Mitral regurgitation (MR) is a frequent disease (2 million people in the United States) increasing with population aging and associated with a poor prognosis.1 Mitral valve reconstruction described by Carpentier 40 years ago2 is now considered as the gold standard for surgical treatment of MR. The golden rules of Carpentier's techniques are based upon 3 basic principles: preserve or restore full leaflet motion, create a large surface of coaptation, remodel and stabilize the entire annulus. In today's conditions, the aim of the surgeon is no longer to correct a regurgitation but to treat a patient for the rest of his or her life and restore a life expectancy similar to the normal population.3 However, even if almost all degenerative MR can be repaired, in the “real world” mitral repair is only performed in 40% to 50% of cases.4 How to improve this rate? One part of the solution is to build a team with an echocardiographist (cardiologist or anesthesiologist), always the same and available when needed, using a dedicated machine in the operating room with real time three-dimensional (3D) imaging if possible, and speaking a common language, with mutual respect and honesty: the exact definition of your best friend!
The echocardiographist has 2 main roles in the field of mitral repair:
• Guide surgical procedure, determining appropriate timing of surgery based on 3 echo triggers: severity of MR, left ventricular (LV) function and dimensions, and mechanism (dysfunction). This provides a road map, a surgical GPS.
• Evaluate intraoperatively the immediate functional result to achieve a perfect repair and as a safety net to avoid reoperation. Intraoperative transesophageal echocardiography (TEE) has to be systematic for all mitral repairs.
Echocardiography provides three essential findings for surgical indications based on international guidelines:5, 6
• Severity of MR.
• LV function and dimensions.
• Likelihood of repair, which depends on valve analysis by echocardiography but mostly on the surgeon's skill and experience.
These findings are usually obtained by preoperative transthoracic echocardiography or TEE if the patient has poor echogenicity or if MR is due to endocarditis. However, pre-pump intra-op two dimensional (2D) or 3DI TEE is mandatory and must be discussed with the echocardiographist immediately before surgery.
Severity of Mitral RegurgitationQuantitative Doppler grading of MR is preferred and is based on the calculation with the proximal isovelocity surface area method of regurgitant volume (yealding volume overload) and effective regurgitant orifice (lesion severity); when using color flow, another important criteria is the width of vena contracta (narrowest portion of the jet). The clinician must separate the criteria used to define a severe degenerative or organic MR from those used for ischemic/functional MR (Table 1).
Table 1. Echo Criteria of a Severe Mitral Regurgitation.
| Organic (degenerative) | Ischemic or functional | |
| Effective regurgitant orifice | 40mm2 | 20mm2 |
| Regurgitant volume | 60ml per beat | 30ml per beat |
| Vena contracta | 7 mm | 4 mm |
It is essential to keep in mind the correlation between MR severity and prognosis: patients >50 years with severe organic MR (effective regurgitant orifice [ERO] >40mm2) are at increased risk of mortality (yearly rate of 6%); interestingly, a recent paper7 underlines the adverse prognosis of less than severe MR, showing that during follow up (mean 8.6 years) 52% of patients developed either MR worsening or de novo LV dysfunction. The authors advocate for revisiting guidelines and identify earlier triggers for surgical consideration.
Patients with ischemic MR and an ERO >20 mm2 have an approximately 2-fold increase in mortality risk and 4-fold increase in the risk of heart failure compared to those with a similar ischemic LV dysfunction but no MR.
Left Ventricular Function and DimensionsWe know that ejection fraction (EF) is an imperfect criterion with severe MR (overestimated). However, this is the main criteria used in publications: patients with overt preoperative LV dysfunction have an increased postoperative mortality, especially with EF<50%. Generally, there is a 10% early postoperative reduction in EF. However, 25% to 30% of patients with MR have postoperative LV dysfunction, particularly those with preoperative EF <60% or end-systolic diameter (ESD) of at least 40mm to 45mm. A recent publication underlines the ESD trigger,8 showing that ESD ≥40mm is independently associated with increased overall mortality (hazard ratio, 1.86) under medical management and after surgery.
The main goal for clinicians is to detect LV enlargement and/or dysfunction earlier by echocardiography and send patients to a surgeon with special expertise on mitral repair in order to have the best chance of improving LV function and survival after surgery and avoid contributing to the important and unacceptable proportion of patients (49%) with severe symptomatic MR not referred to surgeons because of severe LV dysfunction.9 It is also known that patients even with normal EF have structural dysfunction (increased oxidative stress and cardiomyocyte myofibrillar degeneration) detected by histology.10 This is why we advocate for early surgery in degenerative MR, even in asymptomatic patients operated in advanced repair centers with low operative mortality (<1%) and high repair rates (> 80%-90%) with systematic intra-operative TEE to avoid residual MR.11, 12
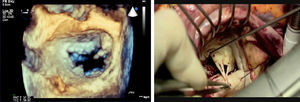
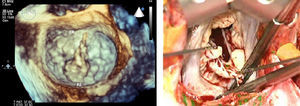
Likelihood of Repair and Echo Valve Analysis 13Valve analysis is essential to determine feasibility of repair with the surgeon's skill and expertise. It requires a team effort with a common language based upon the pathophysiological triad and the functional approach. There has to be a clear distinction in echo report between etiology (ie, cause of the disease), lesions (ie, result from the disease) and dysfunction (ie, result from lesions). Dysfunction is an essential element because it is the basic principle of the functional approach that permits simplified decision making and it is well assessed by echocardiography because it is based upon leaflet motion (type I: normal, type II excessive or prolapse, type III restrictive in diastole IIIa, or in systole IIIb). The echocardiographist also has the duty to localize the dysfunction (segmental analysis) in order to determine which scallop is involved. 2D echocardiography is appropriate to define the type of dysfunction. 2D but overall real time 3D TEE is a spectacular tool to determine segmental analysis, particularly for commissural prolapse (Figure 1). For the frequent P2 prolapse, 3D echo permits evaluating the width of prolapse and the extension to the indentations (Figure 2).
Figure 1. Posterior commisural prolapse. Left, real-time three-dimensional transesophageal echocardiography; right, surgical view.
Figure 2. P2 prolapse. Left, real-time three-dimensional transesophageal echocardiography; right, surgical view.
The main goal and objective of the surgeon planning a valve repair is to correct the dysfunction. Echocardiography is not the best tool to diagnose lesions such as chordal rupture or elongation; in fact, chordal elongation is often undiagnosed. Lesional analysis is well evaluated visually by the surgeon. This analysis is essential to choose the appropriate techniques according to Carpentier's “one lesion one technique” principle.
The following measurements must also be made:
• Height of A2, which correlates with ring size and etiology (>34mm for Barlow)
• Tricuspid annulus diameter in diastole to determine if tricuspid repair will be necessary (above 40mm).
According to the extent of dysfunction (localized or extensive prolapse) the surgeon can evaluate the difficulty of repair based upon his or her own skill and experience.
A TOOL TO EVALUATE REPAIR RESULTIntraoperative TEE is mandatory for all mitral valve repairs. It permits evaluation of immediate functional results: residual MR, reoperation factors, systolic anterior motion, and other complications such as LV dysfunction, circumflex injury, aortic cusp stitch, or atrial septal defect.
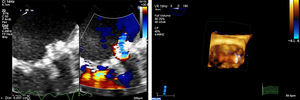
Residual MR is an unacceptable result except for mild and central regurgitation due to leaflet irregularities. Beyond severity, the objective of the echo is to determine the precise mechanism and particularly to identify leaflet jet and segmental analysis; real time 3D color TEE has a clear superiority over 2D analysis for this purpose (Figure 3).
Figure 3. Intra-operative residual mitral regurgitation. Left, two-dimensional color view; right, three-dimensional color view.
In systolic anterior motion, echocardiography determines if there is a need to fill the heart, stop the drugs, and measure the height of the posterior and anterior leaflets (if the ring is too small).
In conclusion, the echocardiographist is the best friend of the surgeon involved in mitral repair but also of the patient, helping to choose the appropriate timing of surgery, predict the techniques to be used, and intra-operatively monitor the result in order to avoid reoperation. You can’t expect more from your best friend!
Conflicts of interestDr. Berrebi is a consultant to Edwards Lifesciences and Philips Healthcare.
Corresponding author: Service de Chirurgie Cardio-Vasculaire, Hôpital Européen Georges Pompidou, 20 rue Leblanc, 75015 Paris, France. alainberrebi@hotmail.com