The present report summarizes the analysis of pacemaker implantation and replacement data sent to the Spanish Pacemaker Registry in 2013, with specific discussion of pacing mode selection.
MethodsThis study was based on information obtained from the European Pacemaker Patient Identification Card.
ResultsInformation was received on 118 hospital centers, with a total of 12 831 cards, or 35% of the estimated activity. There were 755 and 58.1 conventional and resynchronization devices per million population, respectively. The mean age of patients receiving an implant was 77.4 years. Men received 59.5% of first implantations and 56.6% of replacements. Most implantations and generator replacements were performed in patients older than 80 years. Almost all endocardial leads used were bipolar, and 78.7% of leads had an active fixation mechanism. Despite being in sinus rhythm, 24% of patients with sick sinus syndrome and 25% of those with atrioventricular block were paced in VVIR mode.
ConclusionsThe use of pacemaker generators and resynchronization devices per million population continues to increase in Spain. Active fixation mechanisms predominate for leads but just 20% of leads are compatible with magnetic resonance imaging. The factors influencing the correct selection of pacing mode were age and, to a lesser extent, the type of atrioventricular block, and sex. Implementation of home monitoring of pacemakers remains low.
Keywords
The Spanish Pacemaker Registry (SPR, Registro Español de Marcapasos) published its first official report in 1997,1 although the first data were actually obtained via a survey in 1989.2 Since then, and as one of its objectives, the SPR has annually reported3–13 the most relevant characteristics of cardiac pacing in Spain. These reports indicate the degree of compliance with recommendations in current clinical practice guidelines,14–17 compare pacing in Spain with that reported in the registries of other countries18–20 or in other Spanish registries, and determine the quality or appropriateness of the pacing performed. The present report summarizes the most relevant data of the cardiac pacing performed with pacemakers in Spain during 2013 and any changes from the results of previous reports. Detailed information on cardiac pacing has been annually published on the website of the Working Group on Cardiac Pacing (Sección de Estimulación Cardiaca) since 1999.21 However, the information available is incomplete due to progressive database developments and software improvements.
METHODSEuropean Pacemaker Patient Identification CardThe information contained in the European Pacemaker Patient Identification Card (EPPIC) was processed, such as age, sex, and codes for symptoms, causes, electrocardiographic indications, pacing modes, and implantations and extractions of leads or generators. An automatically generated copy of the EPPIC is forwarded to the SPR, although this information can also be sent-and is sent-electronically, such as via the databases of each center, with the proper privacy guarantees and with all essential information of the EPPIC. The Working Group on Cardiac Pacing has its own freely accessible database10 to automate data collection and processing, but this resource has failed to improve the registry and a new website is under development. The data received are refined using specific software by 2 nurses trained in the monitoring of pacing devices.
Information Provided by the Various ManufacturersNot all EPPICs are relayed to the SPR (despite this practice being required by current Spanish legislation in order to monitor possible alerts, etc: Royal Decree 1616/2009 dated 26 October, which regulates active implantable medical devices). Accordingly, the total number of pacemakers used and their distribution by autonomous community was obtained through collaboration with pacemaker suppliers in Spain; this information is also regularly forwarded to the European Confederation of Medical Suppliers Associations (EUCOMED).
Report of the Spanish National Institute of StatisticsThe population data of Spain as a whole or by autonomous community for the various pacing-related calculations were taken from the latest updated provisional census of the Spanish National Institute of Statistics (Instituto Nacional de Estadística) of 2013.22
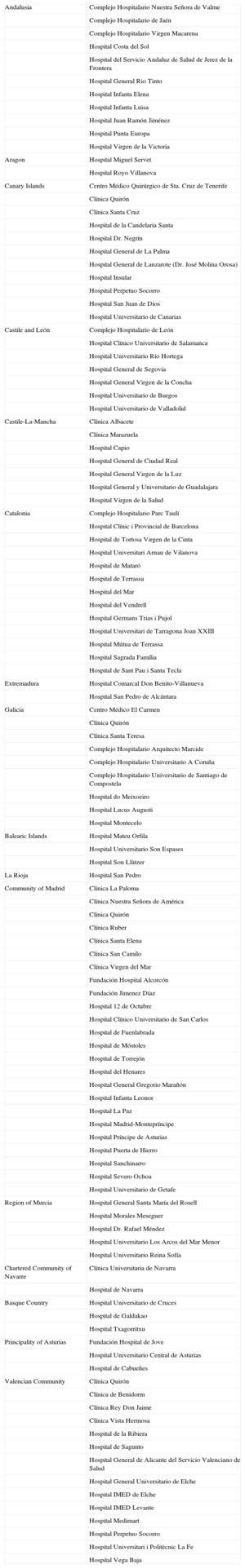
Sample AnalyzedThe results correspond to the analysis of the activity sent to the SPR from 118 hospital centers (Table), comprising 35% of the generators implanted, which was considered sufficient to evaluate the various aspects of cardiac pacing with pacemakers in Spain. The structure follows that of previous reports.
Public and Private Hospitals That Submitted Data to the Spanish Pacemaker Registry in 2013, Grouped by Autonomous Community
| Andalusia | Complejo Hospitalario Nuestra Señora de Valme |
| Complejo Hospitalario de Jaén | |
| Complejo Hospitalario Virgen Macarena | |
| Hospital Costa del Sol | |
| Hospital del Servicio Andaluz de Salud de Jerez de la Frontera | |
| Hospital General Rio Tinto | |
| Hospital Infanta Elena | |
| Hospital Infanta Luisa | |
| Hospital Juan Ramón Jiménez | |
| Hospital Punta Europa | |
| Hospital Virgen de la Victoria | |
| Aragon | Hospital Miguel Servet |
| Hospital Royo Villanova | |
| Canary Islands | Centro Médico Quirúrgico de Sta. Cruz de Tenerife |
| Clínica Quirón | |
| Clínica Santa Cruz | |
| Hospital de la Candelaria Santa | |
| Hospital Dr. Negrín | |
| Hospital General de La Palma | |
| Hospital General de Lanzarote (Dr. José Molina Orosa) | |
| Hospital Insular | |
| Hospital Perpetuo Socorro | |
| Hospital San Juan de Dios | |
| Hospital Universitario de Canarias | |
| Castile and León | Complejo Hospitalario de León |
| Hospital Clínico Universitario de Salamanca | |
| Hospital Universitario Río Hortega | |
| Hospital General de Segovia | |
| Hospital General Virgen de la Concha | |
| Hospital Universitario de Burgos | |
| Hospital Universitario de Valladolid | |
| Castile-La-Mancha | Clínica Albacete |
| Clínica Marazuela | |
| Hospital Capio | |
| Hospital General de Ciudad Real | |
| Hospital General Virgen de la Luz | |
| Hospital General y Universitario de Guadalajara | |
| Hospital Virgen de la Salud | |
| Catalonia | Complejo Hospitalario Parc Taulí |
| Hospital Clínic i Provincial de Barcelona | |
| Hospital de Tortosa Virgen de la Cinta | |
| Hospital Universitari Arnau de Vilanova | |
| Hospital de Mataró | |
| Hospital de Terrassa | |
| Hospital del Mar | |
| Hospital del Vendrell | |
| Hospital Germans Trias i Pujol | |
| Hospital Universitari de Tarragona Joan XXIII | |
| Hospital Mútua de Terrassa | |
| Hospital Sagrada Família | |
| Hospital de Sant Pau i Santa Tecla | |
| Extremadura | Hospital Comarcal Don Benito-Villanueva |
| Hospital San Pedro de Alcántara | |
| Galicia | Centro Médico El Carmen |
| Clínica Quirón | |
| Clínica Santa Teresa | |
| Complejo Hospitalario Arquitecto Marcide | |
| Complejo Hospitalario Universitario A Coruña | |
| Complejo Hospitalario Universitario de Santiago de Compostela | |
| Hospital do Meixoeiro | |
| Hospital Lucus Augusti | |
| Hospital Montecelo | |
| Balearic Islands | Hospital Mateu Orfila |
| Hospital Universitario Son Espases | |
| Hospital Son Llàtzer | |
| La Rioja | Hospital San Pedro |
| Community of Madrid | Clínica La Paloma |
| Clínica Nuestra Señora de América | |
| Clínica Quirón | |
| Clínica Ruber | |
| Clínica Santa Elena | |
| Clínica San Camilo | |
| Clínica Virgen del Mar | |
| Fundación Hospital Alcorcón | |
| Fundación Jimenez Díaz | |
| Hospital 12 de Octubre | |
| Hospital Clínico Universitario de San Carlos | |
| Hospital de Fuenlabrada | |
| Hospital de Móstoles | |
| Hospital de Torrejón | |
| Hospital del Henares | |
| Hospital General Gregorio Marañón | |
| Hospital Infanta Leonor | |
| Hospital La Paz | |
| Hospital Madrid-Montepríncipe | |
| Hospital Príncipe de Asturias | |
| Hospital Puerta de Hierro | |
| Hospital Sanchinarro | |
| Hospital Severo Ochoa | |
| Hospital Universitario de Getafe | |
| Region of Murcia | Hospital General Santa María del Rosell |
| Hospital Morales Meseguer | |
| Hospital Dr. Rafael Méndez | |
| Hospital Universitario Los Arcos del Mar Menor | |
| Hospital Universitario Reina Sofía | |
| Chartered Community of Navarre | Clínica Universitaria de Navarra |
| Hospital de Navarra | |
| Basque Country | Hospital Universitario de Cruces |
| Hospital de Galdakao | |
| Hospital Txagorritxu | |
| Principality of Asturias | Fundación Hospital de Jove |
| Hospital Universitario Central de Asturias | |
| Hospital de Cabueñes | |
| Valencian Community | Clínica Quirón |
| Clínica de Benidorm | |
| Clínica Rey Don Jaime | |
| Clínica Vista Hermosa | |
| Hospital de la Ribiera | |
| Hospital de Sagunto | |
| Hospital General de Alicante del Servicio Valenciano de Salud | |
| Hospital General Universitario de Elche | |
| Hospital IMED de Elche | |
| Hospital IMED Levante | |
| Hospital Medimart | |
| Hospital Perpetuo Socorro | |
| Hospital Universitari i Politècnic La Fe | |
| Hospital Vega Baja |
According to the data provided by the device manufacturers, a total of 36 042 pacemaker generators were used in 2013 in first implantations and replacements. Of these, 848 were biventricular pacemakers for cardiac resynchronization therapy (CRT) using low-energy electrical impulses or cardiac resynchronization devices without defibrillation capability (CRT-P). As usual, slight discrepancies were seen from the information provided by the companies to the EUCOMED (reporting a total of 36 424 generators, including 854 CRT-P devices). The number of total units increased by 2.6% compared with the previous year.
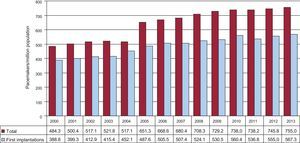
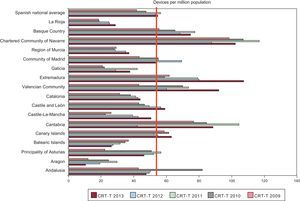
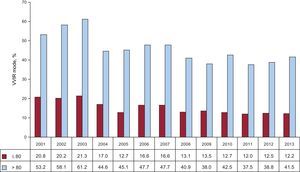
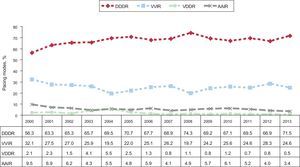
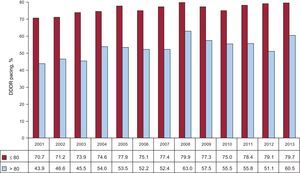
The latest available census data from the Spanish National Institute of Statistics (provisional results published July 1st 2013) recorded a population of 46609000, 22941000 men and 23668000 women, indicating an estimated decrease of 118238 people during the first half of 2013. According to the SPR data, 755 pacemaker generators were used per million population (units/million) (781.4 if CRT-P devices are included) (Figure 1); this figure is lower than the mean of those countries sending data to the EUCOMED (933 units/million) but is somewhat higher than those countries such as the Netherlands, Norway, the United Kingdom, and Switzerland.
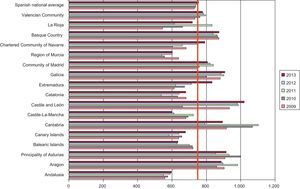
There were notable regional differences9–13 among autonomous communities in the number of units per million population, with clear increases in some regions in northern Spain. Thus, in 2013, there were 1000 units/million in Castile and León, followed by Galicia and the Principality of Asturias with more than 900 units (Figure 2), which, as in previous analyses, are the autonomous communities with the highest mean age.
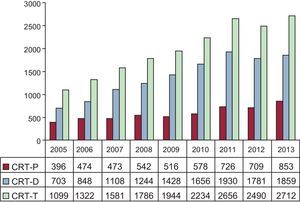
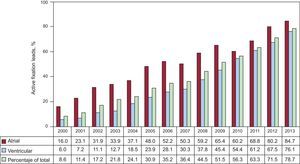
Pacing Devices for Ventricular ResynchronizationThe number of CRT devices was 58.1 units/million according to the EUCOMED data and 54.7 units/million according to the SPR, with a slight increase from the previous year in both devices with and without implantable cardioverter defibrillators, although the increase was slightly higher for pacing only devices (Figure 3). There were 18.2 units/million CRT-P devices; Spain continues to be one of the European countries with fewest CRT implants per million population.23,24
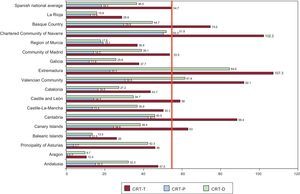
The use of CRT also showed marked interterritorial differences among autonomous communities, with a profile similar to that of other years analyzed; most implantations per million population were performed in Extremadura and the Chartered Community of Navarre, exceeding 100 units/million. These regions were followed, in order of frequency, by the Valencian Community and Basque Country. Details on the other regions, the type of CRT used (with or without implantable cardioverter defibrillator), and the changes over the last 5 years can be seen in Figures 4 and 5.
Cardiac resynchronization devices implanted per million population in 2013, showing the Spanish national average (vertical line) and distribution by autonomous community. CRT-D, biventricular device with defibrillation capability; CRT-P, low-energy biventricular device; CRT-T, total number of cardiac resynchronization therapy devices.
In the data sent to the SPR in 2013, biventricular units comprised 1.8% of the total number of generators, 1.3% of first implantations, and 3.2% of replacements.
Age and Sex of the PopulationThe mean age of patients who underwent some type of intervention was 77.6 years, 77.4 years for first implantations and 78.2 years for generator replacements.
Most implantations (41.5%) were performed in the groups aged 80 to 89 years, followed, aged 70 to 79 years (34.7%), 60 to 69 years (12.6%), 90 to 99 years (6.1%), and 50 to 59 years (3.3%); none of the remaining 10-year age groups exceeded 1%. The replacements followed a similar order, with 42.8% in the group aged 80 to 89 years, 30.3% in that aged 70 to 79 years, 10.4% in that aged the 60 to 69 years, and 10.3% in the group aged 90 to 99 years. There was some activity in patients ≥ 100 years, representing 0.1% of implantations and 0.3% of generator replacements.
Similar to previous years, there were some differences between men and women. The mean age of implanted patients was slightly lower in men (77 years; 78.3 years in women) and the use of generators was higher in men (58.8%), for both first implantations (59.5%) and replacements (56.6%). This difference was similar to those of the other years analyzed.4–13 The use of generators was 604 units/million women and 892 units per million men, given the proportion of activity reported by sex to the SPR and the population distribution of the Spanish National Institute of Statistics.
Type of Procedure: Implantations and Generator ReplacementsPacemaker ImplantationsOf all generators used, 75.2% were first implantations, giving a frequency of 567 units per million (an increase of 12 units/million from the previous year and the highest number on record) (Figure 1).
Replacements and Their CausesPacemaker generator replacements comprised 24.8% of devices used, similar to recent years according to the time series data.
Generator replacements associated with lead substitution comprised 1.6% of the activity registered, the same as in other years with pacemaker data.
The most frequent cause of generator replacement was end-of-life battery depletion (90.5%), followed, in descending order, by infection or erosion of the generator pocket (3%; 1.6% due to infection), elective replacement (2.2%), system change (1.5%), change due to lead complications (1.4%), and premature battery depletion (0.9%), either due to high thresholds or to shorter than expected battery duration.
Pacemaker LeadsPolaritySimilar to recent years, almost all leads implanted were bipolar (99.7%), 99.9% for the atrial position and 99.8% for the right ventricle. Of the few unipolar leads used (0.3%), most were for epicardial pacing of the left ventricle through the coronary sinus (63.1%), followed by epicardial pacing of the right ventricle (31.5%) and atrium (2.6%) during cardiac surgery. Unipolar leads are possibly selected for their lower diameter when venous access problems arise, such as due to marked tortuosity, a narrow venous diameter, or the presence of multiple previous leads restricting the lumen of the vessel.
Lead Fixation SystemMost leads implanted (78.7% of all leads) used an active fixation mechanism involving a helix secured in the myocardium; its higher use in both cardiac chambers continues (Figure 6). The frequency of such implantations was again higher in the atrium (84.7% vs 76.1% in the right ventricle).
According to an analysis performed with a cutoff age of 80 years, the greater use of this system is independent of patient age. The use was similar for both age groups and cardiac chamber analyzed. Thus, an active fixation mechanism was used in 76.7% and 78.8% of all leads implanted in patients > 80 years and < 80 years, respectively, as well as in 84.8% and 84.6% of leads implanted in the atrium and 74.1% and 76.4% of leads implanted in the right ventricle, respectively.
Magnetic Resonance-compatible LeadsIn 2013, leads specifically designed to protect against possible disturbances during magnetic resonance imaging were used in 18.8% of all implantations, in the atrium in 19.7% and in the ventricle in 18.3%. A slight decrease was seen from 2012,13 possibly because these generators belong to a higher-end and more expensive product range. This system should be required for all implanted leads, because it is impossible to predict if patients will need magnetic resonance imaging during their lifetimes.
Extraction and Replacement of Pacing LeadsOf all leads implanted in 2013, 1.5% required extraction. The most frequent cause of extraction was infection or ulceration (62.8% of cases), followed by insulation defects (11.4%), conductor breakage (8.7%), sensing problems (5.7%), exit block (similar percentage), and lead dislodgement (2.8%); the remainder were elective or unspecified.
Implantation of a new electrode lead comprised 1.8% of all procedures; 1.6% were for the substitution of a generator to improve hemodynamic function or due to damage of the lead before or during surgery. As in the previous year, 0.2% of procedures were performed exclusively for lead substitutions.
Symptoms, Causes, and Electrocardiographic Abnormalities Prior to ImplantationSymptomsThe most frequent clinical symptoms motivating implantation were syncope (41.6% of patients), dizziness (25.5%), dyspnea or signs of heart failure (16.4%), and bradycardia (10.2%); other less frequent symptoms or signs were tachycardia (1%), chest pain (0.9%), and resuscitated cardiac arrest due to bradyarrhythmia (0.3%). Asymptomatic patients received 3.2% of implantations and the remainder were performed in patients with uncoded symptoms. The profile was similar to that of previous years.9–13
CausesThe most frequent indications for implantation of a cardiac pacing system were presumptive fibrosis of the conduction system (44.3%) and unknown (41%), although both could be combined in the same group as the first cause is assigned after exclusion of other causes. These indications were followed by ischemia (5.5%; 0.25% in postischemic patients), valve disease (2.7%), and iatrogenic-therapeutic causes (2.5%; 0.7% of these after ablation of the atrioventricular node, whether intentional or not). Cardiomyopathies and hypertrophy constituted 2.4% and 0.5%, respectively. Neurally-mediated mechanisms comprised less than 1% (0.6% carotid sinus syndrome and 0.2% vasovagal syncope). Heart transplants and ionizing radiation were a minor cause (0.04% and 0.02%, respectively). The causes have changed little over the years analyzed.3–13
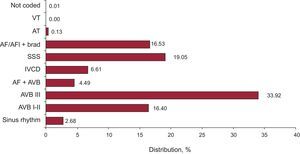
Electrocardiographic AbnormalitiesThe most frequent electrocardiographic abnormalities prior to implantation were atrioventricular conduction block (AVB) (54.8%) and various manifestations of sick sinus syndrome (SSS) except atrial fibrillation or atrial flutter with bradycardia (19%). Details of the groups and the changes over time are shown in Figures 7 and 8.
Electrocardiographic abnormalities prior to implantation in 2013. AF/AFl + brad, atrial fibrillation or atrial flutter with bradycardia; AF + AVB, atrial fibrillation with atrioventricular block; AT, atrial tachycardia; AVB, atrioventricular block; IVCD, intraventricular conduction defect; SSS, sick sinus syndrome; VT, ventricular tachycardia.
As in previous years,9–13 men had a higher incidence of conduction problems, both AVB and intraventricular conduction defects. There was a similar frequency of SSS in both sexes, with men:women ratios of 1.4, 3.0, 1.7, and 0.98 for AVB, intraventricular conduction defect, atrial fibrillation or atrial flutter with bradycardia, and SSS, respectively.
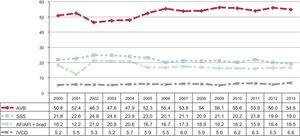
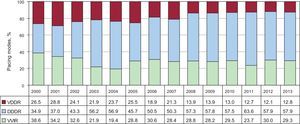
Pacing ModesSingle-chamber pacing comprised 41.3% of all generators used in 2013, with atrial pacing (AAIR) comprising just 0.6%. The lowest use of this mode was seen in 2013, confirming the trend toward its progressively lower use (Figure 9), both in first implantations (0.4%) and replacements (1.2%). The use of single-chamber ventricular pacing (VVIR), used in 40.7% of cases, has changed little since the previous decade (42.7% of implantations and 34.6% of replacements) (Figure 9). Given that, among electrocardiographic alterations, first implantations or replacements in patients with persistent atrial tachyarrhythmia represent 19.9% of procedures (21.0% of implantations and 16.2% of replacements), the estimated rate of patients paced in VVIR who could be paced in atrial synchronous pacing mode14,15 remained stable at around 20%; the factors affecting pacing mode selection are discussed in the next section.
Sequential dual-chamber pacing with 1 or 2 leads comprised 58.7% of procedures. Sequential pacing with a single lead (VDDR) was used in 13.3% of all units. Its use has tended to decrease in recent years, as shown by the ever-increasing gap between first implantations (10.1%) and replacements (22.9%). Dual-chamber pacing with 2 leads (DDDR) was the most widely used mode (45.4%), both in first implantations (46.6%) and in replacements (41.2%). One or more biosensors for detecting variations in pacing frequency were included in 87.4% of procedures (Figure 9).
After the decrease of the previous year, the use of biventricular pacing for CRT increased again, for both devices with and without defibrillators. Of the low-energy devices, 144 more were used than in the previous year (a 20% increase), reaching 18.2 units/million. Overall, the use of CRT devices (58.1 units/million) differed from the published means of other European countries24 and Spain showed the fewest CRT implantations of the countries reporting procedures to the EUCOMED.23
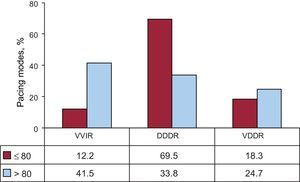
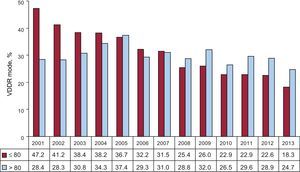
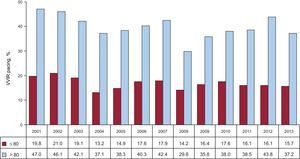
Pacing Mode SelectionPacing Conduction DisturbancesPacing in Atrioventricular Conduction Block. To evaluate the degree of compliance with pacing mode guidelines,14,17 this study was limited to patients in sinus rhythm and excluded those with persistent atrial tachyarrhythmia with AVB (code C8 of the EPPIC). Possible factors influencing pacing mode selection in this group were analyzed, such as age, sex, and degree of block. Although atrial synchronous pacing (DDDR and VDDR modes) was the most common at 74.4%, its use was slightly lower than in 201213 due to a decrease in VDDR (20.7%) that was not compensated for by a slight increase in DDDR (53.7%) (Figure 10). Analysis of pacing modes based on atrial synchronization by the distribution of the 2 usual age groups (cutoff of 80 years) showed a marked difference in its choice, 87.8% in those ≤ 80 years and 58.5% in those > 80 years, due to the greater use of DDDR mode in the 2 age groups (Figure 11). Older patients showed greater use of VDDR mode. Use of VDDR mode continued to decrease, reaching its lowest level since 2000 in both age groups (Figure 12), whereas DDDR mode increased in both age groups.
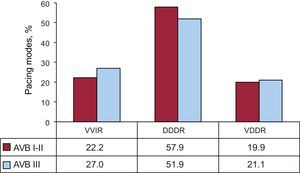
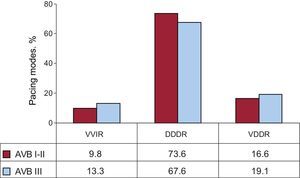
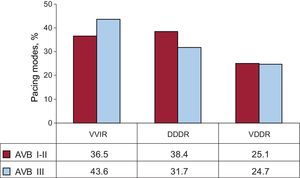
Comparison of atrial pacing by the degree of block between first- and second-degree AVB and third-degree AVB revealed a greater use in the former (77.8%) than in the latter (73.0%), due to greater use of DDDR in first- and second-degree AVB (Figure 13), as in previous years.9–13 This difference was maintained for these degrees of block regardless of patient age, although the gap was wider in those > 80 years (Figures 14 and 15). The choice of pacing mode was somewhat influenced by sex in both age groups; use of DDDR was higher in men than in other years analyzed,11–13 and VDDR was more frequent in women. Together, sequential pacing was used 3.5% less often in younger women and 3.8% less often in older women than in men. A high percentage of patients with AVB and sinus rhythm (25.6%) continued to have VVIR (Figure 10). This increased use was seen particularly in older patients (Figure 11), as in previous years (Figure 16), and was somewhat higher in those with third-degree AVB (Figure 13) and in women of both age groups.
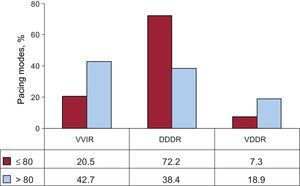
Pacing data in this group have changed little in recent years.5–13 Synchronous atrial pacing comprised 70.7%, the same as in 2012. The most frequently used mode was DDDR (57.9%), and VDDR comprised just 12.8%. Single-chamber ventricular pacing was the second most used mode (29.3%) (Figure 17). As for AVBs, age was a determining factor in mode selection: VVIR mode was used in 42.7% of those > 80 years vs 20.5% in those ≤ 80 years. Unlike in other years, VDDR mode was also affected by age (≤ 80, 7.3%; > 80, 18.9%) (Figure 18). In this group of electrocardiographic abnormalities, CRT-P devices for the treatment of ventricular dysfunction comprised 8.7% of all units implanted, with clear differences by age (3.9% in > 80 years vs 13.2% in ≤ 80 years) and with a markedly higher use in women of both age groups (≤ 80 years, 22.9% of women vs 10.5% of men; > 80, 9.0% of women vs 3.2% of men).
For the correct evaluation of the pacing modes for SSS and the degree of adherence to the modes most recommended in the current clinical guidelines,14,17 the present analysis was performed in 2 groups (as for AVB), separating those patients who theoretically have persistent atrial fibrillation or atrial flutter with bradycardia (code E6 of the EPPIC) from those who theoretically are in permanent sinus rhythm.
Sick Sinus Syndrome With Persistent Atrial Tachyarrhythmia. As expected, pacing was largely in VVIR mode (94.8%). However, as in other years, implantation of dual-chamber devices still comprised 5.2% (4.7% in DDDR), probably because these patients require reversion to sinus rhythm. Moreover, 0.5% of pacing was in VDDR mode, an inadequate mode for SSS, but possibly chosen because of technical problems in the passing of 2 leads, a situation we consider unlikely.
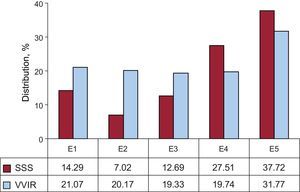
Sick Sinus Syndrome in sinus rhythm. In the other electrocardiographic manifestations of SSS, when patients should have a stable or intermittent sinus rhythm, pacing was largely performed in modes capable of atrial sensing and pacing (74.9%), as recommended for this group of patients14 (DDDR, 71.5%; AAIR, 3.4%). The use of AAIR fell to its lowest use of all recorded years4–13 (Figure 19). Pacing was performed with VVIR in 24% (the mean level for recent years) and with VDDR in 0.5%, both of which are less suitable for this type of disease. To try to evaluate if any of the electrocardiographic manifestations had a greater or lower influence on the above adherence to the recommended pacing mode, the type of pacing was analyzed separately for each subtype; the E7 and E8 subgroups of the EPPIC (interatrial block and chronotropic incompetence, respectively) were excluded due to their minimal representation in each year (< 0.5% in 2013). A rate of VVIR pacing of between 20% and 31% was seen, with the maximum value corresponding to tachycardia-bradycardia syndrome, as usual. This subgroup may incorrectly include patients with persistent slow-fast atrial fibrillation, who should be included in the already analyzed E6 subgroup (Figure 20).
Distribution in 2013 of single-chamber ventricular pacing and sick sinus syndrome according to the electrocardiographic codes of the European Pacemaker Patient Identification Card, excluding E7 and E8 (interatrial block and chronotropic incompetence, respectively) due to their low incidence. E1, sick sinus syndrome not specified; E2, exit block; E3, sinus arrest; E4, bradycardia; E5, bradycardia-tachycardia syndrome; SSS, sick sinus syndrome; VVIR, single-chamber ventricular pacing.
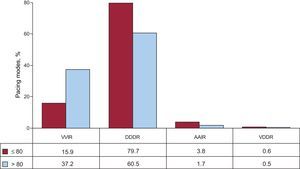
When age was studied as a factor affecting pacing mode selection, there was a marked difference in the use of pacing modes between the 2 age groups (cutoff of 80 years). Pacing with the capability of atrial sensing and pacing was used in 83.5% and 62.2% of those ≤ 80 and > 80 years, respectively (Figure 21). Single-chamber ventricular pacing was used in 15.7% and 37.2%, respectively. Use of AAIR continued to be low (3.8% and 1.7%, respectively). Both groups showed low use of VDDR (0.6% and 0.5%, respectively) (Figure 21). Age influenced the choice of mode in all years studied (Figures 22 and 23).
Sex as a factor affecting the choice of pacing mode showed a slight influence on appropriate mode selection in 2013. The use of VVIR mode was 1.5% higher in women in the ≤ 80 year group and was 4% higher in women in the > 80 year group (in previous years, the percentage was similar).
Home Monitoring/Follow-upIn 2013, 6% of all conventional pacemakers and 39% of all CRT units were included in home monitoring/follow-up programs.
DISCUSSIONAccording to the SPR data, the use of conventional pacemaker generators slightly increased in 2013 (2.8% more than in the previous year) due to population aging (with a progressive increase in the mean age at first implantation to 77 years), even as the population decreased. Pacemaker use in Spain reached 755 units/million, exceeding the mean of the 55 countries forwarding data to the European Heart Rhythm Association White Book20 of the European Society of Cardiology, which includes some non-European countries such as those of northern Africa (556 units/million in 2012, according to the latest data published). Nonetheless, pacemaker use was still below the mean of the 18 European countries reporting data to the EUCOMED (933 units/million).23 There was a higher percentage of implantations in men due to their higher incidence of intraventricular conduction defect and AVB.
The rate of implantations of CRT devices per million population has increased since 2012 (58.1 vs 53.1 units/million). This increase was largely due to CRT-P devices (16% more) because the number of CRT units with implantable cardioverter defibrillators (CRT-D) was lower than that recorded in 2011. The increase in CRT-P devices could be explained by the current economic situation, which would favor as much as possible the implantation of this type of device vs CRT-D devices. Nonetheless, Spain continues to be the country with the lowest number of total CRT and CRT-D implantations per million population and the third last of the 18 European countries in CRT-P implantations,23 a situation that has persisted since before 2007.24 Accordingly, this situation cannot be attributed to the current economic climate alone and a clear explanation is lacking, as there is no known delay in implantations, and the low number of implantations may be because there are fewer medical units able to perform these procedures. The CRT-P pacing mode was used in 8.6% of patients with intraventricular conduction defect and was more common in women than in men, both in those > 80 years (9.0% vs 3.2%, respectively) and in those ≤ 80 years (22.88% vs 10.47%, respectively). These figures could have been partly influenced by the data of the MADIT-CRT25 trial showing the greater efficacy of this therapy in women.
As in the previous reports of the registry, there were notable differences among the autonomous communities in the rates of implantations of conventional pacemakers and CRT devices, probably due to the differences in the mean ages of the populations and the unequal distribution of arrhythmia and heart failure units for patient referrals.
There was a predominance of bipolar leads and marked increase in the system of active fixation in recent years. It is already used in 78.7% of all leads, with an even higher percentage in the case of the atrium (84.7%). One of the main reasons for its widespread use is its versatility, which allows implantation in any point of the cardiac chambers or in alternative sites. This approach is becoming more and more common, partly to achieve a more physiological pacing pattern, which appears to reduce pacing-related deteriorations in ventricular function,26 as well as to improve the electrical performance of the leads and facilitate future removal if necessary. This year, there was no increase in the frequency of the use of leads compatible with magnetic resonance imaging (20%), which should be another standard for pacing. The criteria used for the selection of these leads are unknown, but their use should be increased given the impossibility of predicting which patients may one day need magnetic resonance imaging. Their use is expected to significantly increase in the coming years because marketing has begun of leads systematically compatible with magnetic resonance imaging at no additional cost, something that remains to happen with pacemaker generators.
In SSS, DDDR is the most commonly used mode, but there is still a considerably high percentage of VVIR pacing, especially in older patients (37.2% of those > 80 years). The progressive disuse of AAIR pacing is continuing, perhaps because of the results of the DANPACE trial,27 which linked AAIR pacing to a greater number of reinterventions and a higher incidence of atrial fibrillation compared with DDDR mode, results already incorporated into the European cardiac pacing guidelines of 2013.14 The mode of choice is DDDR, and AAIR pacing is an alternative. The guidelines discourage the use of VVIR devices because DDDR pacing in this situation offers advantages such as a moderately reduced incidence of atrial fibrillation and stroke and a lower risk of the development of pacemaker syndrome, a condition that impacts patient quality of life.
There is a continuing increase in the use of DDDR systems for AVB, resulting in a significantly reduced use of VDDR devices that are nonetheless effective in the long-term.28 A quarter of patients with AVB continue to receive single-chamber pacing. As in other registries, the choice of VVIR is influenced by age in patients with AVB (> 80 years, 41.4%; ≤ 80 years, 12.1%) and somewhat less by the degree of block (greater use in third-degree AVB) and sex (more in women).29 Although no clear scientific evidence is available on the survival benefits of dual-chamber pacing, there are data indicating an influence on quality of life and the possible development of heart failure. Individualization of the pacing mode decision is recommended,14 considering also that dual-chamber devices are more expensive and are associated with a slightly higher risk of complications. Pacing with DDDR continues to be the option of choice for patients with both persistent and intermittent AVB, even in the absence of concomitant SSS.
Use of follow-up and home monitoring systems in conventional pacemakers slightly increased, reaching 6%. Their use in CRT (39%) continues to be the highest in Europe.30 Their expanded use is restricted by difficulties in the organization of this type of assistance and the additional cost of these systems. However, this safe and cost-effective method permits the early detection of events and fewer face-to-face visits;31,32 thus, their use is expected to increase in the future.
CONCLUSIONSThe slow increase in the use of pacemakers and CRT devices continues, although their use is still below the mean of other European countries. The use of leads with active fixation has become widespread. Age and, to a lesser extent, sex influence correct adherence to the recommended pacing mode. Home monitoring of pacemakers is still far from being widespread.
CONFLICTS OF INTERESTSNone declared.