To the Editor
The incidence rate of acute coronary syndrome during pregnancy ranges between 1.5 and 3.3 cases per 100 000 pregnancies.1 The principal risk factors are advanced maternal age, classical cardiovascular risk factors, and severe anaemia; the maternal mortality rate is very high, and the aethiopathogeny is not the same as that observed without pregnancy, so thrombus and coronary dissection are more frequent.2 Primary angioplasty is the treatment of choice for acute myocardial infarction during pregnancy, since it is the safest option for the woman and the foetus.3
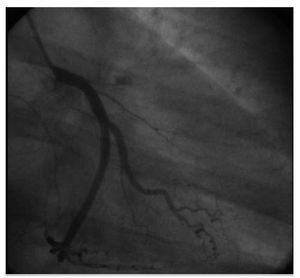
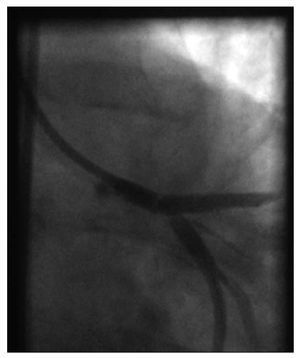
We present the case of a 39-year-old first-time mother, in the sixth week of gestation and a 1 pack/day smoker with no other cardiovascular risk factors. She experienced centre thoracic pressure 15 minutes in duration, and the electrocardiogram showed a rise in the ST segment in anterolateral distributions; she was admitted to the cardiac unit and the decision was made to perform emergency coronariography with abdominopelvic protection. We observed thrombotic-type ostial occlusion of the anterior descending artery, but coronary dissection was not observed from the angiogram (Figure 1). At the beginning of the procedure, loading doses of clopidogrel, Aspirin, and sodium heparin were administered and we proceeded to implant a conventional stent in the occluded zone. During the procedure, the patient experienced thoracic pain once again, and we witnessed the appearance of a thrombus in the proximal region of the circumflex artery and the left coronary trunk (Figure 2). In response, we administered abciximab and intracoronary adenosine and dilated the left coronary trunk, the anterior descending artery and the circumflex artery with the kissing balloon technique. Subsequent evolution was good. The echocardiogram showed hypokinesia in the apical segments of the lateral, anterior and inferior faces, with an ejection fraction at the lower limit of the normal range, and the electrocardiogram showed anteroseptal necrosis. Aspirin was prescribed for an indefinite period, in addition to clopidogrel, and it was later decided to maintain clopidogrel during 12 months. The pregnancy progressed normally, and in week 41 of gestation, the patient was admitted to the maternity hospital following a premature rupture of the amniotic sac, and a caesarean was indicated. Platelet concentrate was administered before the procedure, and spinal anaesthesia was used. A baby girl was born, at term and with adequate weight for her gestational age. She presented a permeable oval foramen of 0.2 mm, restrictive interventricular muscle communication and moderate mitral insufficiency, which rated as mild in a check-up 2 months later. The mother made favourable progress with no episodes of angina, signs of heart failure or anaemia, and 24 hours later resumed treatment with aspirin and clopidogrel.
Figure 1.Occlusion in the anterior descending artery.
Figure 2.Thrombus in the left coronary trunk and the circumflex artery.
We feel it important to report our experience given the rareness of the case and the scant experience with the use of antiaggregants during pregnancy. With regard to the use of clopidogrel, the experience has been reported in a small number of human cases with no description of apparent complications4; as for glycoprotein IIb/IIIa inhibitors, some cases have been reported with abciximab5 and only one with tirofiban,6 and none took place during the first trimester of pregnancy. In that case, despite the implantation of an uncovered stent, prolonged clopidogrel treatment was chosen due to its location and the presence of the intracoronary thrombus, whereas in the abciximab case the decision to use the drug was made based on the appearance of the thrombus during the procedure. We can neither establish nor discard a relationship between platelet antiaggregant use, together with the possible effects of radiation during the organogenesis period, and the cardiac malformations in the newborn. It must be stated that these anomalies are relatively frequent and have a benign prognosis,7 but this possible relationship should be considered. On the other hand, we found ourselves in a situation in which we had to perform a caesarean in a patient who was taking clopidogrel, which is why we opted to administer platelet concentrate before the procedure. In this way, we were able to bring excessive bleeding under control and avoid acute complications for the patient.