Keywords
INTRODUCTION
Thrombolysis in Myocardial Infarction (TIMI) grading system and myocardial perfusion grade (MPG) are angiographic markers of efficacy of coronary reperfusion at the epicardial artery and microcirculation levels.1,2 These markers predict adverse clinical outcomes including short3,4 and long term2,5,6 mortality. There is a mutual interrelation and dependence between these markers. Restoration of an optimal epicardial flow is a prerequisite for restoration of normal reperfusion at the microcirculation level3,4 and the latter is a precondition for unimpeded blood flow in the epicardial coronary system. Stone et al.3 and Constantini et al.4 and a previous work from our group7 have demonstrated that none of the patients with restoration of the suboptimal epicardial flow (TIMI grade ≤2) had optimal flow at the microcirculation level (MPG 3). Restoration of suboptimal epicardial flow (TIMI grade ≤2) denotes increased segmental coronary resistance due to severe vascular obstruction and is associated with extensive myocardial necrosis, reduced myocardial salvage with primary percutaneous coronary intervention (PCI), negative left ventricular remodeling and increased mortality.8,9 Nevertheless, restoration of normal epicardial blood flow (TIMI grade 3) does not mean optimal reperfusion at the microcirculation level. Several studies have shown that a sizeable portion of patients with TIMI grade 3 have suboptimal myocardial reperfusion at the microcirculation level.3-5 In particular, the prognostic value of MPG 2 remains controversial.3-6,10
In this study, we investigated the prognostic value of MPG in patients with STEMI, in whom a TIMI flow grade of 3 was restored with primary percutaneous PCI. The aim of the study was twofold: first, to investigate the relationship between MPG, initial area at risk, myocardial salvage and infarct size; and second, to investigate the prognostic impact of MPG on long term (5-year) mortality. The exclusion of patients with TIMI grade ≤2 reduced the interference of variations in the epicardial blood flow and enabled the assessment of pure impact of MPG on the outcomes.
METHODS
Patients
The primary study sample consisted of 1861 patients with STEMI presenting within the first 24 hours from the symptom onset at the Deutsches Herzzentrum and 1. Medizinische Klinik rechts der Isar in Munich, between January 2002 and December 2007. Details of the primary study sample were reported in another work from our group.7 After exclusion of patients treated conservatively (n=112) and with thrombolysis or coronary artery bypass surgery as primary reperfusion strategy (n=53), those with mechanical failures to open occluded coronary arteries (n=31), missing scintigraphic examinations (n=173) or with data of inadequate quality (n=86) and those with a Thrombolysis in Myocardial Infarction (TIMI) flow grade ≤2 (n=193), 1213 patients with STEMI and a TIMI flow grade of 3 at the end of primary PCI remained and were included in this study. All the study patients had paired scintigraphic examinations, before and 7 to 14 days after PCI. The diagnosis of STEMI was established in the presence of chest pain lasting more than 20 minutes associated with electrocardiographic changes (ST segment elevation of ≥1 mm in at least 2 extremity electrocardiographic leads or ≥2 mm in at least 2 contiguous precordial leads or left bundle branch block of new onset). The diagnosis was confirmed by coronary angiography in all patients. Severity of heart failure was assessed according to Killip classification.11
Angiographic Analysis
Coronary angiography was performed according to standard criteria. Offline analysis of digital angiograms was performed in the core laboratory using an automated edge detection system (CMS; Medis Medical Imaging Systems, Neuen, the Netherlands) by personnel blinded to the clinical diagnosis. Primary PCI (mostly with stent implantation) and periprocedural care were performed according to the standard criteria. Stents (mostly bare-metal stents) were used in 88% of patients (n=1066). Antiplatelet therapy consisted of clopidogrel (600 mg as a loading dose followed by 75 mg/day for at least 4 weeks to 6 months) and aspirin (200 mg/day continued indefinitely).
Epicardial blood flow in the infarct-related artery and MPG were graded according to the Thrombolysis in Myocardial Infarction (TIMI) group definitions.1 TIMI flow grade was defined as follows: TIMI 0, no perfusion (no antegrade flow beyond the point of occlusion); TIMI 1, penetration without perfusion (the contrast material passes beyond the area of obstruction, but fails to opacify the entire coronary bed distal to the obstruction for the duration of the cine run); TIMI 2, partial reperfusion (the contrast material passes across the obstruction and opacifies the coronary bed distal to the obstruction with rates of entry in and clearance from the distal bed perceptibly slower than its entry into and/ or clearance from comparable areas perfused by contralateral non-infarct artery or coronary bed proximal to the obstruction); TIMI 3, complete perfusion (contrast material enters and exits the bed distal to the obstruction as promptly as in the bed proximal to the obstruction or in the bed from uninvolved contralateral coronary artery).
Myocardial perfusion grade (MPG) was defined as follows: MPG 0, contrast fails to enter the microvasculature; MPG 1, contrast material slowly enters but fails to exit the microvasculature; MPG 2, delayed entry and exit of contrast material from the microvasculature; MPG 3, Normal entry and exit of contrast from the microvasculature.1 In a sample of 50 patients, the intraobserver and interobserver agreements were 94% (47/50) and 88% (44/50) regarding the MPG grading. No discrepancy >1 in MPG grading was observed.
Scintigraphic Study
99mTc-sestamibi single photon emission computed tomography (SPECT) was performed at baseline (before PCI) and 7-14 days after PCI. Patients received an intravenous injection of 27 mCi (1000 MBq) of 99mTc-sestamibi and SPECT was performed 6-8 hours after injection of radioactive agent. A multihead camera system, equipped with low energy and high resolution collimators was used for myocardial imaging. Images were acquired in a 64 ´ 64 matrix by an acquisition time of 40 seconds per image. With dedicated software (ICON Version 6.0.2) transaxial slices were reconstructed. A volumetric sampling tool was applied to create polar maps of relative distribution throughout the entire left ventricle. Each polar map was normalized to its individual maximum. The defect size was defined as the <50 uptake area the scintigraphic parameters were: initial perfusion defect in baseline scintigraphy before intervention final infarct size follow-up absolute salvage minus and index divided by first 3 were expressed as percentage of left ventricle 4th parameter denotes proportion salvaged reperfusion all measurements performed core laboratory investigators unaware clinical diagnosis p
Endpoints and Follow-up
The primary outcome of this analysis was five-year mortality. The extent of initial area at risk (initial perfusion defect), final infarct size and salvage index in groups with various MPG groups were also assessed. The follow-up information was obtained by a phone call at 30 days, a visit at 6 months, a phone call at 1 year and yearly phone calls thereafter. Patients who had cardiac complaints underwent a complete clinical, electrocardiographic, and laboratory evaluation. Information about death was obtained from hospital records, death certificates or phone contact with relatives of the patient or referring physician. The follow-up information was obtained by personnel blinded to the clinical or angiographic characteristics of the patients.
Statistical Analysis
Data are presented as median (with 25th-75th percentiles) or counts and proportions (percentages). The one-sample Kolmogorov-Smirnov test showed an abnormal data distribution for all continuous variables under consideration. Categorical data were compared with chi-square test. Continuous data were compared with Kruskal-Wallis rank sum test. Five-year mortality was estimated by applying the Kaplan-Meier method and log rank test which allowed the calculation of odds ratios (95% confidence intervals and respective P values) associated with various MPG grades. The association between MPG and 5-year mortality was tested in the Cox proportional hazards model. To reduce the over-fitting of the model, MPG and parameters of Tables 1 and 2 that showed a P<.05 with the exclusion of creatine kinase and cardiac troponin (scintigrahic infarct size in the 7-14 days scintigraphy was entered instead) were entered into the model. All analyses were performed using S-plus statistical package (S-PLUS, Insightful Corp, Seattle, Washington). A P<.05 was considered to indicate statistical significance.
RESULTS
Baseline Characteristics
This study included 1213 patients with STEMI and TIMI flow grade 3 at the end of primary PCI. Of them, there were 217 patients with MPG 0-1, 195 patients with MPG 2 and 801 patients with MPG 3. Baseline clinical characteristics of the 3 groups are shown in Table 1. There were significant differences between groups regarding age, proportions of patients with previous coronary artery bypass surgery, infarct location, Killip class, creatine kinase MB activity, concentrations of cardiac troponin, C-reactive protein and serum creatinine and time-to admission interval. Interestingly, the groups with MPG 0-1 and 2 appear to differ little with regard to almost all baseline characteristics (with the exception of anterior infarct location which was more frequent among patients with MPG 2) which shows that both groups have similar cardiovascular risk profiles. Conversely, the group with MPG 3 had a more favorable cardiovascular risk profile and this group was the main cause of trends showing statistically significant differences between groups. Angiographic characteristics are shown in Table 2. Patients with MPG 3 had better left ventricular ejection fraction than the other 2 groups. There were differences in the infarct-related artery. Patients with MPG 3 had lower proportions of patients with pre-interventional TIMI 0 and 1 and greater proportions of patients with TIMI grade 2 and 3 than the other 2 groups. Interestingly, patients with MPG 3 had a higher proportion of patients with no collateral circulation documented by angiography compared to patients with MPG 0-1 or 2 (Table 2).
Schintigraphic Data
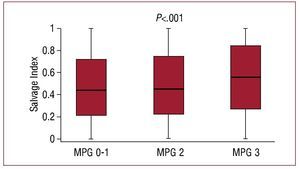
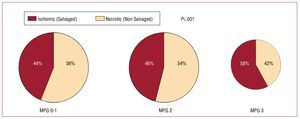
The results of scintigraphic examinations are shown in Table 3. All seen in the Table, all 4 scintigraphic parameters appear to differ little among patients with MPG 0-1 and 2. Compared to patients with a MPG 0-1 or 2, patients with a MPG 3 had a significantly smaller initial perfusion defect (equivalent to initial area at risk) and infarct size (perfusion defect in the 7-14 days scintigraphy). Of note, in patients with a MPG 3, the salvage index or the proportion of the initial perfusion defect salvaged by primary PCI was significantly higher than in patients with MPG 0-1 or 2 (Figure 1). Based on the salvage index (the proportion of the initial perfusion defect salvaged), the ischemic/necrotic proportions of the initial area at risk were estimated (Figure 2). The figure shows that the proportion of salvaged tissue (ischemic) within the initial area at risk was significantly greater among patients with MPG 3 compared to patients with MPG 0-1 or 2. Conversely, necrotic portion (proportion of initial perfusion defect not salvaged by reperfusion) was more prominent among patients with MPG 0-1 and 2 than among patients with MPG 3 (Figure 2).
Figure 1. Salvage index (proportion of initial perfusion defect salvaged by primary PCI) according to MPG groups. MPG indicates myocardial perfusion grade; PCI, percutaneous coronary intervention.
Figure 2. Salvaged (ischemic) and non-salvaged (necrotic) proportions of the initial perfusion defect according to MPG groups. MPG indicates myocardial perfusion grade.
Myocardial Perfusion Grade and 5-Year Mortality
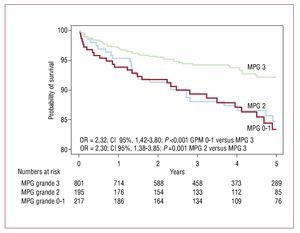
The median [25th-75th percentiles] follow-up was 4.1 [2.1-4.9] years. There were 101 deaths during the follow-up: 28 deaths occurred in patients with MPG 0-1, 25 deaths occurred in patients with MPG 2 and 48 deaths occurred in patients with MPG 3 (Kaplan-Meier estimates of 5-year mortality 16.6%, 15.3%, and 7.8%, respectively, odds ratio [OR]=2.32, 95% CI 1.42-3.80], P<.001 for MPG 0-1 versus MPG 3 and OR=2.30, 95% CI 1.38-3.85, P=.001 for MPG 2 vs MPG 3; Figure 3).
Figure 3. Kaplan-Meier curves of 5-year mortality in patients with MPG 0-1, 2, and 3 after primary PCI. MPG indicates myocardial perfusion grade; PCI, percutaneous coronary intervention.
The association between MPG and all-cause 5-year mortality was tested in the Cox proportional hazards model (see methods for variables entered vs MPG 0-2). Other correlates of 5-year mortality were: age (HR=1.67; 95% CI, 1.38-2.03; P<.001, for 10-year increase in age), Killip class (HR=1.41, 95% CI 1.11-1.79; P=0.005, for 1 class increase) and previous myocardial infarction (HR=2.14; 95% CI, 1.29-3.55; P=.003).
DISCUSSION
In this study, we investigated the impact of MPG on scintigraphic indexes of reperfusion and long-term mortality in a relatively large series of patients with STEMI undergoing primary PCI. To avoid the variability in MPG measurements between various laboratories12, all measurements of reperfusion markers were performed in a centralized core laboratory. The main findings can be summarized as follows: a) in patients with restoration of TIMI grade 3, suboptimal myocardial reperfusion (MPG ≤2) was associated with larger initial areas at risk and reduced myocardial salvage by primary PCI; b) suboptimal myocardial reperfusion was associated with increased all-cause mortality into the model). Because the probability of 5-year survival was similar between patients with MPG 0-1 and MPG 2, these 2 groups were merged as the group with MPG 0-2. The Cox proportional hazards model identified the MPG as an independent correlate of 5-year mortality (adjusted hazard ratio [HR] = 0.65; 95% CI, 0.41-0.97; P=.037 for MPG 3 up to 5 years after acute event; c) patients with STEMI and MPG 0-1 and MPG 2 appear to differ little with regard to initial area at risk, amount of myocardium salvaged by primary PCI, infarct size and 5-year mortality.
Our study showed that patients with suboptimal tissue reperfusion (MPG ≤2) had greater initial areas at risk quantified by scintigraphy. In a prior study by Dibra et al,10 initial area at risk did not differ significantly among patients with closed microcirculation (MPG 0-1) versus those with open microcirculation (MPG>2). However, in this study10 patients with MPG 2 were grouped with patients with MPG 3 whereas in the present study patients with MPG 2 were analyzed as a distinct group. Both studies reported reduced myocardial salvage and increased infarct size in patients with suboptimal tissue reperfusion. Along the same lines, Angeja et al13 have shown reduced scintigraphic infarct size in patients with restoration of the reperfusion at the tissue level.
Paired scintigraphic studies, allowed us to quantify the necrotic and ischemic proportions of initial area at risk. Our data offer additional evidence on the structural and functional components of microvascular obstruction and no-reflow as proposed by Galiuto and Crea.14 Furthermore, we found that the necrotic portion of initial perfusion defect was greater in patients with MPG≤2 than in patients with MPG 3. Consequently, patients with MPG 3 had greater portions of ischemic but still viable myocardium within the initial perfusion defect. This finding could be of importance for explanation of the angiographic assessment of reperfusion at the tissue level. Morphologic studies by Kloner et al15 have shown that myocardial cell damage occurs earlier than microvascular damage in the course of myocardial ischemia suggesting that microvascular tissue is more resistant to ischemia than myocardial tissue. In this study we used a combination of an extracellular tracer (contrast dye) supposed to reflect the openness of the microcirculation2 and an intracellular marker (99mTc-sestamibi) supposed to show viability of surrounding working myocardium.16 On one hand, the presence of large areas of ischemic but viable myocardial tissue inside the initial areas at risk in patients with optimal tissue reperfusion explains greater myocardial salvage, smaller infarct size and better prognosis in these patients. On the other hand, upon the opening of the infarct-related artery by primary PCI, the vascular bed in the ischemic areas may allow flowing of considerable amount of blood due to ischemia-induced vasodilatation.17 This could have 2 implications: First, blood overflowing in the ischemic vascular bed may compensate for segmental vascular obstruction in the core necrotic region allowing an un-impeded epicardial blood flow (TIMI grade 3). Blood redistribution toward ischemic regions and smaller initial areas at risk could be crucial for explaining normal epicardial blood flow despite segmental vascular obstruction in patients with preserved epicardial blood flow and various degrees of suboptimal tissue reperfusion. Second, contrast dye opacification of ischemic regions may mask areas with perfusion alterations making it difficult to appraise the segmental tissue perfusion, thus limiting the accuracy of angiographic methods in the assessment of tissue reperfusion.12
Several prior studies have investigated the association between suboptimal tissue perfusion and increased mortality in patients with STEMI undergoing reperfusion.3-6 In patients with acute myocardial infarction and restoration of TIMI flow grade 3 by angioplasty, Henriques et al5 did not report differences in survival between patients with MPG 2 and 3 over a mean follow-up of 16 months. Similar findings were reported by Haager et al.6 In the studies by Stone et al.3 and Constantini et al,4 patients with MPG 2 had a distinct and intermediate survival curve between survival curves of patients with MPG 0-1 and 3. The novel finding of the present study consists in showing that patients with MPG 0-1 and 2 had similar 5-year mortalities. Reasons for the discrepancy between these studies and the present study regarding mortality remain unknown. Interestingly, patients with MPG 0-1 and 2 showed striking similarity regarding baseline risk, initial area at risk, amount of salvaged myocardium and infarct size. These similarities may underlie similar long-term mortalities and strongly suggest that MPG 2 is not an index of optimal tissue perfusion and should not be considered a benign angiographic sign. In a study of 27 patients with STEMI, Porto et al18 have shown that patients with MPG 2 have relatively preserved perfusion, similar to patients with MPG 3 but with larger infarct size similar to patients with MPG 0-1. Thus, the study by Porto et al18 and the present study suggest that when assessing the results of tissue reperfusion after primary PCI, grouping together patients with MPG 2 and 3 is not justified and they should be considered separately when assessing MPG prognostic impact.
CONCLUSION
In conclusion, in patients with STEMI and restoration of TIMI grade 3 by primary PCI, suboptimal myocardial reperfusion (MPG≤2) was associated with larger initial areas, reduced myocardial salvage, larger infarct size and increased 5-year mortality compared to patients with restoration of perfusion at tissue level (MPG 3). Patients with MPG 2 did not differ to patients with MPG 0-1, with regard to initial area at risk, amount of myocardium salvaged, infarct size and 5-year survival.
ABBREVIATIONS
CI: confidence interval
MPG: myocardial perfusion grade
PCI: percutaneous coronary intervention
STEMI: ST-segment elevation myocardial infarction
TIMI: Thrombolysis in Myocardial Infarction
SEE EDITORIAL ON PAGES 757-9
Correspondence: G. Ndrepepa, MD. Deutsches Herzzentrum,
Lazarettstrasse 36. 80636 München. Germany.
E-mail: ndrepepa@dhm.mhn.de
Received January 8, 2010.
Accepted for publication February 22, 2010.