To the Editor:
Mitral regurgitation is a common complication of acute myocardial infarction, with a prevalence that ranges from 1.6% to 19%.1 Awareness of the precise mechanisms that produce the valvular regurgitation continue to be the subject of debate.2 Only a few data exist about acute ischemic mitral regurgitation that is not due to a mechanical complication. Even when the mitral regurgitation is mild,3 the active ischemia favors the appearance of transitory episodes of acute pulmonary edema. Transitory mitral regurgitation is common during short periods of ischemia4 and it denotes abnormal function of mitral leaflets that are normal as far as ventricular dysfunction is concerned. This clinical picture, though known in medical practice, is nevertheless uncommon, and because it concerns a transitory dysfunction is not usually diagnosed on imaging studies.
We report the case of a 47-year-old woman who was a smoker and had hypercholesterolemia. She was admitted to the coronary care unit with an acute coronary syndrome without ST elevation. Three months previously she had been admitted with an acute inferoposterior myocardial infarction with a peak creatine kinase of 468 U/L. Primary angioplasty was performed successfully and a conventional stent was implanted over a thrombotic occlusion of the proximal circumflex artery, with no other coronary lesions. On discharge, the left ventricular ejection fraction (LVEF) was conserved with no mitral regurgitation.
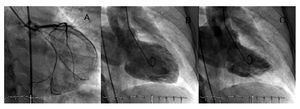
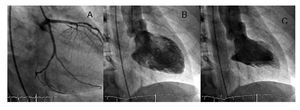
She was readmitted due to an episode of chest pain at rest and dyspnea. Auscultation revealed a fourth tone, a systolic murmur on the left sternal border, and rales at the base of both lungs. An ECG performed during the pain showed an inferolateral subendocardic lesion. She was treated with triple antiplatelet therapy and a catheterization was scheduled for 24 h later. Immediately prior to the procedure, the patient presented angina, dyspnea, and an arterial saturation of 86%, with pulmonary rales. A coronary angiogram showed diffuse restenosis in the stent, with subtotal occlusion of the proximal circumflex artery. The LVEF was slightly depressed, with posterior basal and diaphragmatic akinesis. She had severe mitral regurgitation causing complete opacification of the left atrium during the first beat (Figure 1). She underwent further angioplasty and a drug-eluting stent was successfully implanted. Clinical improvement was noted after reperfusion, with disappearance of the pain and the dyspnea. Another ventriculogram showed absence of the mitral regurgitation (Figure 2). An echocardiogram performed prior to discharge showed the LVEF to be normal, with no segmental alterations and mild mitral regurgitation.
Figure 1. Coronary angiogram showing subtotal occlusion of the proximal circumflex artery. Ventriculography at diastole (A) and systole (B) with the left atrium completely opaque in relation to the severe mitral regurgitation.
Figure 2. Coronary angiogram showing the proximal circumflex artery after implantation of the stent. Ventriculography at diastole (A) and systole (B) with absence of mitral regurgitation.
This case demonstrates that, after discarding other possible etiologies, such as papillary muscle rupture or incorrect positioning of the catheter during the ventriculography, it was the ischemia itself that caused the severe acute mitral regurgitation.
Current information about acute ischemic mitral regurgitation is based on experimental studies, such as that done by Kono et al,5 which showed that mitral regurgitation can be caused by regional dysfunction of the left ventricle at the origin of the papillary muscles.
Ischemia causes changes in the annulus, the subvalvular apparatus and the geometry of the mitral leaflets, and systolic dysfunction.6 Abnormalities in posterolateral contraction are those that most distort the morphology of the subvalvular mitral apparatus,7 and this territory is mainly affected after obstruction of the proximal circumflex artery.
This case illustrates the mechanisms mentioned above. The severe stenosis of the circumflex artery produced massive ischemic mitral regurgitation. The proximal location of the lesion resulted in an extensive area of inferoposterior ischemia, with the subsequent retraction of the posterior mitral leaflet and the lack of coaptation of the mitral leaflets. The resolution of the process after the angioplasty improved the segmental alterations and reverted the mitral regurgitation.