Worldwide, ischemic heart disease is the most common cause of death. In Europe, rates of ST-elevation myocardial infarction (STEMI) range from 43 to 144 people per 100,000 population per year.1 Despite the use of primary percutaneous coronary intervention (PCI) resulting in the overall trend of a reduction in mortality over the past 30 years,2 in-hospital mortality remains high with rates of between 4% and 12% in select European countries.3
Following myocardial infarction (MI), angina occurs in nearly 1 of 5 patients at 1 year. Younger age and nonwhite males, clinical history (prior coronary bypass surgery or baseline angina), index hospitalization (recurrent angina), and outpatient (persistent smoking, revascularization after index hospitalization, and depression, including new, persistent, or transient depression in the year after MI hospitalization) were associated with angina at 1 year.4 Among acute coronary syndrome patients reporting angina at 6 weeks following PCI, 92.0% received beta-blockers during the first year post-MI, yet only 23.3% were treated with other antianginal medications. At 1 year, 33.1% with 6-week angina reported persistent angina symptoms. Of these, only 31.2% had been prescribed non–beta-blocker antianginal medications at any time in the past year. Among patients undergoing revascularization during follow-up, only 25.9% were on ≥ 1 non–beta-blocker antianginal medication at the time of the procedure.5 Thus, the occurrence of ongoing angina and its optimal management is an issue post-PCI. Further studies are indeed necessary to evaluate this challenge and subsequently identify strategies to mitigate persistent angina post-PCI.
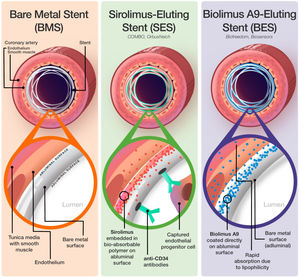
In the management of coronary artery stenosis, bare metal stents were used in the past. However, their use was complicated by a high rate of in-stent restenosis. In the context of STEMI, the ensuing procoagulant and proinflammatory state in conjunction with the stimulation of vascular smooth muscle cell proliferation and accumulation of extracellular matrix proteins due to trauma caused by stent deployment progress to develop intimal hyperplasia, reduction of lumen diameter, and finally in-stent restenosis.6
In combatting this major issue of in-stent restenosis following coronary artery stenting, drug-eluting stents (DES), which release antiproliferative drugs to inhibit smooth muscle cell proliferation and vascular endothelial cell migration, were introduced and are now used routinely.7 Coronary stenting leads to acute endothelial injury and inflammation of the stented culprit artery due to friction and physical stretching of the vessel wall, which results in denudation of endothelial cells.6 This culminates with the acute derangement of the endothelial milieu, which performs numerous physiological functions from hemostasis, vasomotor regulation, to anti-inflammation. Within 30 days, disturbance of the endothelium results in the loss of homeostasis within the vessel wall, triggering events such as platelet deposition, fibrin deposition, and attraction of leukocytes, which may contribute to the occurrence of stent thrombosis.7 The antiproliferative drugs present in DES further delay stent healing due to their pharmacodynamic effects on the cell cycle, with subsequent downstream effects on endothelial function, and raise the need for potent antiplatelet agents to reduce the incidence of stent thrombosis.
The latest generation DES are designed to improve healing and increase stent re-endothelization over previous generation stents. Sirolimus is a macrolide that functions as an immunosuppressant commonly used in DES by inhibiting the interleukin-2 (IL-2)-dependent activation of lymphocytes via blockage of the mTOR pathway.8 A lipophilic derivate of sirolimus, known as biolimus, has similar immunosuppressive potency but has the advantage of greater absorption rates through the vessel wall due to its lipophilicity and more rapidly enters vascular smooth muscle cells, causing arrest of the cell cycle, which aids in the inhibition of hyperplasia-inducing vascular smooth muscle cell proliferation.9 As both drugs affect the cell cycle, they have the adverse effect of delaying re-endothelialization. Sirolimus-eluting stents (SES) (figure 1) have been designed with a bioabsorbable sirolimus-coated polymer on the endothelial-facing side and an anti-CD34 antibody layer on the luminal side, which functions to bind circulating endothelial progenitor cells to promote re-endothelialization.10 In contrast, the biolimus A9-eluting stent (BES) (figure 1) are bioactive stents coated with biolimus, which does not possess any absorbable polymers or antibody layer and is designed to rapidly release most of the drug within 48hours postimplantation, minimizing the delay for healing caused by the drug. BES essentially becomes a bare metal stent once the biolimus A9 on the abluminal surface is eluted after 28 days, hence having similar re-endothelialization as bare metal stents.11 A number of randomized controlled trials have investigated the impact of previous generation DES on endothelial dysfunction over the years,12 but the impact of newer SES and BES toward endothelial and vasomotor function is not known.
The STEMI disease process itself leads to a more intense multifactorial endothelial dysfunction compared with other forms of coronary heart disease, aggravated by the delayed endothelialization and exposed stent struts of DES, properties which are intrinsic to their function to prevent IRS.13 As a result, investigation of the endothelial impacts of stents in the STEMI population is critical as the endothelium is a complex structure with a multitude of important homeostatic functions within the coronary artery.12 An acutely dysfunctional endothelium may favour procoagulant activity and a propensity to vasoconstriction—its consequences made evident by associations of DES-related endothelial dysfunction with persistent angina and poor clinical outcomes.14
Coronary endothelial and microvascular function distal to SES and polymer-free BES were investigated in the FUNCOMBO trial and its findings are reported in a recent article by Gómez-Lara et al., published in Revista Española de Cardiología.15 In this hypothesis-generating study, 60 patients presenting with STEMI were randomized in a 1:1 ratio to receive culprit lesion PCI with either SES (COMBO, OrbusNeich, the Netherlands) or polymer-free BES (BioFreedom, Biosensors, Switzerland), with 51 patients available for analysis. The primary objective was to compare the endothelial function of the distal stented coronary artery between stent types at 6 months, assessed invasively at a repeat functional coronary angiogram with intracoronary infusions of acetylcholine and nitroglycerin. Microvascular function was assessed as a secondary objective, using intracoronary sensors to measure microcirculatory resistance, fractional flow reserve, and coronary flow reserve. Optical coherence tomography imaging was performed to evaluate the pattern of stent healing.
The bioactive SES and polymer-free BES investigated in this current study show similar levels of endothelial dysfunction in the distal artery at 6 months (SES, 64.0% vs BES, 62.5%; P=.913). Similar levels (P> .05) of endothelium-dependent vasoconstriction in response to acetylcholine was also reported between the 2 stent types, alongside similar microvascular function and degree of lumen loss. The authors investigated stent endothelization as a potential etiological factor for the culprit artery endothelial dysfunction, with exposed stent struts an established mechanism by which increased shear stress causes downstream endothelial dysfunction.16 The role of the endothelium is made clear as nonendothelial-dependent functions remain normal. Although endothelial dysfunction remains a challenge with these new-generation DES, optical coherence tomography at 6 months showed high grades of stent healing in both stent types, with a very low level of uncovered stent struts in both bioactive SES (2.3%) and polymer-free BES (3.2%). Microcirculatory function was also preserved between the stent types. Together, these findings suggest changes to complex endothelial homeostatic processes persist after primary PCI, despite successful stent re-endothelialization at 6 months.
The study is an exploratory hypothesis-generating trial, and therefore the authors correctly present no sample size calculation; however these findings offer an interesting insight into the impact of the newest stent technologies and endothelial dysfunction in STEMI patients. Notably, details of endothelial or microvascular function immediately post-PCI were not measured and are therefore not presented.
The shift from bare metal stents to DES such as SES and BES has minimized rates of complications such as in-stent restenosis. However, over the past 20 years, the interest in the role of the coronary artery endothelium in the natural disease history of STEMI after primary PCI has increased. There was high occurrence of endothelial dysfunction at 6 months in the 2 groups in the present study (SES: 64.0% vs BES: 62.5%). The use of bioactive SES consisting of an abluminal bioabsorbable sirolimus-coated polymer with an adluminal CD34+ antibody layer designed to capture circulating endothelial progenitor cells did not seem to reduce the endothelial dysfunction compared with polymer-free BES. The impact of the endothelial dysfunction demonstrated in this current study on clinical outcomes is, however, not known.
Having identified the persistence of endothelial dysfunction, in order to minimize ongoing or recurrent angina following STEMI PCI, it is paramount that appropriate management strategies including lifestyle risk factor management and use of appropriate antianginal therapy, in particular non–beta-blocker therapy such as calcium channel blockers, long acting nitrates or nicorandil, are provided to these patients.17 Unfortunately, details regarding baseline pharmacotherapy for these patients in the FUNCOMBO study are not available. Given the persistence of endothelial dysfunction in the vast majority of patients, it is not known whether these patients were prescribed additional antispasm pharmacotherapy or whether their anginal status was evaluated at 6 months.
Of note, in this study, most included patients were men and most presenting with single vessel disease. Endothelial dysfunction and coronary microvascular dysfunction are known to occur more frequently among women, emphasizing the need to include more women in such studies.
It is known that the index of microcirculatory resistance after primary PCI has a strong inverse relationship with myocardial viability, as assessed by fluorine-18 fluorodeoxyglucose positron emission tomography and predicts infarct size, left ventricular ejection fraction, myocardial salvage, and the presence and extent of microvascular obstruction and myocardial hemorrhage as determined by cardiac magnetic resonance imaging.18 It is encouraging to know that the microvascular environment is preserved in these patients at 6 months based on coronary flow reserve and index microcirculatory resistance assessments, although notably the use of SES or BES in the epicardial vessel will not be expected to influence the microvasculature parameters.
While this is an important study with extensive detailed evaluation of epicardial and microvascular function after STEMI, further larger studies are needed to further investigate the impact of stent technology on distal endothelial dysfunction, and the impact of this endothelial dysfunction on cardiovascular events.
FUNDINGNone.
CONFLICTS OF INTERESTNone.