Keywords
INTRODUCTION
Heart failure is a disease with a poor prognosis1-4 and its appearance frequently signals the final phase of many processes, one of the most prominent of which is ischemic heart disease. Mortality is comparable to that of the most common cancers, with <50% 4-year survival.5 Despite this, current advances in treatment have brought improved quality of life and survival to heart failure patients. However, improved survival and the many comorbidities6-8 are accompanied by additional health problems. Recent studies show that substantial number of heart failure patients die from processes other than cardiac disease, in particular malignancies, respiratory problems and septicemias.5,8-11 The present study aims to determine mortality and causes of death in an outpatient population with heart failure of various etiologies treated at a specialist multidisciplinary unit, and to analyze factors possibly associated with mortality and cause of death. A unit like ours facilitates analysis of data from these patients as it provides level of follow-up and genuine knowledge of treatment seldom found in the literature.
METHODS
Our heart failure unit is integrated into a tertiary hospital. Most patients are referred from cardiology (70.5%) and internal medicine (15.1%); 5% come from the emergency room/short-stay unit. Admissions from primary care clinics are few.
The principal criterion for referral for follow-up is heart failure as the principal problem, independently of the etiology. We also admit patients with severely depressed ventricular function following acute myocardial infarction (AMI). At first visit, patients give written consent to our obtaining analytic samples and using their clinical data for research purposes.
We follow a protocol of visits that includes a minimum of 3-monthly visits from a nurse and 6-monthly visits from the physician (cardiologist, internist, or family physician), and optional visits from specialists in geriatrics, psychiatry and rehabilitation. A computer database is completed with data on possible death and its likely cause. Patients are followed-up indefinitely, unless they decide otherwise or move to another healthcare area.
Survival status and cause of death are documented by reviewing clinical records, contacting family, carers or healthcare centers where patients may be hospitalized or, if contact is impossible, by reviewing the central registry of healthcare insurance policy-holders.
We enrolled all consecutive admissions between August 2001, when the unit opened, and December 31, 2008. Follow-up analysis was closed on June 10, 2009. During this period 26 944 visits were recorded.
Determination of Cause of Death
Patients were divided into 2 broad-ranging groups: cardiovascular death and non-cardiovascular death; patients who died of unknown causes were excluded. Cardiovascular causes were divided into: heart failure (decompensated heart failure or treatment-resistant heart failure, in the absence of another cause); sudden death (SD) (unexpected death, witnessed or not, of a previously stable patient with no evidence of worsening heart failure or any other cause of death); AMI (directly related in time with AMI, whether due to mechanic, hemodynamic or arrhythmic complications); stroke (associated with recently appearing acute neurologic deficit); procedural (post-diagnostic or post-therapeutic procedure death); and other cardiovascular causes (eg, rupture of an aneurysm, peripheral ischemia, or aortic dissection). Non-cardiovascular causes included: malignancies, respiratory infections, digestive infections (including hepatic and pancreatic infections), syndrome of decline (gradual appearance of dependence due to progressive deterioration of functional capacity, inexplicable weight loss or mental deterioration),12 and fracture of the femur (death due to complications following a fractured femur).
We determined clinical and demographic parameters associated with type of death (cardiovascular or non-cardiovascular). Finally, we also compared patients who died suddenly with deaths from any other cause.
Statistical Analysis
Statistical analysis was with SPSS 11.0 for Windows (SPSS Inc.). Statistical significance was established at P<.05. Continuous variables are expressed as mean (standard deviation [SD]) or median [interquartile range], according to whether or not distribution was normal; categorical variables are expressed as percentages. Analysis of mortality was with bivariate and multivariate Cox logistic regression (backward stepwise method). We compared causes of death according to variable type (dichotomous or continuous) and distribution (normal or not normal) using the appropriate tests (c2, Student t test, Mann-Whitney U test). Univariate and multivariate analysis was with logistical regression (backward stepwise method).
Our study complied with Helsinki Declaration principles and Spanish personal data protection law.
RESULTS
We studied 960 patients, 681 men and 279 women. Demographic and clinical characteristics are in Table 1. Median follow-up was 36 [16.6-64.5] (range, 0-95) months. Only 2 patients were lost during the follow-up, due to changes in their place of residence. These patients were included in the analysis as surviving up to the date when they left the healthcare area.
Mortality
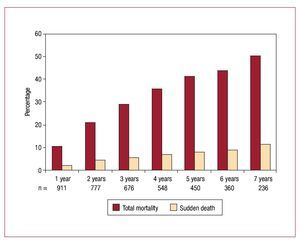
In the 7 years and 11 months of the study we recorded 351 deaths (36.6% mortality). Cumulative yearly mortality is in Figure 1 and ranges from 10.6% in year 1 to 50.8% in year 7. Median age at death was 75.2 [69.5-81.2] years. Median time lapse between diagnosis of heart failure and death was 62 [32.3-107.8] months. Table 1 compares characteristics of patients surviving at the end of the follow-up with those who died. Table 2 shows multivariate Cox regression analysis results.
Figure 1. Cumulative mortality and sudden death, by years of follow-up.
Causes of Death
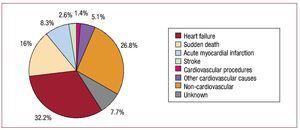
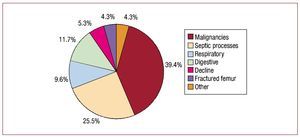
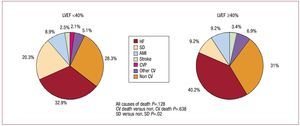
Figure 2 gives the different causes of death. We considered cardiovascular events caused 230 deaths (65.5% of the total). These were mainly due to progression of heart failure (113 patients, 32.2% of total deaths; 11.8% of the population studied); SD (56 patients, 16% of total deaths; 5.8% of the population studied). Note that 94 patients died of non-cardiovascular causes (26.8% of total deaths, 9.8% of the population studied). Figure 3 shows non-cardiovascular causes of death, among which malignancies and septic processes stand out (39.4% and 25.5% of non-CV deaths, respectively). Cause of death remained undetermined in 27 patients (7.7% of deaths). Figure 4 shows (known) causes of death as a function of LVEF <40% or ≥40%.
Figure 2. Causes of death.
Figure 3. Non-cardiovascular causes of death.
Figure 4. Causes of death as a function of left ventricular ejection fraction (LVEF). AMI indicates acute myocardial infarction; CV cardiovascular; CVP, cardiovascular procedures; HF, heart failure; SD, sudden death.
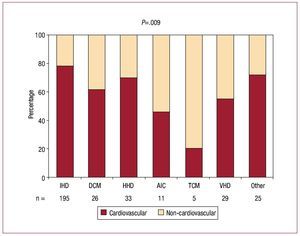
We divided patients in 2 groups by cause of death (cardiovascular and non-cardiovascular) and Table 3 shows the characteristics of both groups. A significant association with cardiovascular-cause death was only found for ischemic etiology of heart failure (P=.006 vs the sum of the other etiologies); a longer period of time since symptom onset (P=.045); treatment with nitrates (P=.024); and treatment with digoxin (P=.04). Patients who died of non-cardiovascular causes had lower body mass index (BMI) (P=.001). Figure 5 shows percentages of cardiovascular and non-cardiovascular deaths as a function of heart failure etiology. In multivariate analysis, ischemic etiology, treatment with digoxin, and BMI remained in the model.
Figure 5. Cardiovascular death and non-cardiovascular death by etiologies. AIC indicates alcohol-induced cardiomyopathy; DCM, dilated cardiomyopathy; HHD, hypertensive heart disease; IHD, ischemic heart disease; TCM, toxic cardiomyopathy (drugs); VHD, valvular heart disease.
Sudden Death
Occurrence of SD was 62.5% in the first 2 years follow-up and 80% in the first 3 years. Percentage of SD in relation with total mortality held reasonably constant over the years (Figure 1). We compared SD and non-SD deaths (Table 4) and found no factor determined SD, although patients with SD were somewhat younger at the time of death (73.5 vs 75.7 years; P=.026), had a slightly lower baseline LVEF (28% vs 31%; P=.049), and a somewhat smaller left atrium (LA) diameter (24.8 vs 26.7; P=.023). SD was more frequent in patients with LVEF <40% than in those with LVEF ≥40% (Figure 4). Deaths of patients with kidney failure were more frequently from other causes: SD, 13.2% of deaths, versus 29.4% in patients without kidney failure (P=.001). Patients receiving hydralazine showed the same tendency (P=.005). In multivariate analysis, LA diameter, hydralazine treatment and creatinine clearance rate remained in the model.
DISCUSSION
Although current therapeutic approaches to heart failure have improved prognosis, mortality remains high (36.6% in a median 3-year follow-up) even though we are managing patients in a special unit with a high number of visits (almost 27 000 in just under 8 years) and good compliance with recommended drug therapies. Mortality figures have been lower than some population-based studies,1-5 but higher than those of a contemporary Spanish outpatient study (MUSIC),13 which reported 26.9% mortality in 44 months follow-up. We consider it important to note that MUSIC patient characteristics differed from those in our series (MUSIC patients were younger [65 vs 69 years], in a better functional class [78.4% in class II vs 55%], with better LVEF [37% vs 31%], lower incidence of kidney failure [46.2% vs 53.3%] and of ischemic etiology [45.7% vs 55.4%]); these factors could explain differences in mortality. In any case, annual mortality was around 7.1%, approximately 10% annually in the first 3 years, with an additional 5% in the following years, a figure possibly congruent with the positive impact that heart failure unit-programs have been shown to have on prognosis of this syndrome.14-16 The benefits these unit-programs provide to prognosis is probably based on the higher level of compliance with therapeutic guidelines, educational interventions with stimuli to promote self-care, and the multidisciplinary approach; all aspects which have received special attention in our population. Moreover, we would emphasize that most of our patients have continued receiving specific attention in the unit throughout the study period. This may be important, as the benefits of a specialized intervention has been seen to be lost in time after it has been suspended.16 Nonetheless, mortality was similar, although the follow-up was slightly shorter (3 vs 3.7 years), to that reported in another Spanish study by Grigorian-Shamagian et al17 (37.7%) of a series of patients discharged from a cardiology service after admission for heart failure.
We had previously investigated the prognostic value of some clinical and echocardiographic parameters analyzing mortality in fixed periods (1-2 years), and finding that parameters like plasma hemoglobin,18 diabetes mellitus,19 body mass index,20 creatinine clearance rate,21,22 fragility,23 or LA diameter24 proved very significant short- and mid-term prognostic factors. The current series is more extensive, and with a longer, although more heterogeneous, follow-up. Multivariate Cox regression analysis (Table 2) enables us to generate a profile of the patient with increased risk of any cause mortality at admission to the unit, although we did not intend to construct a risk score like that used in other studies.13 Our profile describes an older patient, a man, for whom a longer period has elapsed since the onset of symptoms of heart failure, of ischemic etiology, who is in a worse functional class, with worse LVEF, diabetes mellitus, kidney failure, peripheral vascular disease, and fragility, and who does not or cannot take beta-blockers, angiotensin converting enzyme inhibitors or angiotensin II receptor blockers, statins or antiplatelet agents. Differences in results between our previous studies and the current one may be explained by the more extensive nature of the present series and the longer and more heterogeneous follow-up, and the statistical analyses performed. Unlike other series, we preferred to include in this study the treatment administered during follow-up, and not the treatment patients were following at inclusion or discharge, since we believe it has a fundamental role in prognosis. The MUSIC13 study mentioned patients' baseline treatment but did not include it in risk score construction. Grigorian-Shamagian et al17 comment on in-hospital treatment but not follow-up treatment. Their study was an in-hospital series, with a significant number of patients with conserved LVEF, which probably explains why the percentage of patients administered beta blockers was much lower than in our population.
In bivariate analysis, gender, LVEF and ischemic etiology showed no association with mortality. However, they were included in multivariate analysis due to their clinical importance, and showed a statistically significant association. The opposite happens with hydralazine, nitrates and diuretics, which are probably associated with worse functional situation and kidney failure. A history of hypercholesterolemia deserves separate comment as it is statistically associated with improved survival (P=.013), although it loses its statistical significance in multivariate analysis. This observation may be related with the benefit observed from statin administration, which remains an independent prognostic factor in multivariate analysis. We find no plausible explanation for this, although possible beneficial effects in preventing AMI or stroke or perhaps an anti-inflammatory effect (cytokines) could have participated, but this remains mere speculation. We should remember that the CORONA25 and GISSI-HF26 studies show no benefits from rosuvastatin administration on mortality of heart failure patients.
Non-Cardiovascular Mortality
One significant finding of our study is the considerable percentage of deaths from non-cardiovascular causes (26.8% of the total, 9.8% of the population studied) that could be explained by several factors: high patient comorbidity, optimal drug and non-drug treatment in a specialized unit, the greater access these units afford to patients with decompensation, or administration of intravenous treatments in outpatient contexts in initial phases of decompensation. This has already been reported elsewhere.5,8-11 In comparison with the MUSIC study,13 we found a greater percentage of non-cardiovascular deaths (MUSIC, 20.2% of total deaths, 5.4% of the population studied), probably related with the age and comorbidities of our patients, too. This percentage was higher than that observed by Grigorian-Shamagian et al,17 too (16.7% of known-cause deaths, approximately 6.9% of the total with known survival status). In contrast, the percentage of non-cardiovascular deaths is much lower than that in some recent population-wide series.5 (43% at 5 years). In this series, the percentage of deaths due to heart failure is not reported and causes of death are only divided into non-cardiovascular, due to ischemic heart disease and other cardiovascular causes. Moreover, it is striking that non-cardiovascular cause deaths should reach 49% in patients with conserved LVEF, and that this should be the first cause of death. In any case, the populations differ (our patients are younger and probably have more serious cardiomyopathies). Unlike our series, the principal cause of non-cardiovascular death was respiratory disease (vs malignancies).5 In our series, the percentage of non-cardiovascular death was somewhat greater in patients with EF ≥40%, but the differences were not significant. This resembles Grigorian-Shamagian et al's findings17 in patients with EF ≥50%. Neither MUSIC13 nor Grigorian-Shamagian17 specify non-cardiovascular causes of death. The factors significantly associated with death from cardiovascular causes were ischemic etiology of heart failure, a longer period since the onset of symptoms, treatment with nitrates (probably in relation with the etiology) and treatment with digoxin (probably associated with a worse functional situation). In contrast, the toxic drug etiology associated with a very low percentage of cardiovascular death. Although patients with fragility showed a greater tendency to die from a non-cardiovascular cause (57.4% vs 45.6%), this difference was an outlier in terms of statistical significance (P=.054). Patients with heart failure are often fragile and their care should not be limited exclusively to the cardiovascular context. The promotion of a multidisciplinary approach permits early detection and management of other health problems and can produce greater benefits in the morbidity and mortality of this syndrome. The creation of heart failure units in hospitals and their collaboration with basic primary healthcare areas should contribute to improving the quality of attention and extend this to the general population.
Sudden Death
Another noteworthy finding of the present study is the relatively low incidence of SD: only 5.8% of the total population studied. This coincides quite closely with MUSIC data,13 although they report 9.1% SD in the population analyzed, and with Grigorian-Shamagian et al17 (6.9% of the total population with known survival status). This indicates the impact of SD in our context is much lower than that described in the English-speaking world.27,28 Furthermore, the incidence of SD was mainly in the first years of follow-up. Although patients with SD were somewhat younger when they died, had a slightly lower baseline LVEF, and somewhat smaller LA diameter, we cannot define any single factor as clearly determinant, although the percentage of SD was higher in patients with LVEF <40%.
Limitations
In patients for whom we had no medical or healthcare report, we accepted the cause of death reported by family or carers. In patients with malignancies, infection and other non-cardiovascular causes of death this information is likely to be accurate. Cataloguing some causes of cardiovascular death may be more difficult. We believe an individual, isolated error will have had no influence on the general results of our study. In fact, when official medical certificates have been used in other studies, cause of death often remains dubious. Moreover, cause of death can be difficult to determine, even when it occurs in the hospital. Generally, this is because of the confluence of many pathologic situations at the time of death, derived from the high number of comorbidities. Although we have access to NT-proBNP data for 190 patients, we have not included it in the analysis due to the large number of patients for whom the data is unavailable. Similarly, we have no troponin I data. Although ours is a general population with heart failure, of varied etiology, and heterogeneous in some aspects, it remains a selection of the total population of patients with heart failure, since most come from a cardiology service and it is a relatively young population, with few women and fundamentally ischemic etiology. Therefore, the results obtained cannot necessarily be generalized to the heart failure population at large.
CONCLUSIONS
Although total mortality of patients attended in a specialized heart failure unit may not be considered low, despite close follow-up and adequate treatment following established guidelines, one in four died of non-cardiovascular causes. The principal factor associated with cardiovascular death was ischemic etiology of heart failure. Sudden death represented only 5.8% of the total of patients, with no clearly associated determinant factor, although it was more frequent in patients with LVEF <40%.
ABBREVIATIONS
AMI: acute myocardial infarction
IQR: interquartile range
LA: left atrium
LVEF: left ventricular ejection fraction
SD: sudden death
Correspondence: Dr. J. Lupón Rosés.
Unitat d'Insuficiència Cardíaca.
Hospital Universitari Germans Trias i Pujol.
Ctra. del Canyet, s/n. 08916 Badalona. Barcelona. Spain.
E-mail: jlupon.germanstrias@gencat.cat
Received September 7, 2009.
Accepted November 25, 2009.