Keywords
INTRODUCTION
Permanent His-bundle pacing is both effective and safe in patients with supra-Hisian atrioventricular block and can improve ventricular functioning.1,2 It is logical to believe, however, that the technique is only appropriate in patients with supra-Hisian atrioventricular block, and that it would be contraindicated in patients with infra-Hisian atrioventricular block.
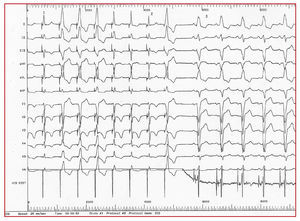
However, in electrophysiologal studies (EPS) we found that His-bundle pacing with a temporary lead led to the disappearance of complete bundle-branch block (CBBB) in some cases (Figure 1). We therefore decided to attempt definitive His-bundle pacing in selected patients with infra-Hisian conduction disturbances.
Figure 1. Stimulation via a lead located in the His-bundle (HIS DIST) in a patient with complete left bundle-branch block (CLBBB). In the first 8 complexes, various morphologies of the stimulated QRS are produced, but those marked 1 and 2 show complete disappearance of the bundle-branch block, with spike-QRS latency, due to pure Hisian capture. From 3 onwards, His-bundle pacing is stopped and the baseline CLBBB reappears.
METHODS
Patient Selection
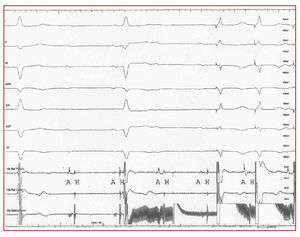
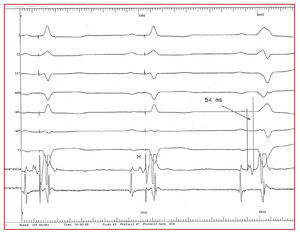
Between February and December 2004, we included 7 patients with electrocardiographic (ECG) evidence of intraventricular conduction disturbance and EPS results indicating disturbed infra-Hisian conduction. His-bundle stimulation during EPS in these patients had produced a normal or "fused" QRS complex (Figure 2). Six of the patients proposed for the intervention had been referred for EPS because of syncope. The seventh patient had heart failure due to dilated cardiomyopathy as well as complete left bundle-branch block (CLBBB) and an indication for resynchronization, which was not possible via the coronary sinus. In this patient, the EPS had shown His-bundle block (H 54 ms) which was corrected by His-bundle pacing (Figure 3).
Figure 2. Electrocardiogram of a tetrapolar lead (proximal and distal His reference) and definitive pacing lead (His-bundle pacemaker). The existence of a complete infra-Hisian atrioventricular block can be observed. The final 2 QRS complexes are "stimulated" in the His-bundle via the pacemaker lead, leading to normalized QRS morphology and duration. A indicates auriculogram; H, His-bundle electrogram.
Figure 3. DDD pacemaker with Hisian stimulation. In the first 2 QRS, capture of the His-bundle normalizes the QRS and leads to spike-QRS latency. In the third QRS, the pacemaker was switched off and a complete left bundle-branch block (CLBBB) appears with His-bundle block. The His-bundle electogram shows the proximal depolarization of the His-bundle. Stimulation was produced distal to the site of the block, which was not refractory as it had not been depolarized, even through the right branch (according to the phenomenon of anisotropy between the two branches). H indicates His-bundle electrogram.
Patients ranged from 63 to 82 years of age. There were 4 women and 3 men. The table shows the type of electrocardiographic disturbances presented by the patients.
Pacemaker Implantation
The 7 patients, 4 of whom had CRBBB (1 with added first grade supra-Hisian atrioventricular block), 2 with CLBBB, and 1 with complete infra-Hisian AVB were proposed for definitive His-bundle pacing using a biventricular DDD pacemaker. Previous His-bundle pacing had led to the disappearance of the conduction disturbance in all of the patients.
The technique used for pacemaker implantation has been described elsewhere,2 and consists of introducing a tetrapolar lead using fluoroscopy via the femoral vein until activity is registered in the His-bundle (the reference zone). The lead is advanced and the reference zone "mapped" while attempts are made to register activity in the His-bundle; when this is achieved, contact is maintained between the lead and the septum and the fixation helix is removed. Stability and thresholds are then tested (maximum accepted 2.5 V for 0.4 ms). We used 52 cm, active fixation Tendril SDX, St Jude leads (St Jude, Minneapolis). With this lead, the mechanism used to extract the fixation helix prior to implant leaves several centimeters of guideline uncovered, which are useful for manipulating and stabilizing the lead.
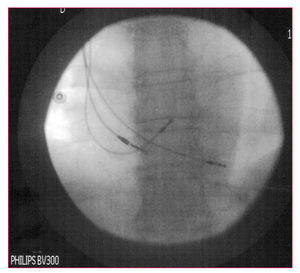
Leads were implanted in the right atrium, in the bundle of His, and, for safety, at the apex of the right ventricle (Figure 4), and connected to the atrial, left ventricular, and right ventricular terminals, respectively, of a biventricular pacemaker generator.
Figure 4. Radiological image of 3 definitive leads placed in the lower interatrial septum, His-bundle, and the right ventricular apex.
By programing an appropriate advance in the left ventricular pacing, it is possible to stimulate the "Hisian zone" exclusively and the right ventricular spike locates on the refractory QRS complex with no opportunity for originating local capture (Figure 5). When the Guidant Contak Renewal TR2CRT-P pacemaker was used (on 3 occasions), the sensitivity of the left ventricular channel was adjusted to be as "blind" as possible to avoid inhibiting stimulation of the His-bundle because of possible A wave sensing. In another 2 cases, and again to avoid this effect, we used devices in which left ventricular channel sensing was not possible, such as the Medtronic Insync III.
Figure 5. Electrocardiogram of a DDD pacemaker and His-bundle pacing. The asterisk in the descending part of the QRS indicates the back-up pacing in the right ventricle.
RESULTS
Effects of His-Bundle Pacing
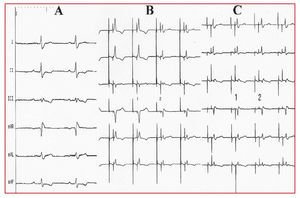
Selective His-bundle pacing using high output voltages (over 2.5 V) in the 2 patients with CRBBB led to the disappearance of the bundle-block and reduced the duration of the QRS complex (Figure 6), which acquired a "pre-excited" aspect. Using low output voltages led to a reappearance of CRBBB with spike-QRS latency and a failure to normalize QRS morphology and duration.
Figure 6. A: electrocardiogram with sinus rhythm and 250 ms PR interval showing a complete right bundle-branch block (CRBBB). B: the same electrocardiogram as in A with DDD pacemaker and sequential stimulation in the atrium and His-bundle; the first 2 QRS show His capture and capture of adjacent myocardium, a "fusion" which eliminates the CRBBB, narrows the QRS, and resynchronizes the right ventricle; the last 2 QRS show "pure" Hissian capture, with correction of the atrioventricular block and appearance of CRBBB. C: the same electrocardiogram as in B. The first 2 QRS show His-bundle capture; in the later QRS, His-bundle capture is lost (note the increase of latency in the His spike) and atrioventricular block reappears, with persistence of CRBBB.
In 2 patients with CLBBB, His-bundle pacing led to the disappearance of the bundle-block and practically normalized QRS duration and morphology. This was the case of the patient with dilated cardiomyopathy (Figure 7).
Figure 7. Electrocardiogram showing complete left bundle-branch block (CLBBB). DDD pacemaker activated from the fifth QRS on, with His-bundle pacing leading to a normalized QRS complex and disappearance of the CLBBB.
In the patient with complete infra-Hisian AVB, His-bundle pacing corrected the disturbance and normalized the QRS (Figure 2).
The His-bundle lead was successfully implanted in 5 (71%) of the 7 patients initially selected for the procedure (2 with CRBBB, 1 of whom had first-grade AVB, 2 with CLBBB, and 1 with complete infra-Hisian AVB). Acute His-bundle pacing thresholds were between 1.2 and 2.3 V with a duration of 0.4 ms. Fixation of the His-bundle lead required between 12 and 47 mins.
Follow-Up
Between 2 and 12 months follow-up, no lead dislodgement was observed, though the His-bundle pacing threshold increased in three patients to 4, 4.5 and 4.5 V for 0.4 ms at 7, 8 and 10 months, respectively. No problems arose because of oversensing.
The echo-Doppler readings did not deviate significantly from pre-implant values, except in the patient with dilated cardiomyopathy and CLBBB, in which pre-implant left ventricular dyssynchrony was normalized. There was no evidence of AV valvular incompetence.
DISCUSSION
It has been known for some time3 that selective His-bundle pacing can lead to the disappearance of CBBB. This can be explained by longitudinal dissociation in the His-bundle, a theory based on the anatomical and histological studies of James and Sherf4 which sustains that the fibers going to for the right and left branches of the conduction system are organized longitudinally and separated in the His trunk. This makes cross-excitation between the right and left bundles (anisotropy) difficult. A lesion which only affects part of the His trunk can therefore cause electrocardiographic disturbances typical of CBBBs. This has been confirmed by other authors5-9 and explains why His-bundle pacing in a zone distal to the site of the block and a Hisian extrasystole originating in that region can lead to the disappearance of CBBB.10
The fact that His-bundle pacing does not always lead to an absolutely normalized QRS complex with clear latency between the spike and the start of the QRS (His-Purkinje conduction time), can be explained by the simultaneous capture of myocardium next to the His-bundle, so that 2 depolarizing fronts are produced. One of these captures the His-bundle and activates the left ventricle via the left branch, while the other captures myocardium in the Hisian region and depolarizes and resynchronizes the right ventricle (Figure 6). The QRS complex obtained is therefore a fusion of the 2 activation fronts, and is similar to that seen in anteroseptal pre-excitation syndromes.
The fact that this did not disappear in any of the CRBBB patients in which the QRS complex was completely normalized, together with the spike-QRS to His-bundle pacing latency, can be explained by the location of the block in a peripheral region of the right branch, distal from the His-bundle.11
In patients with CLBBB, His-bundle pacing produces an almost normal QRS complex, although the short spike-QRS latency indicates some degree of adjacent myocardial capture (fusion). The disappearance of the CRBBB indicates that it is located in the His-bundle (it is impossible to "eliminate" a CLBBB by stimulating sites in the right ventricle) and that stimulation is distal to the site of the blockage (Figure 3), which remains refractory.
In patients with complete infra-Hisian atrioventricular block, the fact that His-bundle pacing produces an almost normal QRS, with minimal latency, can be explained by the mechanism described above. It also shows that the His-bundle block is proximal, and that capture occurs distally to that zone, which is free of refractoriness (Figure 2).
In the patient with dilated cardiomyopathy and CLBBB, evidence for intraventricular resynchronization produced by His-bundle pacing is provided by a return to normal echo-Doppler electromechanical patterns.
We do not know whether the increase in His-bundle pacing threshold over time is due to microdislodgement, fibrosis, or some other mechanism.
CONCLUSIONS
Permanent His-bundle pacing is possible in the majority (71%) of cases with infra-Hisian atrioventricular block and can be attempted when prior stimulation of the His-bundle leads to disappearance of the conduction disturbance (63% of the present series).
We believe that it is worth persevering this pacing site, despite the potencial drawbacks, if it means this will pursue myocardial contraction which mimics a physiological contraction. A lack of knowledge regarding the progression of the conduction disturbance, lead stability, and the evolution of pacing thresholds means that, for the time being, it is necessary to ensure ventricular capture using a back-up lead in the right ventricle.
The theory of longitudinal dissociation in the His-bundle is confirmed and explains the findings that we describe.
Correspondence:
Dr. R. Barba Pichardo.
A. Sundheim, 30, 1.° C. 21003 Huelva. España.
E-mail: rbphuelva@Yahoo.es
Received March 21, 2005. Accepted for publication March 9, 2006.