To the Editor,
Isolated congenital absence of the pericardium (CAP) encompasses a range of congenital pericardial defects from a small foramen in the pericardium to a complete absence of the entire pericardium.1 Complete absence of the entire pericardium or absence of the whole left or right side usually has an excellent prognosis. On the other hand, partial absences are more dangerous because entrapment of parts of the heart through the defects may lead to fatal myocardial strangulation, myocardial ischemia and sudden death. Most patients are asymptomatic, but some may have non-specific chest pain.2 Complete absence of the left pericardium usually results in a characteristic chest radiograph, including a leftward shift of the cardiac silhouette. Electrocardiographic ST-T abnormalities are rarely described.1
A 28-years-old Caucasian man was found dead in his bed. He had reported vague, non-localized chest pain to his parents before going to sleep. An EKG performed two years before the sudden death showed normal SR, LV hypertrophy, negative T wave in leads V5 and V6, positive/negative T wave in lead V4, no lead I available, real QT of 0.40 and a correct QT 0.3. After 6 months an EKG showed: normal SR, artifact in lead V6, negative T wave in lead I, VL, V5, positive/negative T wave in lead V4, real QT 0.40 and corrected QT 0.37 (Figure 1). After another 6 months, an EKG showed normal SR, LV hypertrophy, flattening of T wave in leads I, V5 and V6, real QT 0.36 and correct QT 0.34. A 2-dimensional echocardiography was performed showing normal 4-chambers dimensions and septum. Six months before the sudden death, an EKG showed: normal SR, positive T waves in all the leads, high voltage of QRS in the precordial derivation, real QT 0.32, corrected QT 0.32.
Figure 1. EKG: normal SR, artifact in lead V6, negative T wave in lead I, VL, V5, positive/negative T wave in lead V4, real QT 0.40 and corrected QT 0.37.
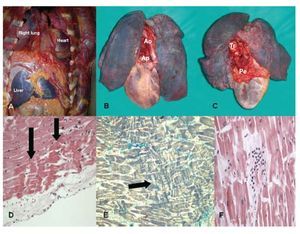
Autopsy showed a CAP with a "tongue" of pericardium on great vessels. The heart was completely caved into the left hemi-thorax and interposition of lung between the left hemi-diaphragm and inferior border of the heart was observed (Figure 2 A-C). The heart was slightly dilated, 460 gr in weight; the LV wall thickness was normal without septal asymmetry. Coronary arteries showed no stenosis or thrombotic occlusion. The valvular apparatus was normal. Patchy fibrosis and foci of contraction band necrosis in sub-endocardial layers (Figure 2 D-E) were microscopically detected. In some fields, the myofibers were stretched and an interstitial margination of polymorphonuclear leukocytes was observed (Figure 2 F). The parietal pericardial appendage showed an increased thickness and neovascularisation. The toxicological analyses were negative.
Figure 2.A: the heart was completely collapsed into the left hemi-thorax. B: anterior view. C: posterior view: a "tongue" of pericardium is visible. D-E: contraction band necrosis. F: margination of polymorphonuclear leukocytes was observed. Ao indicates aorta; Pr, pericardial ring; Pe, pericardium; Tr, trachea.
In patients with absence of the pericardium, EKG often shows incomplete right bundle-branch block with poor R-wave progression as a result of the leftward displacement of the heart. In this case the patient was in sinus rhythm; presence of right axis deviation, right bundle-branch block pattern, and leftward displacement of the transition zone in the precordial leads were not recorded.2 T-wave abnormalities at standard EKGs were considered aspecific and not worthy of further diagnostic tests. Pericardial defects are associated with other congenital abnormalities in up to 50% of patients, mostly cardiac and pulmonary in nature. Chest wall abnormalities have also been described.3 Genetic factors may play a greater, as yet undiscovered, aetiological role in CAP. CAP usually has an excellent prognosis, but sometimes the edge of the defect may compress the great vessels, which may affect filling and systolic function. Involvement of coronary arteries may lead to myocardial ischemia and sudden death, while involvement of the phrenic nerve may contribute to the symptoms.
We decided upon for an acute myocardial necrosis, in a patient with a CAP who presented atypical chest pain and T-wave abnormalities at standard ECG. We considered several hypotheses to establish the relationship between the CAP and myocardial necrosis, with torsion of the great vessels due to cardiac hyper mobility or impingement of a coronary artery by the edge of the pericardial defect being the most probable.3