To the Editor,
The formation of an aneurysm in the ventricular wall, due to thinning and dilatation, is a relatively common complication after transmural myocardial infarction.1 It can be associated with the formation of an adjacent intraventricular thrombus, form the substrate of ventricular arrhythmias, or encourage remodeling and dilatation of the left ventricular chamber. On rare occasions, a rupture may occur outside the acute phase of the infarction.
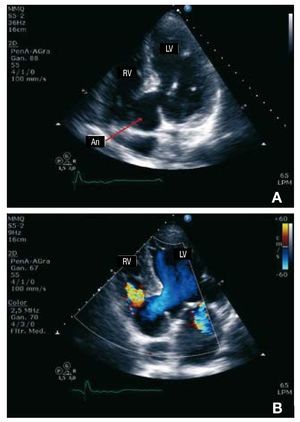
We present the case of a 77-year-old man with an inferior infarction not treated with fibrinolytic therapy in 2006, who subsequently underwent percutaneous revascularization. The patient was admitted to our center due to intermittent thoracic pain episodes lasting several hours and with atypical characteristics which had begun 1 month before. The ECG showed inferior Q-wave infarction, and physical examination revealed systolic-diastolic murmur with thrill more audible at the left sternal border. A transthoracic echocardiogram was performed, which detected an echo-free cavity (An) communicating with the left ventricle (LV) at the basal level of the posterior septum. It presented a narrow neck and inflow from the LV at systole, protruding toward the right ventricle (VD) (Figure 1A). A solution of continuity was observed between the cavity wall and the body of the right ventricle. Flow was present at systole and diastole (Figure 1B) with a systolic gradient of 80 mm Hg, creating a restrictive ventricular septal defect through it. Thinning and basal inferior akinesia was also observed, with preserved contractility in the other segments and normal overall systolic function. Given the background and the echocardiographic findings, the patient was diagnosed as presenting a basal septal aneurysm of the left ventricle that had undergone rupture and fistulization toward the right ventricle. It was concluded that the solution of continuity could increase, and so the patient was referred to cardiovascular surgery. A procedure was performed to remove and close the aneurysm using a Dacron patch (Figure 2); coronary bypass grafting to the anterior descending artery using the left mammary artery was also performed without perioperative complications.
Figure 1. A: 2D-echocardiography (4-chamber apical view) where thin interventricular septum can be observed protruding toward the ventricle right (RV) forming an aneurysm (An). B: 2D color Doppler echocardiography (4-chamber apical view) shows the flow from the left ventricle (LV) toward the aneurysm at protosystole (blue), and a turbulent flow between the aneurysm and the right ventricle (RV) (color mosaic).
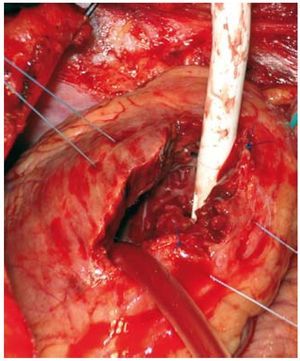
Figure 2.Intraoperative photograph showing a thin and necrotic interventricular septum, through the paraseptal left ventriculotomy. Note that the aspirator (white cylinder in the upper part of the photograph) is introduced through the interventricular shunt.
Rupture of the myocardial wall may occur in the context of acute infarction, an inflammatory process of the wall (eg, due to a septal abscess or complicated endocarditis on the aortic valve), or after a non-penetrating thoracic injury, but rarely in the scar of a chronic aneurysm.2 Scarring of the necrotic wall involves the replacement of myocardiocytes by fibrous tissue. This scar tends to be rigid and resistant, at the expense of losing elasticity, which favors dilatation in response to the increase in intracavitary pressures. In this case, the thin wall of the aneurysm had given way and opened toward another cardiac cavity years after the infarction, thus leading to an acquired interventricular shunt. We only know of one other case reported in the literature which described late rupture of the interventricular septum 2 months after an myocardial infarction. Since presentation was slow and progressive, it was possible to administer surgical treatment before the shunt was large enough to produce cardiac failure, shock, or death.