Our objective was to assess the prognostic value of NT-proBNP in patients with asymptomatic moderate/severe aortic stenosis and to validate an adapted Monin score using natriuretic peptide levels in our setting.
MethodsProspective study of 237 patients with degenerative asymptomatic moderate/severe aortic stenosis. NT-proBNP was determined in all patients, who were then followed up clinically. The adapted Monin score was defined as follows: (peak velocity [m/s]×2)+(logn NT-proBNP×1.5)(+1.5 if woman). A clinical event was defined as surgery, hospital admission due to angina, heart failure or syncope, or death.
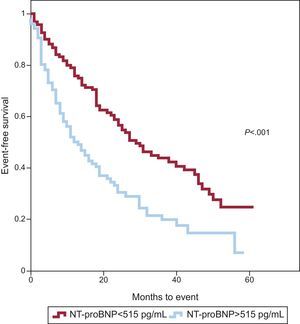
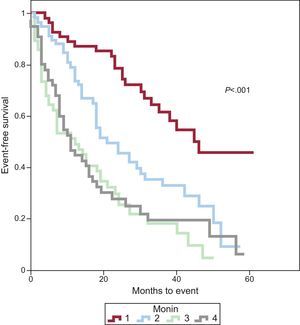
ResultsA total of 51% were women, and the mean age was 74 years. Mean (SD) echocardiographic values were as follows: peak velocity 4.14 (0.87) m/s; mean gradient, 43.2 (16.0) mmHg; aortic valve area, 0.87 (0.72) cm2, and aortic valve area index, 0.49 (0.14) cm2/m2. The median NT-pro-BNP value was 490.0 [198.0-1312.0] pg/mL. There were 153 events during follow-up (median 18 months). The optimum NT-proBNP cut-point was 515 pg/mL, giving event-free survival rates at 1 and 2 years of 93% and 57%, respectively, in patients with NT-proBNP <515 pg/mL compared with 50% and 31% in those with NT-proBNP >515 pg/mL. Patients were divided into quartiles based on the Monin score. Event-free survival at 1 and 2 years was 87% and 79% in the first quartile, compared with 45% and 28% in the fourth quartile, respectively.
ConclusionsNT-proBNP determination provides prognostic information in patients with asymptomatic moderate/severe aortic stenosis. The adapted Monin score is useful in our setting and allows a more precise prognosis than does the use of NT-proBNP alone.
Keywords
Aortic stenosis (AS) is the most common valve disease in Western countries, and its incidence is rising along with increases in life expectancy.1 Aortic valve replacement (AVR) is the treatment of choice in symptomatic patients with severe AS. Clinical practice guidelines recommend AVR for asymptomatic patients only if they have ventricular dysfunction or a pathological result on stress testing.2,3 However, several studies suggest that prognosis in asymptomatic patients with severe long-term AS is not as favorable as initially thought.4–8 Given that surgical mortality has decreased in recent years,9 several groups now advocate AVR for asymptomatic patients in an effort to improve prognosis.10–12 However, because of the high prevalence of AS in Spain, treating all patients with severe AS is neither organizationally nor economically feasible. Parameters are therefore needed to allow selection of asymptomatic patients at high risk of experiencing events over time. Such an approach would allow AVR surgery to be carried out in this group at the optimal time. Some of the parameters that have been described for risk stratification are difficult to obtain, or require serial echocardiographic studies or the performance of exercise tests.13–17
Recently, Monin et al.18 proposed a score that combines 3 easily obtainable parameters (maximum velocity [Vmax], B-type natriuretic peptide [BNP], and sex) and which identifies patients with moderate to severe AS and a high risk of events over time who would benefit from early AVR, despite being asymptomatic. The objectives of this study were to assess the role of N-terminal pro-B-type natriuretic peptide (NT-proBNP) in the prognostic assessment of asymptomatic patients with moderate to severe AS and to validate an adapted Monin score in our population.
METHODSThis was a single-center prospective study carried out between 2006 and 2011 in 237 consecutive patients with asymptomatic moderate or severe degenerative AS (Vmax>3.5 m/s and/or an aortic valve area <1.25cm2) and normal ventricular function (left ventricular ejection fraction >55%). Only patients with preserved resting ventricular function were included, as the study was designed to avoid mixing entities that are known to have a very different prognosis. Ventricular dysfunction occurred in 7% of patients as the disease progressed and was associated with clinical deterioration in all patients. We excluded patients with bicuspid aortic valve, given the low number of patients in our series, and those with other significant valve disease. All studies were performed using a General Electric Vivid 7 or 9 echocardiograph. The echocardiographic plane showing Vmax was used to calculate transvalvular gradients, and was typically the apical plane. The aortic valve area was calculated using the continuity equation and was indexed for body surface area. Blood analysis was performed with the patient at rest and fasting 15min before the echocardiogram. The samples were centrifuged for 15min, frozen, and subsequently analyzed by immunofluorescence. The score proposed by Monin et al.18 was defined as (Vmax [m/s]×2)+(logn BNP×1.5) (+1.5 if women); in line with common practice in our environment, the NT-proBNP logn was used instead of BNP. Patients were assessed clinically every 6 months; if patients failed to attend a visit, their hospital records were reviewed or a telephone interview was carried out to ascertain their vital and/or functional status. The primary endpoint was the occurrence of a composite event of hospitalization for angina, syncope or heart failure, AVR surgery, or death from any cause. The study was approved by the hospital ethics committee and all patients gave written informed consent before inclusion.
Statistical AnalysisContinuous variables were expressed as means (standard deviation) and categorical variables as numbers and percentages. To determine the best prognostic cut point for NT-proBNP, a bootstrap analysis was performed with a thousand replications, and the crossover point was confirmed by goodness of fit (multiple resampling provides confirmation that the cut-point obtained is the most appropriate). We determined the sensitivity, specificity, and area under the curve for the cut-point. The cumulative incidence of events was estimated using the Kaplan-Meier method. Univariate analysis was carried out using the Student t test or the Mann-Whitney U test. Categorical variables were analyzed with the chi-square test or Fisher's exact test as appropriate. A Cox multivariable regression was performed. A first model included the variables that make up the Monin score and a second was run with the same variables together with possible confounding variables. Results are expressed as hazard ratios (HR) and 95% confidence intervals (95%CI). In all analyses, a 2-sided P value of <.05 was considered significant. The statistical analysis was performed with SPSS 18.0 and R v. 2.11.1 (R Foundation for Statistical Computing).
RESULTSPatient baseline characteristics for the overall sample and for subgroups based on the occurrence of events are shown in Table 1. Of the overall sample, 51% were women, and the mean age was 74 years. When the European Society of Cardiology criteria was used,2 severe AS, defined by Vmax>4 m/s, was present in 57% of the sample (135 patients); when the criterion of aortic valve area <1cm2 was used, severe AS was present in 74% (176 patients). We followed up 97% of patients (231 patients) for a median of 18 [interquartile range, 7-31] months. Sixty-four percent of the sample (153 patients) showed the combined primary endpoint during follow-up, at a median of 12 [5-23] months after inclusion in the study. Some patients had more than 1 event during follow-up, in which case the patient was censored at the first event and only events of interest were recorded. There were 183 events in 153 patients: 110 patients required surgery, 44 were admitted for symptoms secondary to AS (without an indication for cardiac surgery), and 29 patients died (12% of patients): 14 from cardiac causes (heart failure or sudden death), 12 from extracardiac causes (neoplasms, respiratory infection, or stroke), and 3 after AVR surgery. Operative mortality was 2.9%. Six patients were lost to follow up. Valve surgery was indicated following a positive exercise test in 6% of the patients.
Baseline Characteristics of the Overall Sample and According to the Occurrence of Events in Asymptomatic Patients With Moderate or Severe Aortic Stenosis
| Total (n=237) | Patients without events (n=78) | Patients with events (n=153) | P | |
| Age, years | 74±9 | 75±10 | 73±9 | .15 |
| Women | 117 (51) | 36 (46) | 77 (50) | .55 |
| Hypertension | 175 (74) | 57 (73) | 113 (74) | .84 |
| Dyslipidemia | 147 (62) | 51 (65) | 93 (61) | .64 |
| Diabetes mellitus | 65 (27) | 23 (29) | 42 (27) | .74 |
| Baseline NT-proBNP, pg/mL | 490.0 [198.0-1312.0] | 325.5 [161.0-798.2] | 570.0 [250.0-1486.0] | .001 |
| Baseline logarithmic NT-proBNP | 6.3±1.3 | 6.0±1.3 | 6.5±1.3 | .003 |
| Creatinine, mg/dL | 1.2±0.9 | 1.2±0.7 | 1.2±0.7 | .94 |
| Maximum velocity, m/s | 4.14±0.87 | 3.84±0.92 | 4.23±0.82 | <.001 |
| Mean gradient, mmHg | 43.2±16.0 | 35.51±11.5 | 47.0±16.7 | <.001 |
| Maximum gradient, mmHg | 70.2±24.7 | 59.9±17.8 | 75.1±26.2 | <.001 |
| Aortic valve area, cm2 | 0.87±0.72 | 0.92±0.46 | 0.85±0.83 | .43 |
| Valve area index, cm2/m2 | 0.49±0.14 | 0.56±0.13 | 0.46±0.14 | <.001 |
| LV end-diastolic diameter, mm | 46.6±6.6 | 45.7±6.7 | 46.9±6.6 | .20 |
| LV end-systolic diameter, mm | 27.4±8.4 | 26.0±5.6 | 28.1±9.6 | .042 |
| LV mass, g | 232±83 | 216±66 | 239±90 | .027 |
| LV ejection fraction, % | 64±9 | 66±8 | 64±9 | .073 |
| Monin score | 18.5±3.1 | 17.3±2.9 | 19.1±3.0 | <.001 |
| NT-proBNP>515 pg/mL | 107 (47) | 28 (36) | 79 (52) | .018 |
LV, left ventricle; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
Data are expressed as No. (%), mean±standard deviation or median [interquartile range].
Bootstrapping showed that the best cut-point in this series was 515 pg/mL, which had a sensitivity of 52% and a specificity of 64% (area under the curve =0.628). A Kaplan-Meyer survival analysis was performed in patients with NT-proBNP values above and below the cut-point (Fig. 1). Event-free survival at 1 and 2 years of follow-up was 93% and 57% in patients with NT proBNP <515 pg/mL vs 50% and 31% in patients with values above the cut-point. Patients were divided into quartiles using the adapted Monin score, and Kaplan-Meier survival analysis was carried out for the different Monin quartiles (Fig. 2). Event-free survival at 1 and 2 years were, respectively, 87% and 79% in the first quartile (Monin score <16.7), 74% and 46% in the second quartile (score 16.7-18.3), 49% and 30% in the third quartile (score 18.3-20.3), and 45% and 28% in the fourth quartile (score >20.3).
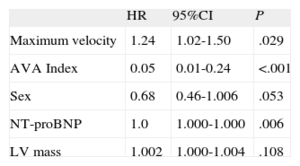
Table 2 shows the results of the multivariable analysis and indicates that Vmax, the aortic valve area index, and NT-proBNP were independently related to prognosis.
Risk Analysis Using Cox Regression for the Combined Endpoint: Model 1
| HR | 95%CI | P | |
| Maximum velocity | 1.24 | 1.02-1.50 | .029 |
| AVA Index | 0.05 | 0.01-0.24 | <.001 |
| Sex | 0.68 | 0.46-1.006 | .053 |
| NT-proBNP | 1.0 | 1.000-1.000 | .006 |
| LV mass | 1.002 | 1.000-1.004 | .108 |
95%CI, 95% confidence interval; AVA, aortic valve area; HR, hazard ratio; LV, left ventricle; NT-proBNP, N-terminal pro-B-type natriuretic peptide.
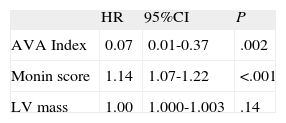
When the same model was applied with the adapted Monin score (which already includes sex, Vmax, and NT proBNP), it was independently related to prognosis, whether assessed quantitatively (Table 3) or by quartiles (Monin Q2 vs Q1: HR=2.23; 95%CI, 1.28 - 3.88; P=.004, Q3 vs Q1: HR=3.50; 95%CI, 1.95 - 6.24, P<.001; Q4 vs Q1: HR=3.10; 95%CI, 1.73 - 5.55; P<.001).
The NT-proBNP cut-point obtained (515 pg/mL) correctly discriminated patients with a follow-up event compared with those with moderate AS (P<.001). Monin's score accurately predicted events in both groups (Figs. 3 and 4) and had better predictive power than the use of NT-proBNP alone.
This study shows that asymptomatic patients with moderate to severe AS and NT-proBNP>515 pg/mL have a high risk of events during follow-up. The Monin score improves risk stratification and identifies a subgroup of patients (those in the first quartile) with good outcomes at 2 years. Currently, clinical practice guidelines recommend AVR only in asymptomatic AS patients with a class I indication when ventricular dysfunction is present or there is a positive exercise test.2,3 In other patients with asymptomatic AS, the recommendation is to continue clinical and echocardiographic follow-up every 6-12 months.2,3 Surgery should only be considered in special circumstances. However, not all patients with severe asymptomatic AS have a favorable prognosis, with event-free survival rates during follow-up ranging from 20% to over 50%.4,7,8,13 In the present series, the inclusion of patients with moderate AS may have had an impact on the results. Nevertheless, the rate of events in our series (64% of patients) is similar to that described by Monin et al.18 (59.6%), especially when taking into account that these authors included patients with AS and Vmax>3 m/s. The strategy of serial clinical and echocardiographic examinations can also lead to saturation in consulting rooms and imaging departments, and the marked decrease in operative mortality among patients with AS in recent years9 has prompted several groups to propose AVR in asymptomatic patients to improve their prognosis.10–12 Nevertheless, it is important to identify patients who would benefit from early AVR even when asymptomatic, as well as to identify patients who could undergo less intensive follow-up.
The exercise test is a useful and safe tool for risk stratification in patients with asymptomatic severe AS.19,20 However, although an abnormal result is an indication for AVR (symptoms on exercising, class I, level of evidence C, fall in blood pressure below baseline, IIa C),2 this test may not be feasible in all settings. In our series, a positive treadmill test was used as an indication for surgery in 6% of patients.
Determining BNP16,18,21 or its precursor (NT-proBNP)22 or a combination of both23–25 has demonstrated prognostic value in AS. A systematic review found no difference between BNP and NT-proBNP in the diagnosis of heart failure.26 NT-proBNP degrades more slowly and has a higher concentration in circulation and less biological variability than BNP.27 In our series, the best cut-point for NT-proBNP was 515 pg/mL, which is significantly higher than that found in other patient populations. However, those earlier studies did not specifically focus on patients with AS.28 The prognostic value of the crossover point can be considered moderate (area under the curve =0.628), although it is sufficient to independently detect a significant group of patients with asymptomatic AS who will experience events during follow-up.
In recent years, several parameters and scores have been described to predict which patients with AS will suffer an event during follow-up.13 In our series, Vmax was an independent marker of events during follow-up, as observed in previous studies.7,8,17,18,29 Rosenhek et al.7 showed that asymptomatic patients with very severe AS (Vmax>5.5 m/s) have a poor long-term prognosis, with only 44% and 4% of patients event-free at 1 and 4 years, respectively. Rapid progression of AS is also associated with a poorer prognosis.13,17 Both factors (Vmax>5.5 m/s, progression >0.3 m/s per year) are considered to be indications for AVR in patients with low surgical risk (class IIa).2 The aortic valve area index is also a marker of poor prognosis,21 a finding which was confirmed in our series. Other more complex echocardiographic parameters have been described, such as valve resistance,30 valve-arterial impedance,15,31 systolic longitudinal deformation of the left ventricle,15 left atrial volume index,15,29 tissue Doppler measurements, and aortic flow analysis.32 Unlike other studies,33,34 in our series, ventricular mass was independently associated with prognosis.
In view of the above, in recent years interest has increased in new algorithms that could provide a more precise prognosis in asymptomatic severe AS.15,18,34,14 However, some of these algorithms involve the use of complex parameters.15
The Monin et al. score18 combines 3 easily measurable parameters (Vmax, BNP, and sex). This is the first study to validate the usefulness of the Monin score in asymptomatic AS patients in our setting. In this series, we observed event-free survival rates of 87% and 79% at 1 and 2 years, respectively, in the first quartile, compared with less than 49% and 30% in the third and fourth quartiles. This score therefore provides a better prognostic classification between groups of high (quartiles 3 and 4) and low risk (quartile 1) than the NT-proBNP value alone. A Monin score of <16.7 identifies asymptomatic patients with good prognosis in the medium term. Patients with a Monin score of >18.3 (third and fourth quartiles) should be more closely followed up and an exercise test should be considered for better risk stratification. If surgical risk is low, early AVR surgery could even be considered if surgical risk is low, as half of these patients will have symptoms within 1 year.
LimitationsThe follow-up period in this study (median 18 months) was not very long, although we believe it was sufficient to meet the initial study objective. The inclusion of patients with moderate AS (Vmax>3.5 m/s) may have had an impact on the results. However, the number of events in our series is similar to that described in the study by Monin et al. (which included patients with AD with Vmax>3 m/s).
CONCLUSIONSNT-proBNP can stratify the prognosis of patients with moderate or severe AS before symptom onset. The optimal cut point was 515 pg/mL. The score described by Monin et al. can be adapted to our population and improves the prognostic value of NT-proBNP alone.
CONFLICTS OF INTERESTNone declared.