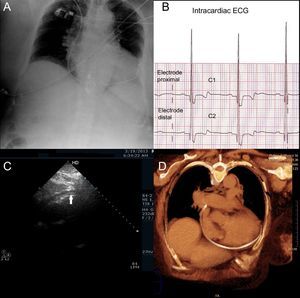
A 77-year-old woman, with an otherwise good clinical status, was admitted to the hospital for syncope. An electrocardiogram (ECG) revealed second-degree atrioventricular block with good ventricular response. Twelve hours later, she experienced a second episode of syncope and the ECG revealed atrioventricular block with pauses >3seconds; she underwent placement of a temporary pacemaker (TP) after cannulation of right subclavian vein and insertion of a lead that appeared to pace right ventricle. An X-ray showed the TP lead following the outer curvature of the heart to the apex (Figure A). An intracardiac ECG recorded complexes compatible with right ventricular epicardial pacing (Figure B). Intracardiac ECG is a recording of the patient's electrical activity that uses TP leads (proximal V1 and distal V2). Thus, the patient's own rhythm must be conserved and he or she must not be completely dependent on the pacemaker. Negative QRS deflection indicates an endocardial site; positive-negative deflection, an intramyocardial site; and positive deflection, epicardial pacing. In this case, the absence of current of injury indicated that the myocardium had not been perforated. Echocardiography revealed the presence of an electrode catheter inside the pericardial sac, with the distal end at the apex (Figure C). Computed tomography revealed catheter perforation behind the proximal segment of superior vena cava in the pretracheal retrocaval space. The catheter entered the pericardial sac, tracing a path from the inferior aspect to the apex, with discrete hemopericardium (Figure D). The TP maintained cardiac pacing, requiring an increase in the pacing threshold. During elective surgery to implant a permanent pacemaker, once the device had been placed and prior to withdrawal of the TP electrode, severe hypotension was detected; tamponade was suspected, but was ruled out after sternotomy. Once the TP electrode had been withdrawn, a stitch was placed in cava as prophylaxis. She was discharged from the hospital on the ninth day after the surgical intervention.
ISSN: 1885-5857
Impact factor 2023
7.2