity (n = 270) | |||||
| Predilatation of SB (+)(n = 175) | Predilatation of SB (–)(n = 662) | P | Predilatation of SB (+)(n = 135) | Predilatation of SB (–)(n = 135) | P | |
| Age, mean (SD), y | 62.1 (10.6) | 62.6 (10.2) | .57 | 63.2 (9.9) | 62.3 (10.0) | .48 |
| Female sex | 57 (32.6) | 218 (32.9) | .93 | 45 (33.3) | 37 (27.4) | .37 |
| Diabetes mellitus | 40 (22.9) | 210 (31.7) | .023 | 29 (21.5) | 28 (20.7) | .88 |
| Hypertension | 105 (60.0) | 396 (59.8) | .97 | 83 (61.5) | 79 (58.5) | .72 |
| Current smoking | 44 (25.1) | 167 (25.2) | .98 | 37 (27.4) | 38 (28.2) | .89 |
| Chronic renal failure | 7 (4.0) | 21 (3.2) | .59 | 5 (3.7) | 3 (2.2) | .48 |
| Prior myocardial infarction | 17 (9.7) | 50 (7.6) | .35 | 11 (8.2) | 13 (9.6) | .68 |
| Acute coronary syndrome | 99 (56.6) | 380 (57.4) | .84 | 73 (54.1) | 70 (51.9) | .81 |
| Creatinine, mean (SD), mg/dL | 1.15 (1.24) | 1.15 (1.48) | .99 | 1.19 (1.40) | 1.04 (0.50) | .25 |
| Left ventricular ejection fraction, mean (SD), % | 59.6 (11.5) | 59.5 (11.6) | .94 | 60.4 (10.1) | 59.9 (9.2) | .69 |
| Dual antiplatelet therapy, mean (SD), months | 15.3 (10.5) | 14.3 (9.7) | .25 | 14.3 (10.8) | 12.7 (9.0) | .17 |
| Follow-up duration, mean (SD), days | 719 (345) | 729 (357) | .74 | 707 (336) | 714 (332) | .87 |
SB, side branch; SD, standard deviation. Data are expressed as No. (%) or mean (standard deviation).
Baseline Angiographic and Periprocedural Data
| Overall (n = 837) | Propensity (n = 270) | |||||
| Predilatation of SB (+)(n = 175) | Predilatation of SB (–)(n = 662) | P | Predilatation of SB (+)(n = 135) | Predilatation of SB (–)(n = 135) | P | |
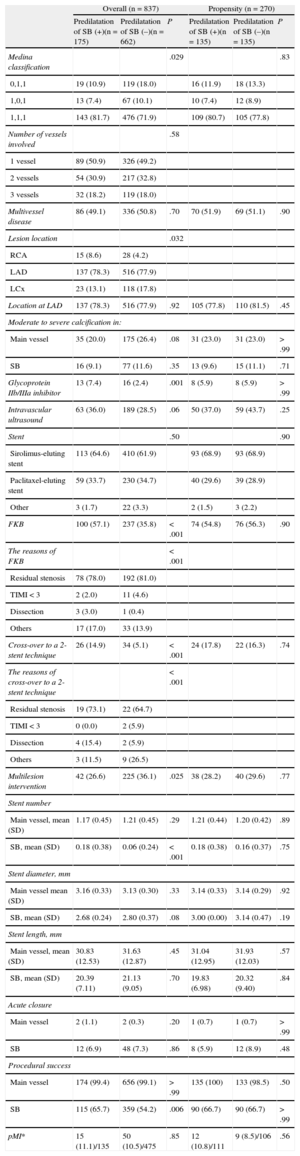
| Medina classification | .029 | .83 | ||||
| 0,1,1 | 19 (10.9) | 119 (18.0) | 16 (11.9) | 18 (13.3) | ||
| 1,0,1 | 13 (7.4) | 67 (10.1) | 10 (7.4) | 12 (8.9) | ||
| 1,1,1 | 143 (81.7) | 476 (71.9) | 109 (80.7) | 105 (77.8) | ||
| Number of vessels involved | .58 | |||||
| 1 vessel | 89 (50.9) | 326 (49.2) | ||||
| 2 vessels | 54 (30.9) | 217 (32.8) | ||||
| 3 vessels | 32 (18.2) | 119 (18.0) | ||||
| Multivessel disease | 86 (49.1) | 336 (50.8) | .70 | 70 (51.9) | 69 (51.1) | .90 |
| Lesion location | .032 | |||||
| RCA | 15 (8.6) | 28 (4.2) | ||||
| LAD | 137 (78.3) | 516 (77.9) | ||||
| LCx | 23 (13.1) | 118 (17.8) | ||||
| Location at LAD | 137 (78.3) | 516 (77.9) | .92 | 105 (77.8) | 110 (81.5) | .45 |
| Moderate to severe calcification in: | ||||||
| Main vessel | 35 (20.0) | 175 (26.4) | .08 | 31 (23.0) | 31 (23.0) | > .99 |
| SB | 16 (9.1) | 77 (11.6) | .35 | 13 (9.6) | 15 (11.1) | .71 |
| Glycoprotein IIb/IIIa inhibitor | 13 (7.4) | 16 (2.4) | .001 | 8 (5.9) | 8 (5.9) | > .99 |
| Intravascular ultrasound | 63 (36.0) | 189 (28.5) | .06 | 50 (37.0) | 59 (43.7) | .25 |
| Stent | .50 | .90 | ||||
| Sirolimus-eluting stent | 113 (64.6) | 410 (61.9) | 93 (68.9) | 93 (68.9) | ||
| Paclitaxel-eluting stent | 59 (33.7) | 230 (34.7) | 40 (29.6) | 39 (28.9) | ||
| Other | 3 (1.7) | 22 (3.3) | 2 (1.5) | 3 (2.2) | ||
| FKB | 100 (57.1) | 237 (35.8) | < .001 | 74 (54.8) | 76 (56.3) | .90 |
| The reasons of FKB | < .001 | |||||
| Residual stenosis | 78 (78.0) | 192 (81.0) | ||||
| TIMI < 3 | 2 (2.0) | 11 (4.6) | ||||
| Dissection | 3 (3.0) | 1 (0.4) | ||||
| Others | 17 (17.0) | 33 (13.9) | ||||
| Cross-over to a 2-stent technique | 26 (14.9) | 34 (5.1) | < .001 | 24 (17.8) | 22 (16.3) | .74 |
| The reasons of cross-over to a 2-stent technique | < .001 | |||||
| Residual stenosis | 19 (73.1) | 22 (64.7) | ||||
| TIMI < 3 | 0 (0.0) | 2 (5.9) | ||||
| Dissection | 4 (15.4) | 2 (5.9) | ||||
| Others | 3 (11.5) | 9 (26.5) | ||||
| Multilesion intervention | 42 (26.6) | 225 (36.1) | .025 | 38 (28.2) | 40 (29.6) | .77 |
| Stent number | ||||||
| Main vessel, mean (SD) | 1.17 (0.45) | 1.21 (0.45) | .29 | 1.21 (0.44) | 1.20 (0.42) | .89 |
| SB, mean (SD) | 0.18 (0.38) | 0.06 (0.24) | < .001 | 0.18 (0.38) | 0.16 (0.37) | .75 |
| Stent diameter, mm | ||||||
| Main vessel mean (SD) | 3.16 (0.33) | 3.13 (0.30) | .33 | 3.14 (0.33) | 3.14 (0.29) | .92 |
| SB, mean (SD) | 2.68 (0.24) | 2.80 (0.37) | .08 | 3.00 (0.00) | 3.14 (0.47) | .19 |
| Stent length, mm | ||||||
| Main vessel, mean (SD) | 30.83 (12.53) | 31.63 (12.87) | .45 | 31.04 (12.95) | 31.93 (12.03) | .57 |
| SB, mean (SD) | 20.39 (7.11) | 21.13 (9.05) | .70 | 19.83 (6.98) | 20.32 (9.40) | .84 |
| Acute closure | ||||||
| Main vessel | 2 (1.1) | 2 (0.3) | .20 | 1 (0.7) | 1 (0.7) | > .99 |
| SB | 12 (6.9) | 48 (7.3) | .86 | 8 (5.9) | 12 (8.9) | .48 |
| Procedural success | ||||||
| Main vessel | 174 (99.4) | 656 (99.1) | > .99 | 135 (100) | 133 (98.5) | .50 |
| SB | 115 (65.7) | 359 (54.2) | .006 | 90 (66.7) | 90 (66.7) | > .99 |
| pMI* | 15 (11.1)/135 | 50 (10.5)/475 | .85 | 12 (10.8)/111 | 9 (8.5)/106 | .56 |
FKB, final kissing ballooning; LAD, left anterior descending coronary artery; LCX, left circumflex; pMI, peri-procedural myocardial infarction; RCA, right coronary artery; SB, side branch; SD, standard deviation; TIMI: Thrombolysis In Myocardial Infarction.
Data are expressed as No. (%) or mean (standard deviation).
*Was just evaluated in 610 of overall and 216 of propensity score-matched populations.
Quantitative Coronary Angiographic Data
| Overall (n = 837) | Propensity (n = 270) | |||||
| Predilatation of SB (+)(n = 175) | Predilatation of SB (–)(n = 662) | P | Predilatation of SB (+)(n = 135) | Predilatation of SB (–)(n = 135) | P | |
| Bifurcation angle, mean SD), (°) | 51.5 (16.0) | 52.7 (17.6) | .41 | 51.2 (16.6) | 51.3 (16.4) | .99 |
| Pre-procedural MLD, mean (SD), mm | ||||||
| Main vessel, proximal | 1,26 (0.71) | 1.43 (0.77) | .007 | 1.29 (0.70) | 1.32 (0.76) | .75 |
| Main vessel, middle | 1.15 (0.62) | 1.27 (0.59) | .02 | 1.16 (0.63) | 1.18 (0.57) | .75 |
| Main vessel, distal | 1.67 (0.72) | 1.56 (0.68) | .06 | 1.66 (0.71) | 1.59 (0.62) | .43 |
| SB, ostial | 0.86 (0.41) | 1.15 (0.48) | < .001 | 0.91 (0.42) | 0.90 (0.36) | .74 |
| SB, distal | 1.47 (0.54) | 1.50 (0.53) | .55 | 1.47 (0.54) | 1.42 (0.53) | .40 |
| Preprocedural DS in SB ostium, mean (SD), % | 58 (18) | 44 (20) | < .001 | 56 (18) | 57 (16) | .83 |
| Preprocedural lesion length in SB, mean (SD) mm | 6.46 (5.61) | 6.32 (6.25) | .79 | 6.64 (5.96) | 7.25 (6.25) | .35 |
| Final MLD, mean (SD), mm | ||||||
| Main vessel, proximal | 2.90 (0.55) | 2.79 (0.51) | .016 | 2.90 (0.57) | 2.84 (0.59) | .28 |
| Main vessel, middle | 2.65 (0.52) | 2.63 (0.48) | .52 | 2.67 (0.53) | 2.65 (0.57) | .83 |
| Main vessel, distal | 2.61 (0.55) | 2.53 (0.52) | .06 | 2.63 (0.56) | 2.60 (0.54) | .70 |
| SB, ostial | 1.43 (0.63) | 1.23 (0.58) | < .001 | 1.41 (0.63) | 1.39 (0.67) | .77 |
| SB, distal | 1.73 (0.56) | 1.56 (0.58) | .001 | 1.73 (0.55) | 1.65 (0.64) | .25 |
| Final DS in SB ostium, mean (SD), % | 34 (25) | 41 (24) | .001 | 36 (24) | 35 (24) | .81 |
DS, diameter stenosis; MLD, minimal luminal diameter; SB, side branch; SD, standard deviation.
Data are expressed as mean (standard deviation).
Predilatation of the SB before main vessel stenting was performed in 175 (20.9%) patients. The baseline clinical characteristics were not significantly different between the groups, except for the proportion of patients with diabetes (Table 1). Table 2 shows the angiographic and periprocedural data. The Medina classification differed significantly between the groups (P = .029). Final kissing-balloon inflation was performed more frequently, and the rate of cross-over to a 2-stent technique was higher in the predilatation group. Thus, the procedural success rate for SB was higher in the predilatation group, even though there were no significant differences in the rate of PCI-related acute closure in the main vessel or SB. In addition, the incidence of periprocedural myocardial infarction was also not decreased in the predilatation group (11.1% vs 10.5%, adjusted odds ratio = 1.05; 95% confidence interval [95%CI], 0.42-2.60; P = .92).
Quantitative Coronary Angiographic DataThe quantitative coronary angiographic data are shown in Table 3.
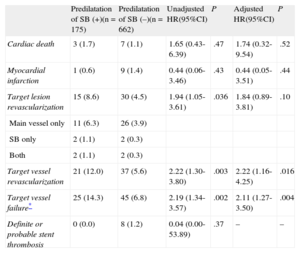
Clinical OutcomesComplete clinical follow-up data were obtained for all patients included in the present study. There was no significant difference in the duration of follow-up between the groups (Table 1). During a median follow-up of 21 months (interquantile range, 14-31 months), there were 45 (5.4%) cases of target lesion revascularization and 70 (8.4%) cases of TVF. In total, 82.2% (37 of 45) of target lesion revascularization were performed at the main vessel, 8.9% at the SB, and the remaining 8.9% at both the main vessel and SB in the overall population, respectively. The incidence of TVF was significantly higher in the predilatation group, a difference driven primarily by the higher TVR rate in the predilatation group (Table 4 and Figure 2A). However, the rates of cardiac death, myocardial infarction, and stent thrombosis were not significantly different between the groups. On multivariate analysis, the predilatation group had a significantly higher likelihood of adjusted TVF and TVR.
Long-term Clinical Outcomes in the Overall Population
| Predilatation of SB (+)(n = 175) | Predilatation of SB (–)(n = 662) | Unadjusted HR(95%CI) | P | Adjusted HR(95%CI) | P | |
| Cardiac death | 3 (1.7) | 7 (1.1) | 1.65 (0.43-6.39) | .47 | 1.74 (0.32-9.54) | .52 |
| Myocardial infarction | 1 (0.6) | 9 (1.4) | 0.44 (0.06-3.46) | .43 | 0.44 (0.05-3.51) | .44 |
| Target lesion revascularization | 15 (8.6) | 30 (4.5) | 1.94 (1.05-3.61) | .036 | 1.84 (0.89-3.81) | .10 |
| Main vessel only | 11 (6.3) | 26 (3.9) | ||||
| SB only | 2 (1.1) | 2 (0.3) | ||||
| Both | 2 (1.1) | 2 (0.3) | ||||
| Target vessel revascularization | 21 (12.0) | 37 (5.6) | 2.22 (1.30-3.80) | .003 | 2.22 (1.16-4.25) | .016 |
| Target vessel failure* | 25 (14.3) | 45 (6.8) | 2.19 (1.34-3.57) | .002 | 2.11 (1.27-3.50) | .004 |
| Definite or probable stent thrombosis | 0 (0.0) | 8 (1.2) | 0.04 (0.00-53.89) | .37 | – | – |
95%CI, 95%, confidence interval; HR, hazard ratio; SB, side branch.
Unless otherwise indicated, data are expressed as No. (%).
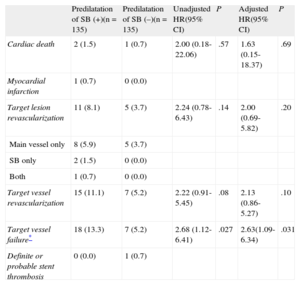
After performing propensity score matching, a total of 135 matched pairs were generated. The c-statistic for the propensity score model was 0.790, indicating acceptable discrimination. There were no significant differences in the baseline clinical, angiographic, and procedural characteristics for the propensity score-matched population (Tables 1 and 2). The incidence of periprocedural myocardial infarction was similar between the groups (adjusted odds ratio = 1.71; 95%CI, 0.16-18.26; P = .66). Table 3 demonstrates the quantitative coronary angiographic data from the propensity score-matched population.
A total of 25 TVFs occurred during a median follow-up of 21 months in the matched population. The predilatation group was associated with significantly worse outcomes in the matched population (Table 5 and Figure 2B). Although there were no significant differences in the incidence of cardiac death or myocardial infarction between the groups, patients in the predilatation group had significantly higher rates of target lesion revascularization, TVR, and TVF. In the multivariate analysis, using the baseline SB diameter stenosis as a covariate, the predilatation group still showed a significantly higher incidence of adjusted TVF.
Long-term Clinical Outcomes in the Propensity Score-matched Population
| Predilatation of SB (+)(n = 135) | Predilatation of SB (–)(n = 135) | Unadjusted HR(95% CI) | P | Adjusted HR(95% CI) | P | |
| Cardiac death | 2 (1.5) | 1 (0.7) | 2.00 (0.18-22.06) | .57 | 1.63 (0.15-18.37) | .69 |
| Myocardial infarction | 1 (0.7) | 0 (0.0) | ||||
| Target lesion revascularization | 11 (8.1) | 5 (3.7) | 2.24 (0.78-6.43) | .14 | 2.00 (0.69-5.82) | .20 |
| Main vessel only | 8 (5.9) | 5 (3.7) | ||||
| SB only | 2 (1.5) | 0 (0.0) | ||||
| Both | 1 (0.7) | 0 (0.0) | ||||
| Target vessel revascularization | 15 (11.1) | 7 (5.2) | 2.22 (0.91-5.45) | .08 | 2.13 (0.86-5.27) | .10 |
| Target vessel failure* | 18 (13.3) | 7 (5.2) | 2.68 (1.12-6.41) | .027 | 2.63(1.09-6.34) | .031 |
| Definite or probable stent thrombosis | 0 (0.0) | 1 (0.7) |
CI, confidence interval; HR, hazard ratio; SB, side branch.
Unless otherwise indicated, data are expressed as No. (%).
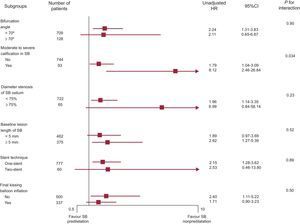
To determine whether the increased TVF risk for SB predilatation observed in the overall population was consistent, we compared the HR of SB predilatation for TVF in various important subgroups (bifurcation angle < 70° vs ≥ 70°, moderate to severe calcification in SB, diameter of the stenosis of the SB ostium < 75% vs ≥ 75%, baseline lesion length in the SB < 5mm vs ≥ 5mm, 1-stent technique, and final kissing-balloon inflation). The TVF rate was consistently higher in the predilatation group across all the specified subgroups (Figure 3). Moreover, there was a significant interaction between predilatation of the SB and moderate to severe calcification in the SB. The predilatation group had a much higher rate of TVF among patients with moderate to severe calcification, as well as among those without moderate to severe calcification.
In addition, we further analyzed the adjusted HR of SB predilatation in several specific cohorts. Among patients in the cohort that did not undergo final kissing-balloon inflation, there was a borderline significant tendency toward a higher adjusted TVF rate in the predilatation group (adjusted HR = 2.16; 95%CI, 0.99-4.72; P = .054). In addition, SB predilatation was still found to be a significant risk factor of adjusted TVF in the patient cohort treated with a 1-stent technique (adjusted HR = 2.02; 95%CI, 1.18–3.44; P = .01).
DISCUSSIONThe present analysis represents the first investigation of the impact of SB predilatation before main vessel stenting on procedural and long-term clinical outcomes using a large dedicated bifurcation registry. We found that final kissing-balloon inflation was performed more frequently and that the cross-over rate to a 2-stent technique was higher in the predilatation group. Thus, the procedural success rate for SB was higher in the predilatation group than in the nonpredilatation group, even though there was no difference in the occurrences of acute closure of the SB and periprocedural myocardial infarction between the predilatation and nonpredilatation groups. However, SB predilatation increased the long-term risk of adjusted TVF, mainly as a result of an increased risk of TVR. In addition, no considerable differences were observed in the rates of cardiac death, myocardial infarction, or stent thrombosis between the groups.
Although the 1-stent technique with a provisional SB approach is simple and is now regarded as the gold standard technique for most bifurcation lesions,1–5 an optimal method has not yet been established, and therefore new techniques have been introduced.14 In particular, however, no study has determined whether SB predilatation before main vessel stenting benefits patients with true nonleft main bifurcation lesions treated with drug-eluting stents. Theoretically, SB predilatation may scaffold the origin of the SB, thus retaining access to the SB after main vessel stenting. In the present study, the rate of procedural success for SB was higher in the predilatation group, even though other procedural outcomes were similar between the groups. However, long-term clinical outcomes were worse in the SB predilatation group.
Side branch predilatation may lead to dissection of the SB and increase the risk of recrossing the more proximal strut through a dissection plane, which, in turn, would increase the chance of potentially unnecessary kissing-balloon inflation and/or SB stenting.15 Because of the second intervention, such as kissing balloon inflation and/or SB stenting after main vessel stenting, immediate postprocedural outcomes were better in the predilatation group than in the nonpredilatation group. In the present study, the procedural success rate for SB was higher in the predilatation group than in the nonpredilatation group. The results identified in our analysis were in accordance with observation in a recent randomized trial presented at EuroPCR 2013.16 Pan et al randomized 372 patients with bifurcation lesions to provisional stenting with (n = 187) or without side branch predilatation (n = 185). The primary outcome was better in the predilatation group. That is, the prevalence of Thrombolysis In Myocardial Infarction flow 0-1 was lower with predilatation than without (1% vs 10%; P < .001) after main vessel stenting.
However, immediate postprocedural gains in the present study were not translated into favorable long-term results. These unexpected findings are somewhat surprising and the underlying reasons remain unclear. However, an explanation may exist for the relatively high incidence of adjusted TVF in patients treated with SB predilatation. First, final kissing-balloon inflation was performed more frequently in the predilatation group. Gwon et al11 reported that in patients treated with the 1-stent technique, final kissing-balloon inflation increased the long-term risk of major adverse cardiac events. Second, the cross-over rate to a 2-stent technique was higher in the predilatation group. Patient-level data from 2 current randomized trials showed that the provisional T-stent approach is superior to a complex technique.17 Consequently, the unfavorable effects of SB predilatation on clinical outcome may result from the increased likelihood of potentially unnecessary final kissing-balloon inflation or cross-over to SB stenting. In the present study, however, SB predilatation was an independent risk factor for adjusted TVF even on multivariate analyses, and the difference in outcomes according to SB predilatation did not depend on the various patient subgroups. In the predilatation group, a borderline significant trend toward a higher adjusted TVF rate was present in the nonfinal kissing-balloon inflation cohort, while SB predilatation was a significant risk factor for adjusted TVF in the 1-stent technique cohort. These findings suggest that SB predilatation itself may have adverse effects on clinical outcome.
Some experts have recommended that SB predilatation be used when SB access is difficult or if there is a severe and calcified SB lesion.18 In the present study, however, the prespecified subgroup (bifurcation angle, diameter of the stenosis in the SB ostium, and the degree of calcification in the SB) analyses revealed no significant interactions with predilatation. Instead, the TVF rate was much higher in the predilatation group among patients with moderate to severe calcification, as well as in those without moderate to severe calcification. Based on our results, routine predilatation of the SB before main vessel stenting may not be appropriate in the provisional approach for true nonleft main coronary bifurcation lesions.
Study LimitationsThe present study has several limitations. First, this study was not randomized and therefore potential confounding factors may have significantly affected the results. For example, predilatation of the SB was performed more frequently in patients with unfavorable lesion characteristics, according to the operators’ decision. Unavoidably, therefore, the groups were unequal. To address this limitation, multivariate analysis with the Cox proportional hazards model, propensity score-matched analysis, and various subgroup analyses were applied to adjust for differences in patient characteristics. However, a strong possibility remains that other unmeasured or undocumented factors may have confounded the relationship between treatment strategies and outcomes, despite extensive adjustment for baseline risk factors. Additionally, because this study was conducted retrospectively, some cases have been missed due to incomplete recording of the procedure or suboptimal images that were insufficient to evaluate SB predilatation. However, we investigated whether the operators tried to perform a provisional approach at the initial stage of data collection in the COBIS registry. Second, the power of our study in the propensity-matched sample was not sufficient to predict clinical events. This can be attributed to the relatively small number of patients in our study. Target lesion revascularization was increased by about 2-fold before adjustment and loss of significance after the adjustment, while TVR and TVF continued to be significant. Perhaps this finding was also due to the relatively small number of patients with target lesion revascularization. Therefore, our results should be considered as hypothesis-generating and require confirmation in large randomized trials. Third, it seems that the diameter of the stenosis in the SB ostium did not appear to be severe. For the present analysis, we selected patients with true nonleft main bifurcation based on the Medina classification. The Medina classification was obtained using visual estimation, which tends to overestimate the severity of coronary artery lesion stenosis more than quantitative coronary angiographic analysis. Thus, SB lesions with less severe stenosis, as assessed by the quantitative coronary angiographic analysis, would have been included in the present analysis. Therefore, it may be hard to draw the same conclusions about SB with tighter stenosis, which is the reason interventional cardiologists commonly predilate the SB before main vessel stenting. However, angiographic significance does not always equal functional significance. Koo et al19,20 found that angiographic evaluation overestimates the functional severity of jailed SB lesions in each step of the provisional strategy for bifurcation lesions. Finally, our quantitative coronary angiographic data were derived from conventional 2-dimensional quantitative coronary angiographic analysis. Two-dimensional quantitative coronary angiographic analysis in bifurcation lesions, however, is less accurate, less precise, and less reproducible than 3-dimensional quantitative coronary angiographic analysis. This is also a drawback of our study.
CONCLUSIONSWe investigated the effect of side branch predilatation before main vessel stenting on procedural and long-term clinical outcomes using a large, dedicated bifurcation registry. Side branch predilatation increased the long-term risk of TVF, mainly due to the increased risk of TVR. Based on our results, routine predilatation of the SB before main vessel stenting may not be appropriate for true nonleft main bifurcation lesions using a provisional approach in the current era of PCI. However, our study is only hypothesis-generating and needs to be confirmed by larger controlled randomized studies.
CONFLICTS OF INTERESTNone declared.
This registry was sponsored by the Korean Society of Interventional Cardiology.