To the Editor:
Primary cardiac tumors1 are very uncommon. They include the myxoma, which constitutes between 42% and 77% of these lesions. In contrast, metastatic cardiac tumors are more common, and their incidence in autopsies of patients with generalized neoplasms ranges between 10% and 20%.2 Melanoma is the tumor that most frequently produces cardiac metastases, followed by malignant germ cell tumor (in a series of 100 necropsies in patients with this tumor, 38% presented cardiac metastases3).
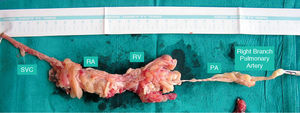
We report the case of a 38-year-old man who, in 2003, was diagnosed as having a testicular germ cell tumor, with mediastinal, pulmonary and retroperitoneal spread. He underwent right orchiectomy and chemotherapy, followed by sequential resection of the retroperitoneal, mediastinal, and pulmonary lesions. Although follow-up examinations indicated that he was disease-free, central venous access (Port-A-Cath®) was maintained. In August 2004, an echocardiogram was carried out when auscultation of a murmur revealed a mass originating in the superior vena cava. It initially presented a tubular morphology, but would later acquire a cluster form with multiple protuberances. It was mobile and extended through the right atrium and ventricle, and pulmonary artery and its right branch, where it ended. Chest computed tomography showed important filling defects in right heart chambers. As the presence of thrombi was suspected, treatment with sodium heparin was begun. Lung scintigraphy was indicative of embolisms in the middle and lower lobes of the right lung. Despite the anticoagulant therapy, the echocardiographic images remained the same and, thus, the decision was made to perform surgery. The lesion was a large, multipedicled tumor mass originating in superior vena cava, with no endocardial adhesions in atrium or ventricle, and with necrotic zones along its entire length. On palpation, it appeared to originate in an inaccessible region above the azygos vein. The lesion was resected in its entirety with the exception of residual pedicle at the base (Figure 1). Another implantation site, measuring 33 cm, observed on the anterior aspect of right ventricle was biopsied. The pathological diagnosis was myxoma. Seventeen months later, echocardiograms again revealed progressive growth of the tumor, with a large vegetative mass originating in superior vena cava extending through the right atrium and ventricle, passing through the pulmonary valve and reaching the main pulmonary artery. The decision was made to perform surgery yet again and a yellowish, clustered, multinodular tumor originating in the brachiocephalic trunk was found. It was not attached to the endocardium and was completely resected. The pathological examination involved calretinin immunolabeling, which proved to be positive, resulting in a diagnosis of villous myxoma (Figure 2).
Figure 1. Macroscopic image of the resected tissue. The myxoma adopts the shape of the cavities. Thus, its diameter is much greater in right atrium and ventricle than in the vena cava or pulmonary artery. Likewise, the diameter is greater in the main pulmonary artery than in the branch. The different portions of the myxoma are indicated. RA indicates right atrium; PA, main pulmonary artery; SVC, superior vena cava; RV, right ventricle.
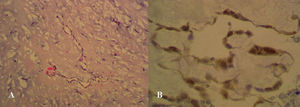
Figure 2. Microscopic image of the resected tissue. A: hematoxylin-eosin. B: immunolabeling for calretinin. Calretinin expression is observed along the length of the sheath covering the myxoma.
This case is of interest because of the rarity of the tumor itself, which had a vermiform shape from its onset in the superior vena cava, reached the right chambers, passed through them without interruption, widened in the right atrium and right ventricle, narrowed when it passed through the respective tricuspid and pulmonary valves, and ended in the pulmonary artery, in short, adopting the intracavitary shape of the structures it passed through (Figure 1). This macroscopic description would correspond to a villous myxoma, a less common subtype of myxoma.6
This case report is entirely exceptional due to the nature of the intracardiac tumor, a myxoma, with no apparent connection to the initial lesion, despite the fact that testicular germ cell tumors have been described as neoplasms that can lead to cardiac metastases3; due to the location of the myxoma, which originated in the superior vena cava-brachiocephalic trunk, the venous site being highly exceptional, although it has been reported in inferior vena cava and femoral vein7,8; and, finally, due to its ability to grow and recur after the first operation.
The most difficult aspect to explain is the association between the myxoma and the initial neoplasm, if it exists. The form and location of this myxoma would support the hypothesis of those who once defended a thrombotic origin. Taking into account its intracavitary site and the fact that the patient had a Port-A-Cath®, and accepting the prothrombotic tendency of cancer patients, the origin could be attributed to this circumstance. One argument against this could be the presence of a synchronous lesion of the same histology on the anterior aspect of right ventricle. Moreover, in this case, it was possible to confirm the nature of the myxoma by an immunohistochemical test for calretinin, a technique that is totally specific for the differentiation of a myxoma from a thrombus.5
The final lesson to be learned from this case is that any abnormal growth should be subjected to pathological examination, regardless of the history. In this patient, with his complex and extensive history of neoplastic disease, it could have been assumed that the present intracardiac mass was metastatic and did not warrant treatment, when, in reality, it was benign and, to a great extent, resectable.