Keywords
INTRODUCTION
Surgical coronary revascularization is an established treatment for advanced coronary disease. According to the most recent records of the Spanish Society of Cardiovascular Surgery, more than 8000 coronary revascularization procedures were performed in 2002. However, the rate of recurrence of angina in these patients is estimated at 24% in the first year and 40% at 6 years,1 and is associated with progression of atherosclerotic disease in the native coronary arteries and/or aortocoronary bypass grafts.2
Although conventional coronary angiography is the diagnostic modality of choice for assessing the condition of bypass grafts, it has the drawback of being an invasive, expensive technique with associated complications that, although rare, can be serious.
New diagnostic modalities, most notably magnetic resonance imaging (MRI) and computed tomography (CT), have recently been developed allowing the noninvasive visualization of coronary arteries and bypass grafts. Despite its drawback of using ionizing radiation and iodinated contrast agents, CT is currently a candidate to be the technique of choice, since it offers the best spatial and temporal resolution and achieves a better signal to noise ratio than MRI.3 These qualities allow for more rapid exploration which, consequently, is more comfortable for the patient, generates fewer artifacts caused by cardiac and/or respiratory movement, and facilitates the use of slices with a thickness of ≤1 mm, a factor that is extraordinarily important given the reduced diameter of coronary arteries and bypass grafts.
Multislice or multidetector CT (MDCT) is the most widely used CT system and has been shown to have a high diagnostic accuracy in the assessment of the major coronary arteries.4-7 However, few studies have evaluated the clinical usefulness of this technique in the assessment of coronary artery bypass grafts.
The goal of the present study was to determine the diagnostic accuracy of MDCT in the assessment of aortocoronary bypass grafts by comparison with conventional invasive coronary angiography.
PATIENTS AND METHOD
Patients
A prospective study was undertaken in 38 patients (29 men) with a mean (SD) age of 66.7 (9.9) years (range, 39-83 years) who had undergone surgical revascularization and in whom angiographic assessment of coronary bypass grafts was clinically indicated due to recurrence of symptoms of ischemia (29 patients, 76.4%) or deterioration of systolic function (9 patients, 23.6%).
All patients were in sinus rhythm and had a mean heart rate of 62.4±6.4 beats/min (range, 50-75 beats/min). Patients were excluded if they presented persistent cardiac arrhythmia (including frequent extrasystoles), kidney failure, or allergy to iodinated contrast agents, or if they were unwilling to perform a single breath-hold of sufficient length.
All patients were assessed by conventional angiography and MDCT (from January 2003) with a gap between the 2 procedures of 27.7±43.2 days (range, 1-175 days).
One hundred and seventeen coronary artery bypass grafts were assessed on the basis of surgical reports: 42 artery grafts (33 from the left mammary artery, 2 from the right mammary artery, and 7 from the radial artery) and 75 saphenous vein grafts (of which 6 were sequential). Table 1 shows the types of coronary artery bypass grafts and the native coronary arteries that were revascularized.
All patients gave informed consent to participate in the study.
Multidetector Computed Tomography
A 16-detector scanner (LightSpeed 16, General Electric Medical Systems, Milwaukee, Wisconsin, USA) was used with a complete rotation time of 500 ms and an acquisition rate of 32 slices per second. The slice thickness was set at 1.2 mm in order to acquire a volume that would include the entire thorax within a single breath-hold that was tolerable for the patients (<30 s).
Markers equivalent to standard posteroanterior and lateral radiographic projections of the chest were used to determine the arrival time of iodinated contrast agent (Iopromide, Clarograf 300, Juste S.A.Q.F., Madrid, Spain) to the ascending aorta (at the level of the carina) based on a sample volume of 13 mL injected into the antecubital vein at a rate of 5 mL/s. This data was then used to establish the acquisition time following administration of the definitive volume of contrast agent (130 mL at 5 mL/s). The chest volume, from the supraclavicular area to the diaphragmatic domes, was calculated using the same projections.
A voltage of 120 kV was used with a current of 300-350 mA and the radiation dose depended on the morphologic characteristics of each patient. No beta-blockers were administered prior to the procedure.
Acquisition was synchronized with the electrocardiogram (ECG) and 1.2 mm slices were then reconstructed for the entire volume acquired during predetermined phases of the cardiac cycle (from 0% to 90% in sequential 10% increments) in order to obtain reconstructions during the phase with the least cardiac movement artifact.
Image analysis was performed using a workstation (Advantage Work Station 4.2, General Electric Medical Systems, Milwaukee, Wisconsin, USA) with specific software for cardiovascular analysis. The following reconstructions were used: multiplane reformat (MPR), maximum intensity projection (MIP), and volume rendering (3D-VR). Each study was interpreted by a cardiologist with experience in performing and interpreting cardiovascular CT and MRI studies, and by a radiographer with extensive experience in performing vascular CT studies; both were blinded to the results of conventional coronary angiography.
Bypass graft patency was assessed along with the presence of significant stenosis (>50% reduction of lumen diameter at any point in the graft, based on visual estimation).
Conventional Coronary Angiography
Conventional coronary angiography of the bypass grafts was performed using a Coroskop Plus/TOP (Siemens, Munich, Germany) with femoral artery puncture and, wherever possible, selective catheterization; standard angiographic projections were performed. Image analysis was performed by the attending interventional cardiologist and, as with MDCT, the presence of lesions in the bypass grafts was assessed visually.
Statistical Analysis
In the descriptive analysis of the study sample, continuous variables were expressed as means (SD), whereas qualitative variables were expressed as percentages.
To determine the diagnostic value of MDCT in the noninvasive assessment of significant lesions (>50% stenosis or occlusion) in aortocoronary bypass grafts, the sensitivity, specificity, predictive values (positive [PPV] and negative [NPV]), and the diagnostic accuracy were calculated. These values were calculated using a 2x2 contingency table in which conventional invasive coronary angiography was taken as the standard. Values were calculated separately for venous and arterial grafts, as well as for all bypass grafts together. The 95% confidence interval (CI) was calculated for each of the diagnostic parameters.
RESULTS
With the exception of 1 patient who displayed deterioration of kidney function (shown by an increase in serum creatinine concentration from 1.45 to 3.16 mg/dL), no complications were observed in any of the patients during the MDCT study.
Of the 117 aortocoronary bypass grafts indicated in surgical reports, 99 grafts (84.6%) were visualized by conventional invasive coronary angiography (Table 2), either by selective injection or indirectly; 37 of the visualized grafts were arterial and 62 were venous. Seventeen occlusions were identified (3 in internal mammary grafts and 14 in saphenous vein grafts), along with 8 stenoses of more than 50% (3 in mammary artery grafts and 5 in saphenous vein grafts).
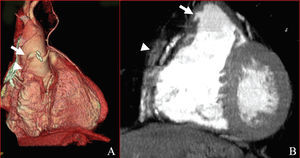
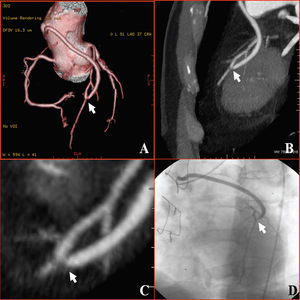
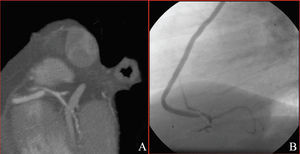
One hundred nine coronary bypass grafts (93.2%) were visualized by MDCT: 41 arterial and 68 venous (Table 2). Twenty seven occlusions (6 in internal mammary artery grafts, 1 in a radial artery graft, and 20 in saphenous vein grafts; Figure 1) and 8 significant stenoses (4 in internal mammary artery grafts and 4 in saphenous vein grafts; Figures 2 and 3) were detected.
Figure 1. Occlusion at the origin of a saphenous vein graft to the right coronary artery (arrows). The trajectory of the thrombosed graft is shown (arrowhead). A: three-dimensional volume-rendering reconstruction. B: maximum intensity projection reconstruction.
Figure 2. Saphenous vein graft to the anterior descending artery with significant stenosis of its distal anastomosis (arrows). A: three-dimensional volume-rendering reconstruction. B and C: maximum intensity projection reconstruction. D: conventional coronary angiography.
Figure 3. Saphenous vein graft to the right coronary artery with significant stenosis of its distal anastomosis. A: maximum intensity projection reconstruction. B: conventional coronary angiography.
To determine the diagnostic capacity of MDCT in the noninvasive assessment of significant lesions (occlusion or >50% stenosis) in aortocoronary bypass grafts, 98 grafts were compared (37 arterial and 61 venous) that were visualized using both techniques (Table 3); 1 saphenous vein graft visualized by invasive coronary angiography was not visualized by MDCT.
A diagnostic sensitivity of 89.5% was obtained for the saphenous vein grafts (17 significant lesions identified by MDCT out of 19 detected with conventional coronary angiography), with a specificity of 97.6% (41 grafts without lesions in MDCT out of 42 seen in conventional coronary angiography), a PPV of 94.4%, and an NPV of 95.4% (Table 3).
All of the 6 significant lesions in arterial grafts identified by invasive coronary angiography were detected by MDCT (diagnostic sensitivity of 100%). In addition, a diagnostic specificity of 96.8% (30/31), a PPV of 85.7% (6/7), and an NPV of 100% (30/30) was obtained for the arterial grafts (Table 3).
The overall sensitivity of MDCT in the detection of significant lesions in coronary artery bypass grafts was 92% (23 lesions correctly diagnosed by MDCT out of 25 visualized by conventional angiography; 95% CI, 81.4%-100%) and the overall specificity 97.3% (71 grafts without lesions according to MDCT out of 73 classified as without lesions by conventional angiography; 95% CI, 93.5%-100%). The overall PPV was 92% (95% CI, 81.4%-100%) and the overall NPV was 97.3% (95% CI, 93.5%-100%). The diagnostic accuracy of MDCT in the noninvasive assessment of all aortocoronary bypass grafts was 95.9% (94 out of 95 bypass grafts compared were correctly diagnosed by MDCT; 95% CI, 92%-99.8%; Table 3).
DISCUSSION
Although conventional angiography is considered to be the method of choice for the visualization of coronary bypass grafts, it is an invasive, expensive technique that is not without associated risks. Consequently, it is of interest to develop diagnostic modalities that allow reliable noninvasive assessment of coronary artery bypass grafts.
Despite the drawback of using ionizing radiation and iodinated contrast agents, CT offers a better combination of high spatial and temporal resolution than its closest competitor, MRI. This allows explorations to be performed with only a short single breath-hold period and facilitates visualization of small-diameter vascular structures, such as artery grafts and the distal vessels of native coronary arteries. Compared with electron beam CT, current MDCT devices allow a larger volume to be covered in a shorter single breath-hold period, with a narrower slice thickness (greater temporal and spatial resolution). This makes it the ideal technique for assessment of both coronary artery bypass grafts and native coronary arteries.3
Nevertheless, there are factors that impede its generalized use and affect image acquisition, such as the presence of arrhythmias and incorrect breath holding, or interpretation, such as artifacts caused by metallic clips and endoprostheses (stents), extensive calcification of the coronary arteries, and interposition of venous structures.
Few studies have compared the diagnostic accuracy of MDCT with conventional coronary angiography for the assessment of coronary artery bypass grafts (Table 4).4,8-13 The study of Ropers et al,8 which used a scanner with 4 detectors and included a larger number of bypass grafts (182 grafts in 65 patients), found a diagnostic sensitivity and specificity of 97% and 98%, respectively, for occlusion, and 75% and 92%, respectively, for significant stenosis. However, a major limitation of that study was the high percentage (38%) of patent bypass grafts visualized by coronary angiography that could not be assessed by CT due to movement artifacts,despite the fact that 86% of patients received treatment with beta-blockers.
Although our study, using a 16-detector scanner, yielded similar results (diagnostic sensitivity of 92% and specificity of 97.3%), it has the advantage that none of the evaluated bypass grafts were excluded due to artifacts derived from cardiac and/or respiratory movement. This was due to a number of factors. Firstly, the use of a larger number of detectors allowed higher temporal resolution and, consequently, faster data acquisition and a shorter single breath-hold period, thereby limiting movement of artifacts considerably.14 Also, although neither beta-blockers nor any other medication that reduces heart rate were administered prior to CT, the heart rate was never greater than 75 beats/minute in any of the patients; this would undoubtedly have reduced the number of cardiac movement of artifacts. Furthermore, all patients received instruction in holding their breath and their ability to do so was confirmed prior to the procedure, leading to a reduction in the number of artifacts caused by incorrect breath holding. Finally, images were reconstructed in the different phases of the cardiac cycle and those with the least movement artifacts were selected. Our experience is consistent with the logical assumption that coronary bypass grafts, as a result of their trajectory, are generally less affected by cardiac movement than native coronary arteries.
The results obtained in this study are also comparable to those obtained in the recent study of Schlosser et al,13 performed with a CT scanner that had the same number of detectors and used a similar protocol.
Although in some studies special data acquisition protocols are used in MDCT of the coronary arteries when the heart rate is high, such studies use data from various consecutive beats to reconstruct an image, thereby necessitating an extremely regular heart rhythm.11,14 In our study, we did not employ these protocols as a result of the baseline heart rate of the patients (mean of 62 beats/minute, due to the fact that the majority received chronic treatment with beta-blockers), and also because aortocoronary bypass grafts are less affected by cardiac movement.
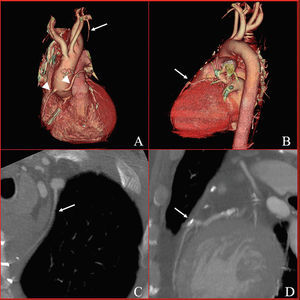
The slice thickness was 1.2 mm, with increments of 1.2 mm in the reconstruction. The reason that a slice thickness of less than 1 mm was not used, despite this possibility being available, was the impossibility of covering the volume of the chest within a single breath-hold period that was tolerable for the patient (<30 seconds). In practice, this implies a lower spatial resolution, which could have a particular influence on the visualization of small-diameter vessels. In our study, MDCT allowed assessment of 11 bypass grafts that could not be assessed by conventional coronary angiography: 2 internal mammary artery grafts occluded in their proximal segment (Figure 4) and 1 sequential graft from the left internal mammary artery to the stenotic marginal artery; 1 radial artery graft occluded at its origin; and 7 saphenous vein grafts, 1 patent and the remaining 6 occluded. Invasive coronary angiography allowed evaluation of a sequential vein graft to a right posterolateral branch that was not identified by MDCT.
Figure 4. Left mammary artery bypass graft to the anterior descending artery occluded in its proximal segment (arrows in A and C) with a patent distal native vessel (arrows in B and D). Two saphenous vein grafts are shown (arrowheads in A). A and B: three-dimensional volume-rendering reconstruction. C and D: maximum intensity projection reconstruction.
Two false negatives corresponding to saphenous vein grafts were obtained in which a significant stenosis in the distal anastomosis to small-diameter vessels (marginal and diagonal) was not identified by MDCT.
Two false positives were obtained in this study: an internal mammary artery bypass graft to the anterior descending artery, probably caused by artifacts due to metal clips at the distal anastomosis, and a saphenous vein graft in which the severity of the stenosis was overestimated by MDCT.
Considering stenosis and occlusion together, an internal mammary artery graft was classified as occluded by MDCT, whereas it was classified by invasive coronary angiography as displaying diffuse narrowing of the graft (string sign) associated with competitive flow from the native coronary artery that did not present significant narrowing prior to the bypass graft.
Limitations
Due to the limited number of stenoses compared with occlusions, a finding that is similar to those of other studies,9,11,12 the diagnostic accuracy of MDCT was not assessed separately for significant stenosis and occlusion of bypass grafts.
A slice thickness of 1.2 mm rather than less than 1 mm was used for data acquisition in order to cover the total chest volume during a single breath-hold period that was tolerable for the patient. This implies a lower spatial resolution and perhaps explains the failure to detect the distal stenoses of the 2 venous grafts to the marginal and diagonal arteries (vessels with a smaller diameter than the main coronary arteries).
The presence of a coronary steal phenomenon by the native vessel due to revascularization in the presence of nonsignificant stenosis can lead to, as in our case, a graft to be considered occluded when by conventional coronary angiography, a dynamic technique, it would be considered patent but with a reduced internal diameter.
Although it was not the aim of this study to assess the native vessels, nor to determine the effective dose of ionizing radiation received by the patients, either with conventional coronary angiography or MDCT, these aspects will be important if the technique is to be employed in general clinical practice.
CONCLUSIONS
In our study, the assessment of coronary artery bypass grafts with MDCT showed a high diagnostic accuracy compared with invasive coronary angiography in patients in whom conventional coronary angiography was clinically indicated. However, confirmation of the high negative predictive value obtained in this study, which would allow the technique to be used as a valid alternative to conventional coronary angiography, will require a more extensive series that also includes native vessels.
Correspondence: Dr. F. Ridocci Soriano.
Servicio de Cardiología. Consorcio Hospital General Universitario de Valencia.
Avda. Tres Cruces, 2. 46014 Valencia. España.
E-mail: ridocci_fra@gva.es