To the Editor,
Pulmonary artery aneurysms (PAAs) are an infrequent condition. Only a few, isolated cases have been reported in the literature worldwide and appropriate management remains unclear.
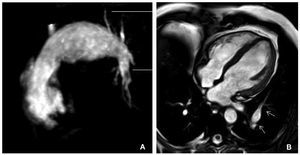
We present the case of a 48-year old patient, with a history of high blood pressure and tobacco use, who was admitted to our center for acute lateral myocardial infarction with subsequent coronary angioplasty of the circumflex artery. Interestingly, chest x-rays showed a sacular image at the level of the left edge second arch. Later, resonance angiography revealed aneurismatic dilatation measuring 53 mm in the pulmonary trunk and 23 mm in the left pulmonary artery (Figure). The patient was discharged at 5 days, opting for conservative management of the aneurysm due to the patient's clinical history (asymptomatic and with no published data to indicate high risk of rupture). At 9 months follow-up, the patient presented no clinical change and resonance angiography showed no difference in the anatomic characteristics of the aneurysm.
Figure 1. Resonance angiography of chest showing dilatation of the pulmonary artery trunk and its left branch. A: axial T1 slice. B: axial MPR reconstruction.
A review of the literature suggested the etiology of PAAs can be congenital or acquired. Congenital aneurysms are usually associated with cardiac malformations causing pulmonary hypertension, and persistent ductus arteriosus is the most frequent. Other causes include atrial and ventricular defects. Acquired causes can be idiopathic or associated with other processes, like infections (tuberculosis, syphilis), traumatisms, pulmonary valvular stenosis, or diseases affecting collagenous tissue.1,2 So, many PAAs coincide with a series of pathologic situations prior to development of the aneurysm: increased pulmonary flow, pulmonary hypertension, and/ or a coexisting pathologic process affecting the vascular wall. In the infrequent cases when PAA is not due to a functional or structural anomaly of the cardiovascular system, it is known as idiopathic PAA. Our patient corresponds to this clinical condition as we excluded causes and factors that predispose development of a PAA.
Clinical presentation of a PAA varies. It can be asymptomatic, being a chance finding in a chest x-ray as in our patient. In symptomatic patients, dyspnea, hemoptysis and chest pain are most frequent.1,3 Hemoptysis generally indicates instability of the aneurysm and indicates the need for surgical intervention.
Diagnosis by transesophageal echocardiography visualizes the trunk and rules out pulmonary hypertension or pulmonary valve infection and intracardiac shunt as secondary causes of the aneurysm.4,5 High resolution computerized tomography (CT) or resonance angiography permit evaluation of the trunk and its branches.5,6 Etiologies like syphilis, tuberculosis, and collagenopathies should also be considered.
Generally, the distinctive pathology of aortic aneurysms leads to a different management approach.4 Even if it is unclear, surgery is indicated (prosthesis, reconstruction with pericardium, or arteroplasty) if the risk of rupture exists.7 Patients with <60 mm aneurysms, low pulmonary pressure, absence of congenital or acquired significant right shunt or not associated with collagenopathies are considered at low risk and conservative management is preferred, as in our patient.1-3
To conclude, pulmonary aneurysms are extremely rare; they are frequently found in chest x-rays by chance. High resolution CT and resonance angiography are fundamental to diagnosis. Surgery is indicated in patients at risk of dissection or rupture.