Keywords
INTRODUCTION
ST-segment elevation acute myocardial infarction (STEMI) is a common condition whose treatment has changed considerably over the last years.1 Currently, the best treatment for STEMI is considered to be a primary percutaneous coronary intervention (PCI),2 providing that a series of requisites are met. One of these is that the time from the arrival of the patient to the emergency room to restoration of flow in the obstructed artery is <90 minutes.3,4 Nonetheless, recent reports have shown that this maximum delay time is met only to a certain extent in the patients treated with primary PCIs,5 and that longer treatment delays can adversely affect the patients' prognosis, regardless of their overall risk or the total ischemia time (TT).6 The delay time to reperfusion can vary in certain patient subgroups; for example, the demand for prompt reperfusion is much greater in younger patients with an anterior acute myocardial infarction (AMI) than in other groups.7
Several strategies have been designed to shorten the reperfusion delay time, and their efficacy has been proven in various hospitals in the United States.8-11 This effort has led to the creation of a specific working group within the American College of Cardiology (ACC), called the D2B (door-to-balloon) Alliance. In contrast to the situation in the United States and many other countries within and outside the European Union, the ambulance service in Spain provides in situ diagnosis of AMI and selection of patients for primary angioplasty. Hence, the improvement in reperfusion delay time in our setting may be even better12,13 than that achieved when the D2B recommendations are applied, providing the remaining recommended measures are also used.
The aim of this study is to report the delays encountered in performing primary angioplasty in our setting, determine the factors affecting these delays, and describe the influence on the reperfusion delay time of applying a treatment protocol in a contemporary series of unselected patients.
METHODS
The treatment of choice for STEMI in our hospital is primary angioplasty. Currently, we have a primary PCI program staffed by 5 interventional radiologists and the nursing staff of the catheterization laboratory. The emergency alert is implemented at 15:00 because no catheterization procedures are scheduled for the afternoon.
The public health area in which this study was developed is a triangular-shaped area in the province of Madrid. The hospital is not centrally located, but instead is found at one of the vertices of the triangle. The total population of the area is 635 495 inhabitants, distributed in 13 public health districts, most of which are large urban centers, including the northeast area of Madrid. The only district with less than 10 000 inhabitants is the one farthest from the hospital, at a distance of 73 km. Most of the public health districts are connected to the hospital by a network of highways.
The emergency transport service provides advanced warning to the cardiologist on duty in all cases of AMI of less than 12 hours' duration and in cases requiring rescue angioplasty. The cardiologist then activates the alert, providing the patient is younger than age 90 and is not in cardiogenic shock, and the angiography team notifies the emergency room to transport the patient directly to the catheterization laboratory upon arrival.
A total of 459 patients with STEMI were admitted to our hospital from January 2005 to October 2007, and primary or rescue PCIs were performed in 389 (84.7%). The clinical and angiographic data of these patients were prospectively collected without exception, and stored in a dedicated database. The study included all patients with STEMI, regardless of the time since onset, in whom an urgent PCI was considered indicated and was performed.
All patients underwent coronary angiography; the preferred access was the right radial artery, but other approaches were used when radial access was not feasible or the device size required a different route. All patients were pretreated with 300 mg of acetylsalicylic acid and 600 mg of clopidogrel orally when there were no contraindications, as well as an initial heparin sodium dose of 5000 IU, plus 1000 IU every 30 min for the duration of the procedure. A thrombus aspiration device is routinely used in our catheterization laboratory, except in selected cases that are treated at the discretion of the interventional radiologist. In addition, glycoprotein IIb/IIIa-inhibitor is routinely administered (except when contraindicated); during the study this was mainly abciximab. Whenever possible, a conventional stent was implanted, and in special situations, the choice of the device was based on the operator's criteria.
Following the procedure, a lengthy recording was performed to measure the tissue perfusion parameters. All recordings were stored in DICOM format, and an interventional cardiologist who was not involved in the study reviewed the images to quantify the angiographic variables at different time points during the angioplasty procedure. The perfusion parameters were graded according to the recommendations of the TIMI14 group. The initial epicardial vessel flow (TIMI flow) and the mean door-to-balloon time following thrombus aspiration and at completion of the procedure were analyzed.
The following time points were recorded: the time of pain onset, the time the emergency system (SUMMA112; Servicio de Urgencia Médica de Madrid, Madrid Emergency Medical Service) was alerted, the time the ambulance arrived at the patient's home, the time the patient reached the hospital emergency department, the start of the interventional procedure, and the time the angioplasty guidewire crossed the lesion. In addition, the delay incurred with the use of the aspiration device was recorded. The time points were obtained from the SUMMA event registry, and the time of arrival at the hospital was obtained from the patient's administrative information. The times in the catheterization laboratory were annotated by the attending cardiologist.
The following clinical data were obtained during hospitalization: creatinine kinase and troponin I values at 6 hours and the maximum levels; left ventricular ejection fraction (LVEF) prior to admission, and adverse events (death, reinfarction, and need for revascularization of the AMI culprit lesion). Clinical follow-up assessing the same adverse events was performed in all patients by scheduled visit or telephone interview at 1 and 12 months following the procedure. A new AMI was established on troponin I re-elevation plus at least one of the following criteria: symptoms of ischemia, appearance of new pathological Q-waves, ECG changes indicative of ischemia (ST-segment decrease or elevation), or percutaneous coronary reintervention of the lesion causing the prior AMI.
In April 2007, a multidisciplinary working group was created, which included clinical cardiologists, interventional radiologists, emergency room specialists, and nursing staff from the emergency department and catheterization laboratory. In a second stage, SUMMA staff were incorporated in this group of professionals, with the aim of investigating and discussing the delays to revascularization, and improving the care provided to patients with STEMI. The aim of the working group was to reduce the door-to-balloon time to less than 60 minutes. The specific measures adopted to date consist of the following: monthly meetings to present and discuss the results obtained up to that time; preparation of a written consensus protocol, approved by the area management in charge of care for STEMI patients undergoing a primary PCI, and including advanced warning and activation of the alert from the moment the call from the SUMMA is received (this analysis is not a part of the aim of this study); and free access to the AMI database for all members of the team. All these measures are under the direction of the senior cardiologist in charge of the hospital's catheterization laboratory. In the present report, the times obtained after the first meeting of this group were compared with the times obtained prior to this meeting.
Statistical Analysis
The Kolmogorov-Smirnov goodness-of-fit test was used to assess the normality of distribution. Variables evaluating the delay times were compared using the Student t test for independent data and the Mann-Whitney rank sum test when the hypothesis of normality was rejected. Kruskal-Wallis analysis of variance was used to compare the times between more than 2 groups. The tables list the medians of the original values and occasionally, the medians of the differences between groups with the 95% confidence interval (95% CI). To compare percentages, we applied the Pearson c2 test and the continuity-corrected c2 test. Significance was set at a 2-tailed P value of <.05. A multiple logistic regression analysis model was performed to measure the simultaneous and independent influence of the patients' risk factors for death, including all the variables related to death at 30 days in the univariate analysis and adjusted for the fact of advanced warning or not. The odds ratio (OR) and 95% CI were calculated and variables with a P value of <.1 were included. Data analysis was carried out with SPSS, version 14.0.
RESULTS
Over the period studied, 389 PCIs were performed for STEMI in our center, including 361 primary PCIs and 28 rescue procedures. The demographic and angiographic characteristics of the population studied are shown in Tables 1 and 2.
The median TT (time from symptom onset to passage of the guidewire) was 235 minutes (25th-75th percentiles, 170-335). The median door-to-balloon time was 79 minutes (53-104). The median time spent using the thrombus aspiration device was 8 minutes.
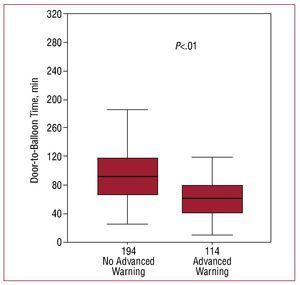
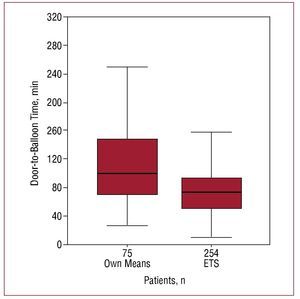
The door-to-balloon time was significantly lower in cases in which the cardiologist on duty received advanced warning and the catheterization laboratory was alerted about the incoming patient before emergency room arrival; there was a 30-minute decrease in this group with respect to the remaining patients (Figure 1). This difference was particularly marked in patients who came to the hospital outside normal working hours (Table 3). The comparison between patients who arrived with advanced warning (36% of the total) and those who did not (64%), showed that the two populations mainly differed in the degree of ST segment deviation (advanced warning was more frequent at higher deviations) and in patient age (higher percentage of warnings in younger patients), whereas the remaining characteristics were similar. The longest door-to-balloon time, however, was observed in patients who arrived at the emergency room by their own means, which comprised 24.5% of the total (patients who had not yet been diagnosed) (Figure 2). A comparison of the characteristics of patients who came by their own means with those of the remaining patients showed a significant difference only in the fact of having angina in the previous 24 hours: fewer patients had this factor than those who came to the emergency room by ambulance (20.7% vs 31%, respectively; P=.04).
Figure 1. Time to revascularization according to whether advanced warning had been given
Figure 2. Time to revascularization according to the means of transport to the emergency room. ETS indicates emergency transport service. The number of patients in each category is indicated in each column.
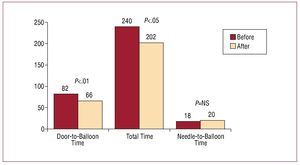
The delays occurring after implementation of the working group meetings (in a total of 83 patients) were analyzed and compared with those occurring before these meetings (306 patients). A significant improvement was seen only with the start of the discussions and presentation of the actual delays to the working group. The TT, door-to-balloon time, and time from the start of PCI to passage of the angiography guidewire before and after the meetings are shown in Figure 3. The TT and door-to-balloon time are seen to decrease significantly, mainly because of the reduction in the time interval from the patient's arrival at the emergency room to the start of the primary PCI procedure.
Figure 3. Comparison of the median times before and after establishing the working group to shorten the revascularization delay time. NS indicates non-significant.
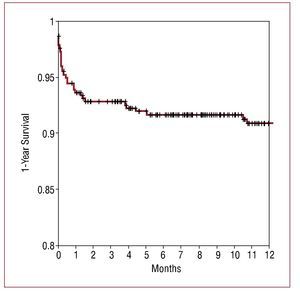
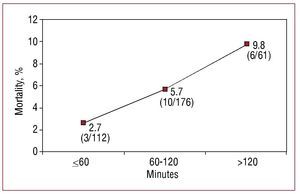
The mean total duration of follow-up was 15.11 months, with in-hospital follow-up rates of 100% and 99% at 1 month. A total of 226 patients reached 1 year of follow-up, and 99% completed the follow-up period. Total 1-year mortality was 8.5%, and 1-month mortality was 6.2% (24 patients, among whom 20 died before hospital discharge). Among the 33 deaths, 9 were due to an extracardiac cause and the remaining to a cardiac cause, mainly cardiogenic shock. The 1-year survival curve is shown in Figure 4. The recurrence rate of AMI affecting the same territory was 1%, in all cases with ST segment elevation. The need to revascularize the same lesion was 3.9%. In patients who required revascularization before 1 month, the event was related to recurrent AMI, whereas in 90% of those requiring revascularization later, the cause was clinical restenosis. Patients with a poorer evolution presented a significantly longer door-to-balloon time: nonsurvivors had a mean door-to-balloon time of 137.6 minutes, compared to 89.7 minutes for the remaining patients (P<.01). After dividing the time interval into segments (terciles), we found a significant, gradual increase (P<.05) in 30-day mortality the longer the door-to-balloon time (Figure 5). In the multivariate analysis, the variables independently related to higher mortality were final TIMI flow 0 or 1 and patient age. A door-to-balloon time >120 minutes was associated with higher 30-day mortality in the univariate analysis and with a trend to higher mortality in the multivariate analysis (Table 4). Severe ventricular dysfunction was also related to higher mortality, but this factor was not included in the multivariate analysis because it is a measurement taken following catheterization and was not available in 28% of those who died (because death occurred before an echocardiogram could be performed). Comparison of the characteristics of patients who presented a door-to-balloon time above or below 120 minutes (Table 5) revealed a higher percentage of patients with diabetes, women, and older patients among those with a longer delay, in addition to patients who came to the emergency room by their own means and those for whom advanced warning was not given.
Figure 4. Total survival at 1-year of follow-up (Kaplan-Meier).
Figure 5. Thirty-day mortality as related to the door-to-balloon time. Data on the graph indicate the total number of patients who died in each group and the percentage calculated using these data.
DISCUSSION
Current recommendations for the treatment of STEMI include the condition that the door-to-balloon time in a primary PCI should not exceed 90 minutes.3 Nonetheless, this requirement is not met in many patients who receive this treatment. A reperfusion delay in patients with STEMI is associated with a less favorable evolution, both in those treated with thrombolysis and those with a PCI.15-18
The mean delay time in performing a primary PCI in our hospital is within the specifications of current recommendations, but we should point out that even in a hospital with a primary PCI program running 24 hours a day, the recommended door-to-balloon limit of 90 minutes was exceeded in 38% of patients, and was longer than 120 minutes in 18.4% of patients. Our results are comparable to those reported by Carrillo et al13 in a hospital with a primary PCI program that had been running for several years: the door-to-balloon time was 70 minutes (46.8-105.5 minutes), but the TT was much shorter, possibly because of geographic differences regarding the distance and access routes to the hospital.
In the present study a relationship was found between the door-to-balloon time and 30-day mortality, with significantly higher mortality in patients experiencing a delay greater than 120 minutes, and a clear trend to higher mortality in these patients in the multivariate analysis. In keeping with the study by McNamara et al,6 the TT was not associated with mortality in our patients, possibly because it is difficult to reliably record this parameter, which depends substantially on the subjective estimate of the patient and does not necessarily represent the true time during which the artery is occluded.
Because of the importance of the delay to reperfusion on the prognosis of patients with STEMI, a recent investigation has focused on a series of measures to shorten this interval.11 In fact, a specific working group for this purpose created within the ACC and known as the D2B Alliance, has set down a series of recommendations to this end. Consistent with the results of previous reports,19,21 we found that advanced warning by the emergency transport service, with direct transfer of the patient to the catheterization laboratory in many cases, resulted in a significant reduction of approximately 30 min in the time to revascularization. In this regard, we mention 2 recent studies performed outside of Spain. The first, from a group in Ontario,20 reported that in patients diagnosed in the ambulance by paramedics who subsequently activated the alert in the catheterization laboratory, the door-to-balloon time was significantly lower than that of patients referred from the emergency room for a primary PCI (69 vs 123 minutes, respectively). In another trial by Carstensen et al,20 a reduction of 95 minutes in the door-to-balloon time was seen when the diagnosis was made by the ambulance staff in situ and more than 90% of patients were directly transported to the catheterization laboratory of a referral center.
We observed a significant improvement in the door-to-balloon time, with a median decrease of 90 minutes, related to discussion of the results and close collaboration with the emergency personnel. Our objective is to achieve revascularization in less than 90 minutes in all our patients, but we believe that a greater reduction, to 60 minutes, would provide additional benefits and is an objective within the possibilities of a tertiary hospital in our country. By adopting a series of simple, feasible measures (being aware of and periodically analyzing our delay times, discussion among all the professionals involved, promoting advanced warning by the emergency transport service, and presence of a cardiologist on 24-hours' centralized call) delays to reperfusion can be substantially reduced, and possibly, the evolution of our patients improved.
Limitations
This study was carried out at a single center with a relatively small number of patients, hence the results cannot be extrapolated to the situation in all the health areas within Spain. In addition, although the data collection was performed prospectively, the analysis of variables with an impact on the result was retrospective and the study design was not randomized. It would be interesting to extend the study to a larger number of patients in other health areas with a primary PCI program and determine the impact of applying a predefined protocol.
CONCLUSIONS
This report presents the true values related to delays in revascularization occurring in primary angioplasty procedures in our setting, which may serve as a reference for future studies. We underline the importance of advanced warning by the emergency transport system for reducing the door-to-balloon time and report the influence of this factor on the evolution of our patients at short-term and mid-term.
ABBREVIATIONS
PCI: percutaneous coronary intervention
STEMI: ST-segment elevation acute myocardial infarction
TT: total ischemia time
SEE ARTICLESON PAGES 1-6
Correspondence: Dr J. Goicolea Ruigómez.
Unidad de Hemodinámica. Hospital Universitario Puerta de Hierro. San Martín de Porres, 4. 28035 Madrid. España.
E-mail: j_goicolea@hotmail.com
Received March 8, 2008.
Accepted for publication July 18, 2008.