To the Editor:
We present the case of a 43-year-old man, a smoker of 20-30 cigarettes per day, who presented to the emergency department with melena. He reported a 1-week history of headache, and 10 days previously he was found to have hypertension at a single measurement (200/120 mm Hg). On questioning, he admitted sudden episodes of dizziness, muscle weakness, profuse sweating, and paleness, on occasions precipitated by defecation. Coinciding with these episodes, his stools were melenic.
On admission, the blood pressure was 140/90 mm Hg. A digital rectal examination revealed remains of stools and a fecal occult blood test was positive. The chest radiography and laboratory results showed no abnormalities. An electrocardiogram (ECG) showed sinus rhythm, left ventricular hypertrophy, and nonspecific repolarization alterations. He was admitted with a diagnosis of gastrointestinal hemorrhage.
On the first hospital day he had several short crises of chest pain, hypertension, profuse sweating, and nausea. Immediately afterwards, the ECG showed subepicardial ischemia. A computerized tomographic study of the chest ruled out aortic dissection. The ECG was eventually recorded during one of these crises and it showed ST segment elevation in leads V1 through V3, DII, DIII, and VF. A few minutes after the last episode he presented severe bradyarrhythmia, with secondary cardiac arrest. Advanced resuscitation maneuvers were applied for 35 min, with alternating episodes of asystole and ventricular fibrillation. A coronary angiogram, done immediately after he recovered stability, showed diffuse coronary spasm in the 3 coronary territories, with no major focal stenosis.
Since then the patient remained in a coma (Glasgow 5) on mechanical ventilation. The echocardiogram showed concentric left ventricular hypertrophy (posterior wall and septum, 15 mm), with no other alterations.
Over the following days several measurements were made of catecholamines, which showed a plasma epinephrine concentration of 282 pg/mL (normal, 20-60) and a norepinephrine concentration of 1346 pg/mL (normal, 300-650). The 24 h urinary excretion of epinephrine was 600 µg (normal, <18), of norepinephrine it was 1349 µg (normal, <390), and of vanilmandelic acid it was 12 mg/dL (normal, 2-8).
The patient died 14 days after admission following a further cardiac arrest secondary to extreme bradycardia, coinciding with a jugular puncture.
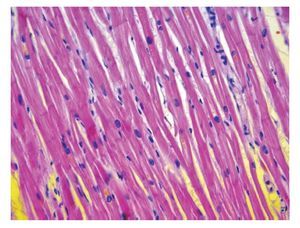
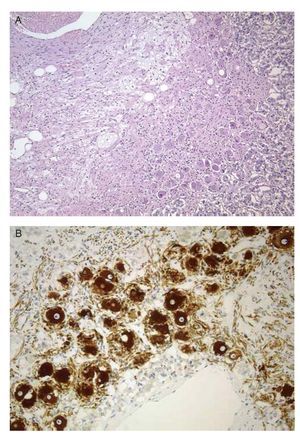
The autopsy revealed concentric left ventricular hypertrophy (795 g), with mild coronary atherosclerosis and diffuse subendocardial necrosis, with no data on hypertrophic cardiomyopathy (Figure 1). The right adrenal gland had a ganglioneuroma 1 cm in diameter, formed by a proliferation of well differentiated ganglion cells (Figure 2A), which stained positively with chromogranin
Figure 1. Histologic image of the interventricular septum that rules out hypertrophic cardiomyopathy.
Figure 2. The tumor showing mature ganglion cells, arranged on a fibrillary background (A), with immunohistochemical stain for chromogranin A, which confirms the nature of the ganglion cells (B).
A antibodies (Figure 2B) and sinaptofisin, on a fibrillary background that stained positively with neurofilaments and S-100 protein. There was no component suggestive of pheochromocytoma. The central nervous system showed data of anoxic encephalopathy.
Catecholamine synthesis by ganglioneuromas is well documented and presents a similar clinical profile to that seen in the patient reported here.1-3 Most cases are associated with hypertension, both in children and in adults.4-7 Very occasionally, a few cases have been associated with hypotension or shock triggered by trauma or stress.2,8 ST elevation in the leads corresponding to different vascular territories is better explained by generalized vasoconstriction secondary to an increase in the catecholamines rather than by a complicated atherosclerotic lesion, a hypothesis that is corroborated during coronary angiography. With the exception of the cardiac hypertrophy, the other findings at autopsy can be explained by the prolonged cardiopulmonary arrest. The cause of the cardiac hypertrophy could not be established, although it might have been due to the hypertension. However, as far as we are aware, the hypertension was only present for a short time before admission.