Keywords
INTRODUCTION AND BACKGROUND
A sustained decline in the death rate for cardiovascular diseases (CVD), predominately related to coronary heart disease (CHD), has occurred since 1960 in European countries (with the exception of some Eastern European countries, and the Russian Federation), United States (US), Canada and also confirmed in many other regions of the world including some Latin American countries and others undergoing a similar process of socioeconomic transition.1-6 In Spain, the CHD mortality rate is among the lowest in Europe and in the world (<37/100,000 in the Northern regions, <60/100,000 in the Southern and South Western communities).7 However, recent evidence suggests that this decline may be leveling off and that an alarming increase in the prevalence of preventable CVD risk factors is occurring in some regions. A study done in Scotland showed a stagnant trend in the CHD mortality decline in men and women age 35-44 from 1994 onward, and similar flattening of this trend in men ages 45-54 since 2003, which now seems to be occurring also in women ages 55-64. A six-fold socioeconomic position (SEP) differential between CHD mortality in the most deprived and most affluent fifths was noted, and attributed to a larger prevalence of risk factors in the most deprived group.5 A similar trend has been observed in men and women ages 35-54, from 1989 through 2002 in US.8 Furthermore, in a recent global trends analysis based on World Health Organization (WHO) data, CHD mortality rates from 1970 to 2000 were declining to a smaller degree (-30%) in some Latin American countries (Argentina, Chile, Brazil, Puerto Rico) as compared to US and Canada (-69%), whereas these trends are flat or increasing in Mexico, Ecuador and Costa Rica. These findings were interpreted as mostly related to more recent unfavorable changes in nutrition (obesity), hypertension, physical activity and smoking in Latin American countries.9
Several studies have reported an increasing prevalence of CVD risk factors. A recently published study using data collected by the National Population Health Survey and the Canadian Community Health Survey from 1994 (n=17,626) to 2005 (n= 132,947) reported an increase in Canadians of a physician-diagnosed prevalence of hypertension, obesity, and diabetes.10 In the US, an analysis of data derived from the National Health and Nutrition Examination Survey showed that 29% of the adult US population (an estimated 58.4 million individuals) had hypertension in 1999-2000. In contrast to previous reports, this data demonstrated a reversal of a declining trend in the hypertension prevalence reported between 1960 and 1991.11 In Spain, a prevalence study conducted between 2004 and 2005 of 216,914 workers (affiliated to a national health plan) of both sex with a mean age of 36.4 years, showed that 22% were hypertensive, 38.5% overweight (Body Mass Index [BMI] 25 to <30) and 15.5% obese (BMI 30 or >). These figures are similar to data obtained in US from a slightly older general adult population cohort (mean age of 43 years) with the exception of a much higher prevalence of obesity in the US population (27%).12,13 In Brazil, adult obesity has tripled since 1977 to 1997, and in Chile prevalence of obesity in first grade children has increased from 5.5% to 18% since 1987 until 2000.14 In the US, adult prevalence of diabetes has doubled between 1980 and 2006, which may be related to the increase in obesity prevalence in the previous decades.15 Recently WHO has reported that obesity is reaching world wide epidemic dimensions.16
These data suggests that the decline in CVD mortality over the last 50 years in most of Europe, US, Canada, some Latin American countries and others in the process of socioeconomic transition may soon end.
In the meantime, CHD has become progressively more predictable over time with the identification of blood cholesterol, blood pressure, smoking and diabetes mellitus as major modifiable risk factors.1-4 These contributions have clearly influenced the decline in CVD mortality observed since 1960, through lifestyle changes and specific therapies. More recently, the predictability of coronary events, including mortality, has improved even further with the additional contributions of inflammatory markers such as the C-reactive protein (CRP), deposits of calcium in the coronary arteries and the genetic characteristics, that likely will evolve in the future into some form of individual genetic predictive score.14-18 However, it is unclear to what extent greater predictability of risk will influence the prevention of CVD morbidity and mortality in the population at risk.
PREDICTABLE AND MODIFIABLE CARDIOVASCULAR DISEASE RISK FACTORS
The expression of modifiable risk factors seemingly depends on multiple mechanisms ranging from genetic to SEP and environmental components. Nowadays it is generally accepted that the endothelial oxidative stress caused by abnormalities such as high LDL cholesterol, hypertension, smoking, high blood sugar may be the common pathway that determines a cascade of abnormal vasoactive (reduction in the release of nitric oxide [NO]) and inflammatory responses such as increase of CRP, interleukin-6 (Il-6), monocyte chemoattractant protein-1, intercellular adhesion molecule-1, that along with endovascular remodeling leads to the formation of atheroma in the arterial wall and eventual ischaemic accidents.19
This plausibly synergistic effect of the most recognizable risk factors acting through a common pathological process emphasizes the need for a comprehensive strategy of risk management both in individuals and populations. However, as Geoffrey Rose has pointed out in his seminal paper Sick individuals and sick populations: "the individual and the population-based have their counterparts in prevention. In the first, preventive strategy seeks to identify high-risk susceptible individuals and to offer them some individual protection. In contrast, the population strategy seeks to control the determinants of incidence in the population as a whole".20-23
What determines the presence of hypertension, type-2 diabetes, cholesterol abnormalities, obesity and even inflammatory markers in individuals and their incidence in populations is still largely unknown. In addition, these so called "independent risk factors", or CVD risk factors may have also multiple, and not well-defined mediators. Despite their limitations, they are instrumental today in the prediction of risk in individuals and in the decision-making process for specific therapies.
In reference to the CVD risk factors, some monogenic induced anomalies causing cholesterol abnormalities such as familial hypercholesterolemia have been identified.19 In addition, even more uncommon monogenic disorders as the one related to a genetic mutation responsible for the absence of high-density lipoprotein cholesterol in the plasma (Tangier's disease) and rare forms of secondary hypertension have been discovered.21 Moreover, multiple polygenic associations to some of the traditional risk factors have been described in the last few years yet with limited direct effect in the expression of disease, in contrast to the monogenic ones, of greater penetration but of uncommon prevalence.20,21 The list of these polygenetic associations or "predisposition genes" keeps growing rapidly for many of the known modifiable risk factors and a genetic risk score is currently in the making as an additional tool to predict CVD risk.20,21 However, it is unclear at this time what its contribution will be in the prevention of CVD risk in the future. In the last 10 years a "coronary artery calcium score" determined by computed tomography has contributed to the predictability of risk yet its additional advantage and cost-effectiveness in relation to other screening methods such as the Framingham score has been disputed and remains to be established.18
IMPACT OF THERAPIES IN THE DECLINE OF CARDIOVASCULAR DISEASE RISK AND MORTALITY
There is no consensus about the quantitative contribution of the specific therapies targeting individuals with traditional risk factors in the decline of CVD mortality observed since the 1960's. This decline began before most of the current antihypertensive and lipid disorder therapies and coronary revascularization procedures were available and was driven mostly by a decline in CHD mortality. A study of data collected in the US from 1968 to 1976 attributed 56% of the CHD mortality decline to changes in lifestyle (less smoking and dietary changes leading to a reduction in blood cholesterol levels) and only 39.5% to specific therapies (antihypertensive therapy, beta blockers, coronary care units, coronary bypass surgery).24 A more recent study analyzing data from the US since 1980 to 2000, attributes 47% of this decline to the currently available specific therapies; a comparison made by the same authors with data collected in The Netherlands, Scotland, England, Wales and New Zealand using the same methods and analysis showed similar results.25 Moreover, the cost effectiveness per year of life saved by specific therapies for CHD has been noted to be inferior to the cost-effectiveness of changes in the lifestyle (i.e., coronary bypass surgery for three-vessel disease versus smoking cessation).26 Furthermore, SEP factors and the built environment may influence lifestyle choices and therefore indirectly determine antecedent factors in the pathway leading to the CVD risk.27-33
Nevertheless, multiple previous studies in different regions of the world have shown a reduction of cardiovascular events and mortality with the isolated use of statins, antihypertensive measures (particularly beta-blockers and angiotensin converting enzyme inhibitors), and smoking cessation, both in individuals free of the clinical expression of coronary heart disease as well as in those after an acute coronary event, therapies that will impact favorably many of the modifiable CVD risk factors.34-37 Cardiac rehabilitation programs have proven to be particularly cost-effective in the management of patients following a coronary event, likely due to its emphasis on patient education.36,37 However, the primary and secondary reduction of risk achieved by treating isolated CVD risk factors has been rather modest (ranging between 15 to 30%) when compared to strategies addressing the risk more comprehensibly, especially in the setting of secondary prevention. Examples are the CHAMP study (inpatient intensive educational program after a coronary event resulting in a significant adherence to the use of aspirin, statins, beta-blockers and angiotensin converting enzime inhibitors), which had a dramatic reduction of recurrent myocardial infarction (from 7.8% to 3.1%) and cardiac mortality (from 5.1% to 2.0%) after 1 year (p<0.05).38 The STENO-2 Study conducted in type-2 diabetics followed for 7.8 years showed a 53% reduction of ischemic events and mortality after achieving pre-established goals in hypertension, blood glucose and lipid abnormalities control.39
Using a conventional risk assessment chart, a 55 year-old man that presents with multiple risk factors, including high LDL cholesterol, hypertension, type-2 diabetes and is a smoker, has a 400-600% higher chance of a coronary event in 10 years than his counterpart. On the other hand, the reduction of an ischaemic event risk is not greater than 20-30% by treating his risk factors as isolated entities.34-37,39 These data suggests that there are unmeasured factors contributing to the synergistic effect on traditional cardiovascular risk factors on mortality risk.39
Furthermore, aggressive attempts to treat single risk factors has led on occasions to deleterious results despite their theoretical plausibility. A case in point is the ILLUMINATE trial for torcetrapib and atorvastatin, which was stopped prematurely after documenting a significant increase in mortality in comparison with the control group receiving atorvastatin alone, despite the former combination achieving a 75% increase in the HDL level and a 25% reduction in the LDL cholesterol.40 The ACCORD trial, which aimed to aggressively reduce the glycosylated Hbg to <6% in diabetics with CVD, was also stopped prematurely when a higher mortality was noticed in the treatment group.41 The interpretation of these negative results is still the object of some controversy since poorly understood effects of these therapies may have had the ultimate responsibility in the higher number of deaths. Nevertheless, the importance of a comprehensive, cost-effective approach to the management of CVD risk is indirectly supported by these unfortunate results.
IMPACT OF SOCIOECONOMIC POSITION FACTORS AND THE BUILT ENVIRONMENT IN CARDIOVASCULAR DISEASE RISK AND MORTALITY
Thomas McKweon, a British physician and demographic historian, in a series of publications since the 1950's, proclaimed that socioeconomic changes were more responsible than specific contributions of medical therapies or public health policies for the population growth and improvement in health outcomes in the last 200 years. Mckweon was one of the first investigators in placing SEP at the center stage of disease prevention.27,29 Today, it is general knowledge that the prevalence and possibly the expression of some of the key CVD risk factors such as obesity, smoking and sedentary lifestyle, are influenced by SEP. Some have called this influence the "fundamental causes of disease", and others "the cause of the causes".27,28 Sir Michael Marmot, who credits Geoffrey Rose for this term, places the "social gradients of inequality" at the focus of this issue: "Describing the social gradient in morbidity and mortality in terms of 'inequality' draws attention to the fact that death and illness are related to social inequalities". He also states that for this reason the term "health inequalities" has been avoided by some and transformed into " health variations" in Great Britain and in the US substituted by the term "health disparities".28 According to the proponents of "the fundamental causes of disease", when society develops methods to prevent disease and improve survival, individuals with greater resources (money, education, social status) will receive more benefits of those advancements than individuals in a more disadvantageous SEP.27
Studies conducted in countries as disparate in terms of the degree of SEP development and ethnic composition as Norway and Chile, have shown that the lower the educational and income levels, the greater the prevalence of obesity, smoking and other harmful behavioral features such as alcoholism and sedentary lifestyle.42,43
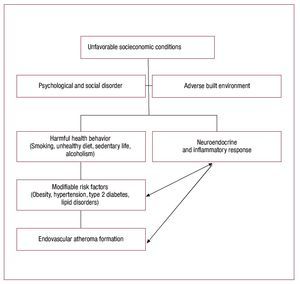
As discussed by Diez- Roux, "the growth of interest in this area has revitalized the notion that cardiovascular disease results from the complex interaction between the characteristics of individuals (their genes, their behaviors, and their biological attributes) and the physical and social environments in which they live".30 It is unclear, however, the mechanisms by which SEP operates in the process that leads to the endovascular atheroma formation. An hypothesis to consider is that an unfavorable SEP lays the ground for psychological disorders (depression, anxiety, low self- esteem, hostility), social disruption (family and group) and significant stress, triggering a causal pathway that may include neuro-endocrine and inflammatory responses (i.e., Il-6, CRP ),44-48 which leads to the adoption of harmful health behaviors (unhealthy dietary habits—obesity, smoking, sedentary lifestyle) that will favor the expression and prevalence of hypertension, lipid disorders, type-2 diabetes. As suggested by Ranjit et al "persons of lower SEP have greater inflammatory burden than those of high SEP as a result of the cumulative effects of multiple behavioral psychosocial and metabolic characteristics. If the role of inflammation in the origin of multiple chronic diseases is confirmed, inflammation may represent a common element through which SEP is related to cardiovascular disease and other chronic disease".47 Similar findings were reported in a study done in British civil servants (the Whitehall II study) that described an inverse relation between social position and levels of Il-6 and CRP.48
Figure 1 depicts these hypothetical pathways. Some of the concepts and information discussed above, and a portion of the hypothetical pathway proposed in figure 1 has been included in a previous publication by one of the authors.49
Figure 1. Hypothetical pathways for unfavorable socioeconomic position factors leading to endovascular atheroma formation.
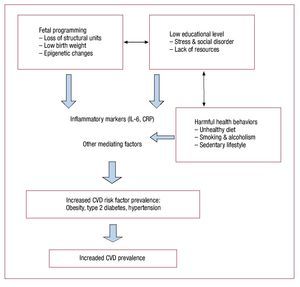
The role of early life influences on individuals and future generations' risk of CVD, is a field that has been growing in the last two decades and is worthy of more consideration and research, especially since the 9-month time period of pregnancy is often in a controlled setting and could be a potential area for simple but potent interventions. A "thrifty phenotype" hypothesis that links the maternal undernourished environment with fetal programming conducive to loss of fetal structural units such as nephrons, myocardial cells, pancreatic ß cells, and low weight at birth, have been suggested as possible biological pathways from low SEP to early and adult life morbidity and mortality, as discussed recently by Lopez-Jaramillo in Revista española de CaRdiología.50 This author also quotes numerous studies reporting the increased prevalence of CVD risk factors such as obesity, diabetes mellitus and hypertension, found later in life in offspring with a low birth weight, suggestive of possible epigenetic mechanisms, or alterations in the expression of genes that could result in changes in the synthesis of certain proteins such as angiotensin II, leptin and adiponectin. Another early life influence, low education level, has been shown to be a stronger predictor of all-cause mortality than income level, which generally reflects an adult life influence, in recently published studies from a Chilean adult cohort followed for 8 years.51,52 In a study published in 2002, 25% of Chilean women were obese (BMI>30 kg/m2), most of them in the lower education level.53 Figure 2 graphically shows the hypothetical links between early life influences and CVD risk factors. Furthermore, a disadvantageous SEP more likely does not support healthy choices or environments in adult life. Recently, several studies have reported the association of the built environment -human modified places such homes, schools, workplaces, neighborhoods, parks- to cardiovascular risk factors, especially obesity.30-33 Much of the discussion of the built environment has focused on 'walkable' neighborhoods, access to healthy food and public transportation. Often, low-income neighborhoods are less 'walkable' and have unsafe parks discouraging physical activity, compared to high-income neighborhoods. Furthermore, fast food and convenience stores are more abundant than grocery stores in low-income neighborhoods, which contribute to unequal access to healthful food choices in poorer areas. Accordingly, favorable conditions in the socioeconomic environment may lead to a reduction of harmful health behaviors and therefore to a disruption of the pathway conducting to the expression of hypertension, type 2 diabetes, smoking and eventually to cardiovascular atherosclerosis. Data from a Latin American cohort study already cited,51,52 reflective of a developing society in a stage of socioeconomic transition, suggests that SEP may act differently than in developed societies, with education having a stronger influence than income in a social environment where the higher income quartiles are nearly at the poverty level of more advanced societies. More studies are needed to further define these characteristics that may assist in formulating better preventive strategies at the population level in low- and middle-income countries.
Figure 2. Hypothetical pathways for adverse early life influences leading to an increased prevalence of cardiovascular disease (CVD) risk factors and eventual increased prevalence of cardiovascular disease. CRP: C-reactive protein.
Private and public programs to support access to health and educational resources, and promote improvements in the built environment are critical components in this process. Recently Seligman and Schillinger54 have described a response to "food insecurity" from low income households that is associated to preferences for energy dense foods (carbohydrates and foods with added fat, salt and sugar), leading to increased body fat, decreased lean muscle mass and favoring the risk of obesity and diabetes. This situation has a simple economical motivation, as it has been pointed out by these authors: "a $1 US dollar can purchase either 1200 kcal of cookies or potato chips or 250 kcal of carrots"; in the US "between 1985 and 2000 the retail price of carbonated soft drinks rose by 20%, the prices of fats and oils by 35%, and those of sugars and sweets by 46% as compared with a 118% increase in the retail price of fresh fruits and vegetables". The globalization of the food industry in developing and recently industrialized societies in Latin America and Asian countries and the promotion of these products in lower income populations, especially those living in large urban centers, will make them more vulnerable to obesity, diabetes and hypertension to chronically disabling diseases as a consequence of the consumption of energy dense, low-cost nutritionally poor foods. Data reported by the WHO in 2004 in several Western European countries, including Spain and England, showed that the consumption of fruits and vegetables was higher in groups with a higher income, education and occupational level.55 Until improvements in societal inequalities occur, efforts must be made towards restructuring public food policies to promote whole foods, such as limiting agriculture subsidies to soy bean and corn producers which fuel the global market of high fructose corn syrup additives to food products and considering a higher taxation of sugar-containing carbonated beverages. Furthermore, worksite and school wellness programs to quit smoking, lose weight and engage in leisure physical activities along with community initiatives to promote 'walkable' neighborhoods with better access to healthier food, may be initial steps in the right direction.
LIMITATIONS
This review has several limitations. It includes only a summary discussion of a very vast field that includes current CVD risk trends and preventive measures, at the individual and population levels, and a comparison of their relative contributions in reducing CVD risk. The role of socioeconomic influences constitutes the central aspect of our review because it is an important yet still largely unresolved determinant of risk in many regions of the world. We are aware that the society at large, of which the health professionals and scientists are only a part, is the one that should address and implement most of the needed changes.
We contrast the rapid progress in CVD risk prediction with the stagnation of preventive measures particularly at the population level in order to emphasize the need for redirecting existing preventive strategies. Our discussion of the CVD risk prediction tools available today is necessarily limited and the reader should look for other sources to obtain detailed information on this subject.
Finally, the mechanisms discussed to link socioeconomic factors to biological causal pathways in determining CVD risk are highly hypothetical and need verification through additional investigation.
CONCLUSIONS
The persistently high CVD mortality rate in some regions, the attenuation of CVD mortality decline observed in others, and the increased prevalence of CVD risk factors in most of developed and developing countries are indicators of globally stagnant CVD prevention. The fact that these alarming trends predominantly affect those in the lower socioeconomic strata underscores the importance of determining the role of SEP in the causal pathways of CVD. The interaction of traditional risk factors, genetics, education and income levels, psychosocial and the built environment characteristics needs further investigation. An important large-scale epidemiological prospective research started in 2002, the Prospective Urban Rural Epidemiological (PURE) study, that will include 140,000 individuals from 600 communities around the world with a follow-up of 10 years, may provide a better understanding of the interrelationship of all those factors when completed.56
The recently reported global epidemic increases in obesity prevalence both in adults and children by the WHO is of particular concern in view of the impact that it may have in the future prevalence of chronic and CVD diseases. According to this report, programs oriented to promote healthy dietary habits and regular physical activity in childhood may be key components in controlling the global obesity threat.12
However, all these efforts may not have a significant impact in controlling the risk at the population level if improvements in the socioeconomic conditions and the built environment, especially in low- and middle-income countries, do not occur. The present global obesity epidemic stresses the need for these changes; otherwise, the burden of increasing chronic disabling diseases will overwhelm the next generations.
ABBREVIATIONS
CHD: coronary heart disease
CVD: cardiovascular disease
SEP: socioeconomic position
Disclaimer: The views expressed in this article are those of the authors and are not necessarily those of the University of California, Sharp Health Care and the University of Colorado.
Funding: This work has been sponsored by Fundación Araucaria (Araucaria Foundation) a non-profit medical foundation established in San Diego, California and an Associate International Member of the World Heart Federation.
Correspondence: Tomas E. Romero, MD.
831 Adella Ave, Coronado (San Diego), CA 92118, USA
E-mails: tromero560@aol.com; tomas.romero@sharp.com