To the Editor,
We present the case of a 3-month-old infant girl weighing 5 kg who was transferred to our center from another hospital presenting vomiting and tachypnea, with a diagnosis of supraventricular tachycardia, tachycardia-induced cardiomyopathy, and cardiac failure refractory to pharmacological treatment with amiodarone, flecainide, and digoxin. During physical examination, the patient was intubated and had bad peripheral perfusion, peripheral coldness and blood pressure <50 mm Hg despite treatment with dopamine.
The electrocardiogram showed atrial tachycardia with (+) P waves in leads II, III, and aVF, (-) in aVL and (+/-) in lead I. The transthoracic echocardiogram showed a highly dilatated left ventricle with a 25% ejection fraction. Electrophysiological study was conducted, which confirmed automatic tachycardia in left atrium at 224 beats/min (atrio-atrial interval, 268 ms).
Catheterization was performed via the right femoral vein, but the oval foramen was found to be closed. In light of this, a Goodale Lubin catheter (Medtronic) was supported on the septal orifice and rotating maneuvers were conducted using a coronary Cross-IT 200 guidewire which passed to the pulmonary veins. Next, the fossa ovalis was predilated using a 1.5, 2, and 3.5 mm diameter Apex (Boston Scientific) coronary balloon catheter. Left femoral vein puncture was performed and a 6 Fr ablation catheter (Biosense Webster) was advanced parallel to and over the guidewire, crossing the previously dilated oval foramen with no difficulty.
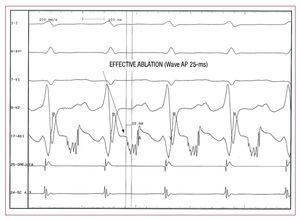
During tachycardia, the left atrium and pulmonary veins were mapped. Proximal to the left inferior pulmonary vein ostium, a fractionated atrial electrogram of 60 ms of duration was found, with an activation time of 25 ms preceding the P-wave (Figure 1). At this level, a single application was performed at 45 W and a mean temperature of 55oC for 12 s. This eliminated the tachycardia within the first second of administration (Figure 2). The patient entered sinus rhythm at 163 beat/min, with P-wave morphology in sinus rhythm. Immediately after entering sinus rhythm, blood pressure increased.
Figure 1. Intracavitary recording of the ablation catheter, auricle of right atrium and distal coronary sinus. Radiofrequency ablation site, showing a premature 25-ms AP.
Figure 2.ECG recording of atrial tachycardia at 229 beat/min (atrio-atrial interval, 262 ms) and entering sinus rhythm at 164 beat/min (atrio-atrial interval, 366 ms) during effective ablation.
The patient evolved satisfactorily, cardiac output normalized within the following hours and she showed progressive clinical improvement. Two weeks later, Doppler ultrasound echocardiogram showed that parameters were within the normal range. Twenty days after ablation she was discharged from hospital.
Those patients diagnosed with atrial tachycardia showing higher heart rates seem to be more at risk of developing cardiomyopathy. It is unknown why some of these patients develop cardiomyopathy whereas others maintain normal ventricular function.1 The treatment of choice for atrial tachycardia when the clinical symptoms are significant is radiofrequency ablation.2
To perform ablation in the left atrium, the interatrial septum is normally passed through. In children, this procedure is usually done via a patent oval foramen, since this does not normally close until age 5 in 50% of the population and until age 20 in 75% of the population.3 Catheters can also be placed in the left atrium via an arterial retrograde approach, advancing through the mitral valve, but this is more difficult.
We report the case of ablation radiofrequency for atrial tachycardia in an 3-month-old infant presenting congestive heart failure, secondary to a severe tachycardia-induced cardiomyopathy. In this case, the oval foramen was closed and had to be perforated using a coronary guidewire (using the soft tip) and rotating maneuvers. The method used to perforate the oval foramen was novel and an alternative to transeptal catheterization and the radiofrequency technique. We used a Cross-It 200 guidewire (Guidant) normally used to completely unblock coronary vessels, which is characterized by a greater push capacity, as well as a sharp distal end of up to 0.010 inches, capable of perforating cardiac structures and atresic valves using a rotating maneuver, as demonstrated in this report.4