Keywords
INTRODUCTION
The development of drug-eluting stents (DES) has resulted in important benefits related to the incidence of restenosis and the need for new interventions.1 Following the initial enthusiasm about these devices, which has favored their gradual widespread use, the knowledge that late thrombosis can occur, the need to prolong dual antiplatelet therapy to reduce the incidence of thrombotic complications, and the fact that restenosis is not eliminated has led to a general reassessment of the indications for DES.2-4
Elderly patients, particularly those older than 80 years, are usually excluded from large clinical trials because of the study design, or are included in very low numbers.5 This fact has prevented subanalyses in this age group. In the specific setting of coronary revascularization, the number of elderly patients referred to the catheterization laboratory for coronary angiography is increasing as a consequence of aging of the population and the progressive departure from decision criteria solely based on age.6 Despite this fact, advanced age continues to be associated with less intensive use of diagnostic and therapeutic resources.7-10
Currently, there are no reasons to suspect that DES are less effective in terms of restenosis in very elderly patients. Nonetheless, the greater comorbidity in this population might make them more susceptible to complications due to the dual antiplatelet therapy required and the more frequent need for interruptions of this treatment. These concerns about safety may be the reason why DES are used relatively less often in the very elderly population.11 It is unknown whether the benefit of averting additional revascularization procedures in these patients would offset the presumably higher rate of complications derived from the need to maintain antiplatelet therapy.
The primary aim of the present study is to analyze safety in terms of stent thrombosis and long-term mortality, and efficacy in reducing major acute cardiac events (MACE) associated with DES use in patients older than 80 in daily clinical practice. This was done by comparing the evolution of patients who received DES to that of patients in the same period who received only conventional bare-metal stents.
METHODS
A retrospective observational study was conducted in a historical cohort of patients, with the primary aim of comparing the safety of DES use with that of bare-metal stent use in octogenarian patients in the routine clinical setting, as indicated by the incidence of stent thrombosis and all-cause deaths. The secondary aim was to compare the efficacy of DES versus conventional stenting in the same population, as related to the need for a new revascularization procedure for the treated lesion, and the combined outcome event of death, nonfatal infarction, and a new revascularization requirement.
Patient Selection
The patients included were all those older than 80 years referred to our catheterization laboratory for coronary angiography to investigate suspected ischemic heart disease between March 1, 2002 and November 30, 2006, and who received at least 1 coronary stent. Patients were excluded if they had a diagnosis of valve disease for which surgery was indicated and those in whom the indication was only left ventricular dysfunction or any cardiomyopathy with no evidence of ischemia on a noninvasive test. We also excluded patients who could not be followed up at long-term because they had no permanent residence and contact was impossible. For the analysis and comparison, the sample was divided into 2 groups: DES group, comprised of patients who had received at least one of these devices, and bare-metal stent group, including patients whose stents were not DES.
Treatment
In accordance with routine practice in the hospital where the study was conducted, the indication for revascularization was decided in each individual case by consensus between the attending physician and the interventional radiologist, based on the clinical picture, coronary anatomy, and the patient's personal opinion. The interventional technique used, devices implanted, and use of glycoprotein (GP) IIb/IIIa receptor inhibitors were at the discretion of the interventional radiologist responsible for the procedure. The choice of stent was decided by the interventional radiologist and the attending physician, based on the patient's clinical and angiographic characteristics. Before the procedure, all patients received aspirin (100 mg/d or a loading dose of 300 mg), intravenous sodium heparin adjusted to the patient's body weight, and clopidogrel (loading dose of 300 mg, followed by 75 mg/d for 4 weeks thereafter in the case of bare-metal stents or 1 year thereafter in the case of DES). The antiplatelet regimen remained invariable during the inclusion period.
Variables
The patients' baseline characteristics and the outcome of the procedure were obtained from the study hospital's clinical records, the registry of procedures in the hospital's catheterization laboratory, and an examination of the angiography recording. Renal failure was defined as a creatinine concentration of >2 mg/dL before the procedure. The reference length and diameter of the lesions treated were assessed by visual estimation on the part of the interventional radiologist responsible for the procedure. A death was considered to have a cardiac cause when a cardiac origin could be confirmed and when a patient died of an unknown cause.12 The combined event, MACE, was established as death by any cause, nonfatal acute myocardial infarction (defined by a hospital admission with that diagnosis) and the need for an additional coronary revascularization procedure for any of the treated arteries. Thrombosis was defined according to the criteria of the Academic Research Consortium (ARC).12
Follow-up
Patients were followed up by telephone contact and by consulting the clinical records for those who were rehospitalized. Follow-up was carried out according to survival analysis methods for the period of December 2007 to January 2008, so that all patients had at least 1 year of follow-up. If there were any questions regarding a particular event, the patient was asked to come to the hospital or send the clinical report describing the event.
Statistical Analysis
The continuous variables are expressed as the mean (SD) and qualitative variables as absolute values and percentages. The differences between groups were calculated using the Student t test for continuous variables and the c2 test for proportions. Event-free survival (which excluded death from any cause, death from a cardiac cause, acute myocardial infarction, coronary revascularization for a treated artery, and MACE) was analyzed by the Kaplan-Meier method, and between-group comparisons with the log-rank test. Two Cox analyses were performed. The first, which analyzed the safety of DES, included the combined event of all-cause death plus confirmed or probable stent thrombosis as the dependent variable. The second, which analyzed the efficacy of DES, had the combined event MACE as the dependent variable. The independent variables included in both models were the variables at the time of coronary angiography significantly associated with the events analyzed in the bivariate analysis, together with those reported in the literature to be associated with a poorer prognosis in coronary disease. Because of the differences in the duration of follow-up between patients treated or not with DES, the 2 Cox analyses performed were limited to the events occurring in the first year following the procedure. The resulting Cox models were then adjusted by a propensity score, obtained by constructing a logistic regression model with the variables that could be associated with the fact of using DES.13,14 Through this model, the individual probability of receiving a DES was obtained, and this factor was included as an independent variable in the 2 Cox models. The first-level interactions between the variables were then assessed and those that were significant were retained in the models. The predictive power of the model used to obtained the propensity score was evaluated by calculating the area under the receiver operating characteristic (ROC) curve, performed with the above mentioned individual probability of receiving a DES versus having actually received one. The statistical analyses were performed with SPSS (version 15.0) and PASS-2008/NCSS-2007 for Windows.
RESULTS
Baseline Characteristics and Procedure Characteristics
During the study period, 176 octogenarians were treated by stent placement in our hospital (90 with DES and 86 with bare-metal stents). Baseline characteristics of the patients are shown in Table 1. The DES-treated patients had a more unfavorable angiographic profile, with significantly more frequent involvement of the left main coronary artery and severe calcifications, a larger number of bifurcation and ostial lesions, and more frequent multivessel disease with a larger number of affected vessels, treated vessels, treated lesions, stents implanted, and stents per patient, as well as longer lesions and smaller diameter lesions. Patients with DES also received treatment of the left main coronary artery and left anterior descending artery significantly more often than those with bare-metal stents. The following types of DES were used: paclitaxel-releasing Taxus stents (Boston Scientific Corporation, Natick, MA, United States) in 43% of patients, zotarolimus-releasing Endeavor stents (Medtronic Vascular, Santa Rosa, CA, United States) in 46%, and rapamycin-releasing Cypher stents (Cordis, Johnson & Johnson, Warren, NJ, United States) in 13%.
Events During Follow-up
Complete follow-up was achieved in 173 (98.3%) patients. One patient was lost to follow-up in the DES group and 2 in the bare-metal stent group. Mean follow-up was 26.3 (12.9) months, with a median follow-up of 21.5 (25th-75th percentiles, 15-37) months. DES use increased during the enrollment period and resulted in a significantly shorter follow-up time for DES patients (19.1 [7] vs 34.3 [13] months; P<.0005). There were no significant differences between the groups in the complications occurring during hospitalization, with the exception of a nonsignificant trend toward development of inhospital bleeding and worsening renal function in those treated with DES (Table 2). Seven patients in the DES group and 6 in the bare-metal stent group died of cardiogenic shock, another patient died of cardiac tamponade in the bare-metal stent group, and another of sudden death in the DES group.
In all patients who underwent treatment of the left main coronary artery, revascularization surgery had been rejected because of a high surgical risk. Among the 18 patients with this condition who were treated with DES, 2 died during hospitalization for revascularization, (both patients were in cardiogenic shock within an ST-segment elevation acute coronary syndrome), another died at 19 months due to congestive heart failure with no evidence of ischemic coronary events, and a fourth patient died at 12 months due to infarction secondary to occlusion of another artery.
Bare-metal stents were additionally implanted in 19 patients from the DES group. In patients who underwent bare-metal stent placement together with a DES, there were no cases of confirmed or probable thrombosis, nonfatal infarction, or a need for new revascularization of the bare-metal stents implanted.
There were no significant differences between the 2 treatment groups during the first year of follow-up with regard to the development of clinical events, except for a greater need to repeat coronary angiography (unscheduled) in the DES group. There was a nonsignificant trend to a higher rate of revascularizations for treated vessels in DES patients.
Thrombosis During Follow-upConfirmed thromboses were not observed, but there was a higher incidence of probable thrombosis in patients with a DES (5.6% vs 3.5%), although the difference was not statistically significant. No stent thromboses occurred after 6 months postimplantation. In patients with DES, there was 1 case of probable acute thrombosis and 2 cases of probable thrombosis during hospitalization. In addition, 1 sudden death at home 1 month following transplantation and 1 nonfatal inferior infarction 5 months after treatment in this group were attributed to probable thrombosis. In patients without a DES, the 3 probable thromboses presented as in-hospital reinfarction in 2 patients, and an anterior infarction 2 months after treatment leading to death in the third patent.
Survival Analysis and Multivariate Analysis
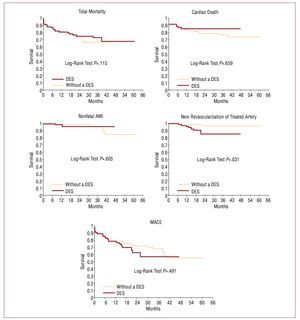
In the unadjusted survival analyses performed for each of the clinical events, there were no significant differences between the groups except in the need for new revascularization of the treated vessel, which was higher in patients with DES (Figure).
Figure 1. Distribution over time of confirmed and probable stent thromboses observed during follow-up according to the type of stent implanted. AMI indicates acute myocardial infarction; DES, drug-eluting stent; MACE, major acute coronary events.
In the logistic regression model performed to obtain a logistic propensity score, all first-level interactions between the variables were excluded because statistical significance had not been reached. The final model (Table 3) had a predictive value of 90.4% (95% confidence interval [CI], 86-94.8) determined by the area under the ROC curve. In the 2 Cox models performed, only left ventricular function and success of the procedure were independent predictors of events. These results were maintained after adjusting by the previously calculated propensity score. As indicated by the presence of the events analyzed, DES use was not independently associated with a different mortality outcome (Table 4).
DISCUSSION
The present study was designed to analyze the safety and efficacy of DES in an unselected population of octogenarian patients with an indication for revascularization. Although patients receiving DES had more unfavorable angiographic characteristics than those treated only with bare-metal stents, there were no significant differences between the 2 groups with regard to mortality, stent thrombosis, or the combined event of death, nonfatal AMI, and the need for a new revascularization of the treated vessel.
Safety in Relation to Death
Despite the fact that patients with DES had a more unfavorable angiographic profile than those who received bare-metal stents (treatment of the left main coronary artery in 20% of patients vs 1.2%, respectively; multivessel procedures in 54% vs 14%; 1.74 treated vessels vs 1.17; lesions significantly longer and vessel diameters smaller in the DES group), overall mortality, cardiac mortality, and the incidence of nonfatal AMI were similar in the 2 groups. As to major adverse events, the potential benefits obtained from DES probably counterbalanced the possible complications associated with DES use and the need for dual antiplatelet therapy, thus resulting in comparable events between a more severely affected patient group and one with less unfavorable coronary disease. DES use was not associated with greater long-term mortality or with MACE after adjusting for the clinical variables that could differentiate between the 2 subpopulations being compared.
Safety in Relation to Thrombosis
We found no significant differences between patients treated with DES or bare-metal stents in terms of the incidence of subacute or late stent thrombosis. Nonetheless, the presence of probable thrombosis according to ARC12 criteria was elevated in both groups, particularly in patients with DES (5.6%). This value is substantially higher than the 3% reported by Vlaar et al15 in a previous study in octogenarians, although the number of lesions treated, patients with multivessel disease, procedures performed in AMI, and particularly, number of DES implanted per patient (1.3) were clearly lower than in our series (number of DES, 1.96). The figure reported by Costa et al16 was also notably lower, although, again, the angiographic and clinical characteristics (absence of ST elevation coronary syndromes) were less unfavorable.
Advanced age has not been associated with a higher risk of stent thrombosis in any of the related studies.17-20 A recent observational study in unselected patients has indicated a higher incidence in younger patients, although the number of octogenarians included was not reported and only confirmed thromboses were analyzed.21 The high incidence of probable thromboses found in our study may be related more to the poor clinical and angiographic profile of the DES-treated patients than to any idiosyncrasy inherent to advanced age.
Safety in Relation to Hemorrhages
The risk of bleeding and the need for early withdrawal of dual antiplatelet therapy in elderly patients treated with DES were not contemplated among the aims of the study. In the first year, there was a 6% incidence of hospitalizations for anemia or hemorrhage in both groups, without significant differences (Table 4). However, these results should be viewed with caution considering the characteristics of our study (observational and retrospective). Although no deaths were detected in which the main cause was bleeding, we cannot specify whether some patients who died of neoplastic disease or sudden death at home might have been affected by anemia or bleeding. The values observed in our study, which encompass only hospitalizations for this cause (systematic follow-up analyses or other examinations were not performed), may very well underestimate this problem in the elderly population, which should be the subject of future studies with an appropriate design.
Clinical Efficacy
This was not a randomized study and the 2 groups compared were clearly different, particularly in their baseline angiographic characteristics. The indication for DES use in our study was mainly based on angiographic criteria, which were much more unfavorable in patients who received a DES. This may explain the paradoxical fact that patients treated with DES had a higher rate of revascularizations of treated vessels than those who received only bare-metal stents. Previous studies in octogenarians have shown treated lesion revascularization values of 4%22 and 4.8%,15 but the characteristics of the patients and lesions included were clearly more favorable than those in the present study. In a study comparing 2 historic series of patients older than 65 treated with stents before and after DES had been developed,23 patients who received DES presented a significantly lower rate of new revascularizations, nonfatal infarctions, and mortality during follow-up than those who had bare-metal stents.
We believe that in our series the use of DES in octogenarian patients with very unfavorable angiographic characteristics resulted in clinical outcomes similar to those achieved in patients with a more favorable anatomy treated with conventional bare-metal stents. In light of the benefits that can be obtained with the use of these devices and while waiting for data from randomized studies specifically for the elderly, DES use should not be limited in these patients solely because of their age. Instead, the decision to treat with a DES should be individualized and based on the clinical and angiographic characteristics of each patient.
Limitations
Because this is an observational study, it was not possible to know if all potentially confounding variables were controlled in the 2 groups studied, despite the adjustment that was carried out. Nevertheless, in contrast to a clinical trial, the study examines daily clinical practice and the expected results with the use of DES in octogenarians, without the restrictions inherent to clinical trials.
A larger number of patients might have provided more data on the true difference in thrombosis rates in the 2 groups and limited the effect of chance on the data observed. It might also have enabled an analysis of the events according to the type of DES used. With a sample size of 176 patients, it would have been possible to detect a hazard ratio of 2.17 as significant (power, 80%; alpha error = .05; 1-year incidence of the event [MACE], 20%; R2 of DES use vs the remaining variables, 0.1; and SD=0.5).
CONCLUSIONS
The results of the present study indicate that DES can be safely used in patients aged 80 years or older with complex coronary lesions and the long-term prognosis will be similar to that of patients with a more favorable coronary anatomy. In view of the characteristics of elderly patients, in particular regarding the extent and complexity of their coronary disease and their possible limitations for strict compliance with a dual antiplatelet regimen, specific clinical trials should be conducted to analyze the outcome of DES in this population subgroup.
ABBREVIATIONS
AMI: acute myocardial infarction
DES: drug-eluting stent
MACE: major adverse cardiac events
Correspondence: Dr. R. López Palop.
Vía Láctea, 38. Urbanización la Glorieta. 30110 Churra. Murcia. España.
E-mail: mlopezs@meditex.es
Received February 19, 2009.
Accepted for publication June 23, 2009.