Keywords
INTRODUCTION
The Spanish Pacemaker Registry (SPR) contains data going back to the 1990.1 This information has been published or made available in other formats since 19942-5: the complete set of data is available on the Web at www.marcapasossec.org in the heart stimulation section. The present work reports the data for the year 2005 and discusses a number of developments that have taken place in recent years.
METHODS
The information presented is the result of computer processing of different information fields on the European Pacemaker Patient Identification Card.2 This card is filled out and sent to the Registry when medical personnel implant a pacemaker. This can be done in paper or magnetic format; the provision of these details to the Registry is meant to be obligatory (Spanish Royal Decrees 634/1993 and 414/1996). Eighty-two hospitals turned in their data in 2005 (see Table, in which these hospitals are grouped by Autonomous Region).
The total number of pacemakers purchased in 2005 was obtained from the different businesses operating in this sector in Spain. The data sent by these businesses to Eucomed was also taken into account. A small error might be expected due to the sale of pacemakers that are not actually implanted. The SPR database is based on the Access computer program. A specific routine was developed to gather the information required for the present study.
The data sent to the Registry have also been sent to the European Pacemaker Registry since 1994, the website of which allows comparisons to be made between pacemaker use in Spain and other European countries (www.heart.org.uk/ewgcp).
In the present work, data referring to the structure of the Spanish population were obtained from the latest report for 2005 published by the Instituto Nacional de Estadística (INE: The National Institute of Statistics) (www.ine.es).
RESULTS
Number of Pacemakers Implanted and Structure of the Spanish Population
In the 2005, 9165 pacemaker implant or replacement cards were received by the Registry, a figure corresponding to only 31.9% of all pacemakers implanted in Spain according to the sales data provided by the different businesses operating in the sector. These industry figures report the sale of 28724 pacemakers 653.1 per million inhabitants. Eucomed reports a corresponding figure of 28 168; if this is value is used instead, 32.5% of cards were sent to the SPR and the number of inhabitants per million with a pacemaker implantation was 638.7. In addition, nine units per million inhabitants were implanted for the purpose of cardiac resynchronization therapy (interval=8.89-9.23 depending on which of the information sources is used).
In 2005 the population of Spain was 44 108,530, with 21.7 million males and 22.3 million females (INE figures for the January 1, 2005; no later figures are available).
First and Replacement Pacemakers
A total of 74.9% of those who received a pacemaker in 2005 were implanted for the first time. Those receiving a replacement made up accounted for 25.1% of registrations. The replacement of electrode cables on their own accounted for 0.4%; in 2% of procedures these were changed at the same time as the generator itself (due to its wearing out, a need to change the pacing mode, or because of a defect).
Age
The mean age of the patients who received a pacemaker in 2005 was 75.67 years; the mean age of those receiving their first pacemaker was 75.69 years, while that of patients receiving a replacement was 75.64 years. The mean age of the male patients involved in these procedures was lower than that of the female patients (74.91 years compared to 76.63 years). These data were prepared from the record cards on which patient age had been included (92%).
The largest number of implantations involved patients in their 70s (39.7% of the total), followed by those in their 80s (34.4%). This shows that, in the majority of cases, the need for an implant is usually associated with a degenerative problem (Figure 1).
Figure 1. Distribution (in percentages) of implants by patient age and decade of life.
Sex
Men made up 56.6% and women 43.4% of the implanted population. Some 56.9% of those receiving their first implant were men, and 43.1% were women. The sex ratio with respect to those receiving a replacement implant was only very slightly different: men 55.8%, women 44.2%.
For the first time, and covering the period of the last two years, the numerical relationship between men and women was studied with respect to electrocardiographic findings. The incidence of sick sinus syndrome (SSS) was virtually the same in both sexes (men/women 1.06 in 2004 and 1.09 in 2005). However, the incidence of disturbances in conduction was clearly greater among men in both years. For example, for intraventricular conduction disturbances (ICD), the men/women ratio was 2.27 in 2004 and 2.35 in 2005, for atrioventricular block (AVB) this ratio was 1.25 in 2004 and 1.3 in 2005, and for atrial flutter or fibrillation it was 1.27 in 2004 and 1.22 in 2005.
Symptoms
Figure 2 shows the distribution of the signs or symptoms associated with the rhythm alterations deemed to indicate the need of a pacemaker. As in previous years, syncope and dizziness were the most often cited problems, followed by dyspnea and bradycardia. Only 2.1% of all implantations involved asymptomatic patients or were performed for preventive reasons.
Figure 2. Distribution (in percentages) of the clinical manifestations of patients receiving their first implant.
Etiology
The causes giving rise to the need for a pacemaker were, on most occasions, either unknown, or fibrosis of the conduction system, followed by ischemia, and cardiomyopathy. Hypertrophic cardiomyopathy was the cause of 0.98% of the total number of implantations, post-ablation was the cause of 0.95%, and neuromediated syndromes were behind 1.04% (among which malignant vasovagal syndromes made up 0.1%) (Figure 3).
Figure 3. Reason for implantation.
Electrocardiographic Abnormalities
Figure 4 shows the preimplant electrocardiographic anomalies recorded and their distribution. Unlike in northern European countries, in which SSS is the most common electrocardiographic abnormality associated with pacemaker implantation, in Spain, AVB was the most common (39.8% of cases; 52.4% if the AVB in atrial fibrillation is taken into account). This was followed by SSS and the group composed of atrial fibrillation or flutter with AVB, or bradycardia. ICD was responsible for 5.9% of cases.
Figure 4. Distribution of electrocardiographic abnormalities before implantation. AF/FL + BRAD: atrial fibrillation/flutter with bradycardia; SSS: sick sinus syndrome; ICD: intraventricular conduction disturbance; AF + BLOCK: atrial fibrillation plus atrioventricular block; AVB: atrioventricular block.
Cables/Electrodes Implanted
Polarity
In 2005, the cables/electrodes implanted were nearly all bipolar (99.3%); these have become established as the most used stimulation system in Spain in recent years (Figure 5). Of the monopolar cables implanted, a significant percentage (15%) were epicardial cables implanted during scheduled heart surgery or during surgery performed specifically for this purpose. Another important percentage was made up of implants put in place via the coronary sinus; the smaller diameter of uniploar electrodes led to their being chosen in such procedures. These were used in 31% of cases (employed in resynchronization therapy or when anatomic difficulties, or impossibilities presented themselves due to the presence of a tricuspid prosthesis etc).
Figure 5. Polarity of electrodes implanted in recent years.
In the atrial position, bipolarity was even more popular; 99.8% of all cables used in this cavity were bipolar.
Fixation Mechanism
Active fixation was used for an overall 30.9% of cables/electrodes: in the atrium 48.0% were secured in this way, and in the ventricle 23.9%.
Pacing Mode
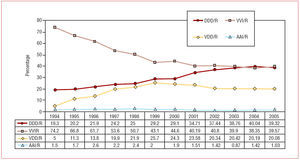
1.a) Overall, 40.6% of all pacemakers implanted were for single chamber pacing, although only 1% were for atrial pacing. Pacing for maintaining atrioventricular (AV) synchrony (including two chamber DDD and VDD pacing) was used in 60.4% of cases (Figure 6). However, if it is taken into account that pacing for permanent atrial fibrillation or flutter with AVB or bradycardia (card codes C8 and E6) made up 21.1% of cases, the number of patients requiring sequential pacing must be much higher. In fact nearly 18.5% of cases, pacing was performed without maintaining the atrioventricular synchrony that could have -- or indeed should have -- been maintained according to the cardiac pacing guides of Spanish, American, or European cardiology societies.6,7 Age was probably the factor that most influenced the decision to proceed in this non-optimum way (although other reasons, such as technical problems, cannot be ruled out). Until the year 2000, the increased use of pacing modes that maintain AV synchrony was owed to the growing popularity of both DDD and VDD modes. However, after 2000, only the use of DDD has increased; the use of VDD has remained stable or has slightly dropped away (Figure7).
Figure 6. Distribution of stimulation modes in 2005.
Figure 7. Change in stimulation mode between 1994 and 2005.
b) Rate responsive pacing (using some form of sensor) made up 79.8% of all the pacemakers used.
c) Stimulation for cardiac resynchronization therapy, in the case of heart failure with ICD, accounted for 1.35% of all pacemaker implants according to SPR data (1.37% according to industry data: 396 units communicated to the Registry; 407 according to Eucomed data). The Registry data reflect no increase with respect to 2004 (1.37%). A movement towards the use of units that provide defibrillation therapy was noted: in 2004 these made up some 473 units according to data obtained from industry and communicated to Eucomed, and 703 in 2005.
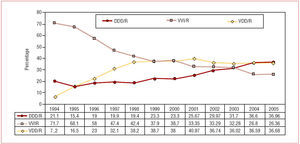
2. Pacing in AVB. When the patients with ABV and sinus rhythm were analyzed, similar percentages were seen in terms of the use of VDD and DDD modes (36% each). The increase in the percentage use of pacing modes that maintain the atrioventricular synchrony in this group of patients has been due to the progressive increase in the use of DDD pacing in recent years, and the non-significant change in the use of VDD (Figure 8). Some 26.4% of these AVB patients received VVI/R pacing in 2005, although this percentage has fallen year after year and is clearly used more among older patients. This can easily be seen from the analysis of patients below and above 80 years of age; this type of pacing was used in 45.1% and 12.71% of cases respectively. A significant difference was recorded for the last two years of analysis (Figure 9).
Figure 8. Change in stimulation mode in atrioventricular block (from first to third degree cases [card codes C1-C7], excluding patients with permanent atrial fibrillation [code C8]) between 1994 and 2005.
Figure 9. Change in use of VVI/R stimulation in atrioventricular block in patients grouped by age between 2001 and 2005 (excluding patients with permanent atrial fibrillation)
Figure 10 shows the modes used in the first/second and third degree AVB subgroups of patients.
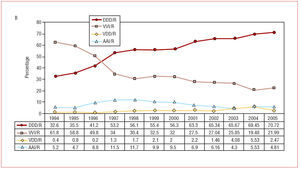
Figure 10. A and B: stimulation modes used in 2005 in first and second (card codes C1-C4), and in third (card codes C5-C7) degree atrioventricular block.
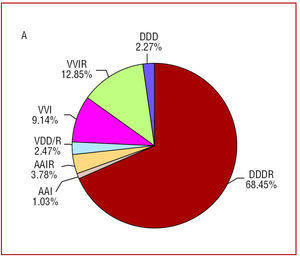
3. Pacing in SSS. The DDD/R mode is still the most used (employed in just over 70% of cases). The use of the AAI/R mode (4.8%) has not increased, nor has the use of the VDD/R mode (2.5%) (Figure 11). As Figure 11 shows, although there has been a notable improvement in pacing in SSS,6,7 the maintenance of the use of the VDD/R mode is noteworthy. In recent years its use has in fact matched or surpassed that of AAI, even though it is clearly not indicated for this type of electrocardiographic anomaly. Neither is the VVI/R mode very justifiable when sinus rhythm persists, although it was used on 22% of occasions. It has, however, shown a clear trend towards a reduction in usage over the years which the Registry has been in operation (with the exception of a small upturn in 2005). The use of the VDD mode has also decreased. The choice of the VVI/R mode seems to be importantly influence d by patient age (used in 38.7% of cases in patients over 80 years of age, but only in 14.9% in those younger; see Figure 12)
Figure 11. A and B: stimulation modes used in sick sinus syndrome in 2005, and the change seen between 1994 and 2005
Figure 12. A and B: Iinfluence of age on stimulation modes employed in sick sinus syndrome, and the change in the use of VVI/R stimulation between 2001 and 2005 (patients with permanent atrial fibrillation were excluded [card code E6]).
4. Pacing in intraventricular disturbances. In ICD, the most commonly used mode was DDD/R (45.7% of patients), followed by VVIR (28.8%). The remainder (25.6%) received VDD/R pacing. Among these patients, age was also the factor that most influenced the choice of pacing mode; 49.6% of those over 80 years of age received VVI/R pacing, while only 18.1% of younger patients were treated with this mode.
Pacemakers for cardiac resynchronization therapy made up 1.35% of all implants (19% of those <80 years of age in the ICD subgroup, and 0.8% of those >80).
Data Quality
Only the data supplied which corresponded to 31.9% of all the pacemakers implanted in Spain in 2005 (32.5% if industry or Eucomed data are taken into account) were analyzed.
Data were missing on some of the cards received:
- Age on 8.0%
- Sex on 11.1%
- The symptoms experienced on 22.4%
- Etiology on 37.3%
- ECG results on 22.2%
The sample was large enough for conclusions to be drawn on the quality of pacing provided in Spain, but not for this to be broken down by Autonomous Region (great disparities were seen because of the wide variation in the participation of the hospitals in these regions, which varies from 0%-100%).
SUMMARY AND COMMENTS
The greater frequency of pacemaker implantation in men compared to women was maintained in 2005, mainly because of the greater incidence of conduction abnormalities among men (both atrioventricular and intraventricular, although the incidence of SSS was the same for both sexes). In men, the mean age of implantation was somewhat older than in women. Most patients received pacemakers when in their 70s or, to a lesser extent, in their 80s.
The cable/electrode selected was nearly always bipolar in both chambers; only a few monopolar cables/electrodes were used in special circumstances (such as in epicardial emplacements). The number of cables that employ active fixation continued to increase notably, especially in atrial implants where they now account for almost 50%.
The pacing modes used to maintain AV synchrony has improved significantly in recent years, although this has tended to stabilize over the last two years. These improvements have largely due been to an increase in the use of DDD double chamber pacing, while the use of VDD and single chamber atrial pacing has remained stable.
Resynchronization therapy accounted for 1.35% of the pacemakers implanted. This figure is no different to that of previous years, owing to the notable use of units that afford the possibility of defibrillation.
Although more cards have been received, the overall percentage of implantations recorded has not improved. Neither has there been any improvement in the quality of the data the Registry receives.
ACKNOWLEDGEMENTS
The authors thank nurses Pilar González Pérez and Brígida Martínez Noriega, and IT specialist Gonzalo Justes Toha for their invaluable help in maintaining the Spanish Pacemaker Registry, the medical staff at the different participating centers who sent in pacemaker registration cards, and the different business that provided their information on the use of these devices.
Correspondence: Dr. R. Coma-Samartín.
Sección de Estimulación Cardiaca. Sociedad Española de Cardiología.
Arturo Soria, 184. 28043 Madrid. España.
E-mail: coma@vitanet.nu