To the Editor,
Unlike what was observed with brachytherapy,1 the use of drug-eluting stents (DES) has not been associated with the delayed intimal proliferation that characterises restenosis. A 12-month follow-up is recommended to define the need for revascularisation in DES.2 Restenosis 1 year after the implant is considered unusual.
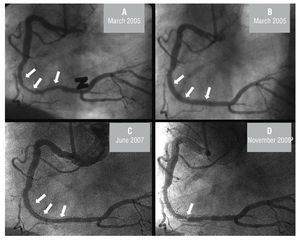
We present the case of a 77-year-old hypertensive male ex-smoker with diabetes and hypercholesterolemia who was admitted in April 2004 for an inferior infarction. He was treated with thrombolysis, showing signs of reperfusion. Twenty-four hours after being admitted, the patient presented post-infarction angina. A coronary angiography was performed, revealing single-vessel (distal right coronary artery) disease that was treated successfully with two conventional partially overlapping stents (Guidant MULTILINK ZETA 3.5´23 and 3.5´15, Abbott Laboratories). After 10 months without symptoms, he was readmitted on March 2005 for progressive unstable angina. Coronary angiography was repeated and in-stent restenosis was observed (Figure 1A), which was successfully treated with stent implantation of a paclitaxel-coated DES (TAXUS 3.5´32; Boston Scientific, Natick, Massachusetts) (Figure 1B). Two years later (June 2007), he was readmitted for recurring atypical pain and another coronary angiography was performed that showed neither restenosis in the previously implanted DES or other significant coronary lesions (Figure 1C). The patient was discharged on treatment with aspirin, atorvastatin, beta-blockers, and angiotensin-converting enzyme inhibitors.
Figure 1. Series of Angiograms. A: 2005, Conventional Stent Restenosis B: 2005, result after implanting a TAXUS 3.5×32 stent in the stent. C: 2007, no restenosis in the stent. D: 2009, subtotal stent restenosis.
There were no new events until November 2009 (more than 4 years after the DES implant) when the patient was readmitted for progressive unstable angina with a one-month evolution. Coronary angiography was repeated showing severe in-stent restenosis (Figure 1D), which was not present in the coronary angiography performed two years before. An intracoronary ultrasound study was performed (Figure 2) that showed proper stent expansion and apposition, and diffuse intimal hyperplasia and a minimal luminal area of 2.34 mm2, which confirmed the severity of the restenosis.
Figure 2.Intracoronary ultrasound study. A: longitudinal image with minimal luminal area (inset). B: minimal luminal area (MLA).
This case is the latest DES restenosis reported in the literature. Restenosis appeared clinically four years after the implantation and angiographies showed that it had developed at least two years after the implant. Although IVUS has limitations in differentiating intimal hyperplasia from in-stent thrombosis (the best technique would have been optical coherence tomography [OCT]), the ultrasound characteristics of our case (concentric, homogeneous echogenic, diffuse restenosis, which was more marked at one point) strongly indicated new intimal growth.
Late restenosis of DES is unusual to find in the literature.3 The largest published series showed a 2.6% rate of restenosis after one year. In another study with a paclitaxel-coated DES that is currently not available for sale,4 binary restenosis at 2 years was similar to conventional stent. In both studies, the diagnosis of late restenosis was achieved using coronary angiography, without restenosis six months after the implant and without knowing whether restenosis occurred about one year after intervention.
It is currently assumed that stent restenosis is due mainly to the proliferation of smooth cells. DES prevents this proliferation by various mechanisms. As with brachytherapy,1 it has been suggested that DES may inhibit most smooth muscle cells but leave a small portion able to multiply, leading to delayed neointimal growth. Other proposed mechanisms include inflammatory phenomenona or progression of the disease in the interior of the stent.5
Although there are no doubts about the effectiveness of DES in preventing restenosis, such cases indicate that in some patients, DES may delay but not prevent the intimal proliferation that causes restenosis. It is important that the follow-up period for studies on the safety and effectiveness of DES be extended beyond one year.