At a conference a few years ago, Professor Braunwald, spoke about the new challenges cardiology would have to face in the 21st century. He mentioned that atrial fibrillation would be one of these challenges, and he classified it as an epidemic, given the extremely high and increasing figures for its incidence and prevalence.1 Yet another article, recently published in a scientifically renowned journal, referred to the growing incidence of this atrial arrhythmia, and again compared it to an epidemic.2
Throughout this editorial we aim to update the evidence on the growing epidemiology of atrial fibrillation. We shall analyze the data and comment on which data we use for the calculations of the incidence and prevalence of atrial fibrillation in the general population. We shall also provide data concerning the varying epidemiology depending on age, sex, race, and social and economic status, as well as compare the data from studies undertaken in populations from North America and from Europe. Finally, we shall make a few comments on these data and analyze the underlying reality of the growth in this arrhythmia.
Nobody nowadays doubts that atrial fibrillation is the most frequent sustained arrhythmia in the human heart, nor that it is the most clinically diagnosed arrhythmia, in both outpatients and hospitalized patients. Its importance as a factor determining mortality, which it increases by 2-fold, and its relevance as a causative factor of stroke, the risk for which it increases by 5-fold, are incontrovertible and concordant in the various publications.3-8
Nevertheless, we should recognize that many of these epidemiologic studies were carried out in populations with permanent or non-transitory atrial fibrillation. Little information is available about death and disease in persons with this atrial arrhythmia in its paroxysmal form, in young adults and in persons without structural heart disease. Epidemiologic studies are also needed in this population, too.
In recent years we have seen the adoption of the clinical classification of atrial fibrillation in three forms: paroxysmal, persistent, and permanent.9 Paroxysmal atrial fibrillation is considered to be that which has a duration of fewer than 7 days, persistent atrial fibrillation that which lasts more than 7 days and fewer than 6-12 months, and permanent atrial fibrillation that which lasts indefinitely. This classification arose in order to cover a new therapeutic weapon, the system of implantable atrial defibrillation. Patients with persistent atrial fibrillation were ideal candidates for this treatment option. Unfortunately, the automatic implantable defibrillator for these atrial arrhythmias failed early on, because of the documented risk of causing ventricular arrhythmias with the electric shock. Nevertheless, the clinical classification survived and has become established, given that it adjusts to the natural history of the disease, the symptoms of the patients, the estimation of its risk and the indication for and results of alternative treatment options, such as cardioversion or catheter ablation.
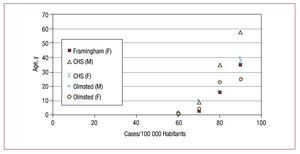
The original studies on the epidemiology of atrial fibrillation, however, did not use this modern classification. Furthermore, an important point to bear in mind in the larger studies of the epidemiology of fibrillation is that they were done on what their authors called non-transient atrial fibrillation. That is, the Framingham, West of Australia, Mayo Clinic, and Olmsted County studies were all based on data concerning chronic or permanent atrial fibrillation, as we would now call it. Another important point is that the known epidemiology of this arrhythmia is based on a population older than 60 years of age, and it is taken for granted that it is a rare clinical entity in young or middle-aged persons3-8 (Figure 1).
Figure 1. The incidence given in different epidemiologic studies in the United States. Note the absence of data for persons younger than 60 years of age and the higher incidence with increasing age and in men (modified from Misayaka et al10). CHS indicates Cardiovascular Health Study; F, female; M, male.
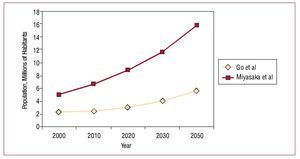
Go et al5 estimated that 3 million persons in the United States would have atrial fibrillation in 2020, and that this figure would increase to 5.6 million in 2050 (Figure 2). Another, more recent epidemiologic study, that of Misayaka et al,10 estimated that the figures provided by Go et al5 were below the true prevalence and incidence of the arrhythmia and that nearly 16 million persons in the United States would have fibrillation in 2050. This very surprising discrepancy in the estimated figures can be explained by the inclusion in the data base of Misayaka et al10 of patients with paroxysmal atrial fibrillation and silent or asymptomatic fibrillation. Both studies take into account not only the growth of the elderly population, but also the increase in the prevalence of the arrhythmia that is being seen over recent years (Figure 2).
Figure 2. Growth in the incidence of atrial fibrillation in the population of the United States. Comparison of the data of Go et al5 and Miyasaka et al. 10.
The study showing the greatest prevalence of atrial fibrillation in the elderly population was the Cardiovascular Health Study, which found a prevalence of 22% in the male population above the age of 80 years. This prevalence was much higher than that found in the other epidemiologic studies mentioned (Figure 1).
Expressing the risk of having this arrhythmia in another way and applying the data from the Framingham study on atrial fibrillation in the adult population, it is calculated that 1 out of every 4 persons older than 40 years will have atrial fibrillation during their lifetime. A European study published in 2006, the Rotterdam study, found the risk of having atrial fibrillation in persons aged 55 years or older was 23.8% for men and 22.2% for women.11 This is not the first study (it was also seen in the Framingham study) to show a small increase in the prevalence and incidence of arrhythmia in men as compared with women.4,8 Misayaka et al10 and the 2 most recent European studies all confirm this finding of a greater prevalence and incidence in men. The differences, though, become less with age and, in relative terms, are the same for all persons over the age of 75 years, given the greater survival of women. No discordance exists about this in the various relevant publications.8,10
Nowadays, we also have data correlating the social and economic status of patients with the risk for this arrhythmia.12 The prevalence of arrhythmia found in the Scottish study was 8.4/1000, with a clear variation according to age: 0.3/1000 in persons younger than 45 years and 70.3/1000 in persons aged 85 years or older. As concerns the social and economic factor, those persons with a lower income also had a lower incidence of fibrillation. However, consideration must be given here to possible confounding factors, such as the lower detection rate of arrhythmia due to poor health care.
As regards the prevalence of atrial fibrillation in Spain, the 1999 CARDIOTENS study, which had a cross-sectional design and was carried out in a primary care and specialized setting, showed an overall prevalence of atrial fibrillation of 4.8%, which rose with each decade of life by 1% in those younger than 50 years of age and reached 11.1% in persons aged 80 years.13 Another epidemiologic study, carried out in a population comprising 7108 persons aged 60 years or over who attended their primary health care facilities, is the PREV-ICTUS study, published in 2007.14 This study found atrial fibrillation on the electrocardiogram of 605 persons, giving a prevalence of 8.5%. This figure rose linearly from 4.5% in persons aged between 60 and 64 years up to 16.5% in persons aged over 85 years. The prevalence was slightly higher in men than in women (P=.036).14 These data, obtained from a census of 9 million inhabitants aged 60 years or over, suggest that between 720 000 and 840 000 persons currently have this arrhythmia in Spain.14 A study that undertook a retrospective analysis of the prevalence of atrial fibrillation in an urban population of 13 945 patients seen at primary care centers revealed a general prevalence of 2.52% in persons aged 40 years or older.15 Another recent study of the prevalence of atrial fibrillation, carried out with a cross-sectional design on a population base of persons seen at the outpatient clinic of specialist cardiologists, found a general prevalence 11.5%.16 This figure contrasts with the previous figure, as it is clearly higher, probably due to the bias derived from the selection of the patients attending a specialist.
The design of the registries in Spain does not enable us to determine the incidence of atrial fibrillation, though the calculations of prevalence that have been reported coincide with the figures of European and American studies.
With regard to the general Spanish population, if we extrapolate the incidence given by Misayaka et al10 to Spain, by the year 2050 there will be about 2 million persons with atrial fibrillation.
The ethnic aspect also shows a few variations in American reports concerning the incidence of atrial fibrillation. The black race appears less predisposed to having fibrillation than the Caucasian race, though the prevalence in the general population is only a little lower.5 The prevalence of this arrhythmia in black persons with heart failure, though, is half that seen in Caucasians. Furthermore, this difference is not reduced after adjusting for the various risk factors associated with atrial fibrillation.17
A summary of the interpretation of all these epidemiologic data shows that the incidence of this arrhythmia is on the rise, for several different reasons. The first of these reasons is that the population of the developed world is not only increasing, it is also becoming older due to the lengthening of the average life expectancy of its inhabitants. But additionally, and this factor probably assumes more importance than the former concerning the growth of this arrhythmia, is that greater interest is being shown in its diagnosis. This arrhythmia may have an overwhelming proportion in an early, subclinical phase. It is now thought that atrial fibrillation is a chronic and progressive condition that in most persons starts at middle or early ages, with randomly distributed crises and with grouping of episodes, initially short but whose distribution over time and duration intensify until they progress to a permanent arrhythmia.18
If what we already know about the incidence and prevalence of atrial fibrillation is noteworthy, these figures are even thought to be below the true figures, bearing in mind the number of middle-aged persons with short-lived crises of palpitations that they consider unimportant and not, therefore, worthy of bringing to the attention of their physician. These persons are just diagnosed with paroxysmal atrial fibrillation, when their arrhythmias in fact become more frequent and of a longer duration, and they are eventually correctly diagnosed at an emergency medical center by means of an electrocardiogram.18 This subclinical phase of arrhythmia is probably more important in order to be able to take therapeutic measures before the atrial remodeling is produced.
We should also take into account the importance of silent or asymptomatic atrial fibrillation. A study in patients receiving azimilide or placebo for atrial fibrillation found that 17% of the placebo group, composed of 489 persons, had asymptomatic atrial fibrillation.19 Another study of patients with atrial arrhythmias who received a pacemaker with a Holter function included found that 38% had asymptomatic relapses of atrial fibrillation.20
Thus, we see that the population is growing and aging, and that we are now paying more attention to the diagnosis of this arrhythmia. Moreover, we are now recognizing early stages of atrial fibrillation, at early and middle ages, at which the prevalence of this arrhythmia was previously unknown. We now recognize that at these ages there is much atrial fibrillation that is clinically silent and not, therefore, quantifiable in epidemiologic data.
The increase in risk factors determining the onset and development of atrial fibrillation is certainly playing a role in the growth in the incidence of this arrhythmia. When reviewing its etiology, it is important to note that the appearance of atrial fibrillation is directly related with the structural heart diseases that cause increased intra-atrial pressure. This is the case with mitral valve disease, heart failure of any origin, arterial and pulmonary hypertension, cardiomyopathies or ischemic heart disease in its acute or chronic phases. Cardiac tumors, pericardial disorders, congenital heart disease (whether or not corrected previously) and cardiac surgery are all potential causes of atrial fibrillation.
Other systemic diseases, such as hyperthyroidism, are linked to the appearance of arrhythmias during their clinical course. Obesity, diabetes mellitus and the metabolic syndrome have all recently been associated with the onset of atrial fibrillation, and these diseases are all growing in the developed world.21 An inverse process relates to the incidence of rheumatic valve disease, which has fallen and almost ceased to exist in the developed countries.
Of all the etiological factors, though, heart failure has an enormous epidemiologic burden in the elderly, and its growth parallels that of the aging of the population (Table).
Idiopathic atrial fibrillation, often called lone atrial fibrillation, is an etiologic variant in recession, if one considers that it is an atrial arrhythmia of unknown etiology, not related with structural heart disease or hypertension. This use of the word idiopathic implies a diagnosis by exclusion of any known cause or etiology. Consequently, far fewer persons now have it, as its association is known, for example, with sporting activity,22 and cases with a family incidence are associated with a genetic determination.23 Genetics, a field in which further findings will very likely soon be revealed, is helping us in our understanding of this arrhythmia.
Nevertheless, it is necessary to insist that medical recognition of atrial fibrillation in its early stages, during its phase of paroxysmal fibrillation, is the factor having the greatest weight regarding the very great increase in the incidence of this arrhythmia that we are now witnessing, above its true increase.
The reader is reminded that catheter ablation of arrhythmogenic foci of the pulmonary veins is a therapeutic technique that was initially used in paroxysmal focal forms of atrial fibrillation. Given this, the age in one of the cohorts treated with this procedure was 55 (10) years24 and in the cohort of another series it was 51 (12) years.25
If we consider electric cardioversion as a therapeutic procedure applicable to this atrial arrhythmia in its persistent phase, the mean age in 2 large series recently published was 68 (8) years in the European series26 and 69 (7) years in the American series.27 A recently reported series from Spain found the mean age of the candidate population for electric cardioversion to be similar, although slightly less than the mean seen in foreign series, 63 (11) years.28
Thee data all give us an idea of how atrial fibrillation presents clinically before the age of 70 years, especially in its paroxysmal and persistent forms.
The Scottish study mentioned earlier12 refers to the impact that this increasing epidemiology has on the outpatient clinics of cardiology services. Its authors point out that the number of outpatient visits for atrial fibrillation is the same as the number for ischemic heart disease, and that these figures are only surpassed by the number of visits due to heart failure in the elderly population, which almost doubles the numbers of each of the other.
The Royal Academy of the Spanish Language provides the following definition of epidemic (translated): "disease that propagates for some time in a country and that simultaneously attacks a large number of persons." Thus, this definition of The Royal Academy of the Spanish Language gives a concept of epidemic having a clear implication of limits in time and space, which are lacking for atrial fibrillation. The sole facet of this arrhythmia that would equate it to an epidemic is the fact that it "simultaneously attacks a large number of persons."
Faced with these epidemiologic data, which prove alarming in their proportions and repercussions on health care and expense, it is of course necessary to be aware of the need to continue investigating the etiology and pathophysiology of atrial fibrillation in order to be able to develop new preventive and therapeutic measures.
Correspondence: Dra. C. Moro.
Unidad de Arritmias. Hospital Ramón y Cajal.
Ctra. de Colmenar, s/n. 28034 Madrid. España.