To investigate possible age-related differences in the profile, clinical symptoms, management, and short-term outcomes of patients seen for acute heart failure in Spanish emergency departments.
MethodsWe performed a multipurpose, multicenter study with prospective follow-up including all patients with acute heart failure attended in 29 Spanish emergency departments. The following variables were collected: demographic, personal history, geriatric syndromes, data of acute episode, discharge destination, in-hospital and 30-day mortality and 30-day revisit. The sample was divided into 4 age groups: <65, 65-74, 75-84, and ≥85 years.
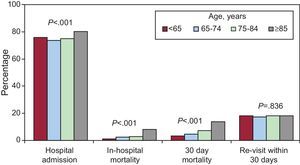
ResultsWe included 5819 patients: 493 (8.5%) were <65 years old, 971 (16.7%) were 65-74 years old, 2407 (41.4%) were 75-84 years old, and 1948 (33.5%) were ≥85 years old; 4424 patients (76.5%) were admitted from the emergency department, 251 of whom (4.5%) died during hospitalization. Statistically significant differences were observed in relation to cardiovascular risk factors, comorbidities, geriatric syndromes, clinical presentation, and diagnostic and therapeutic procedures based on an increase in the age of the groups. A statistically significant linear trend was observed between age group and the probability of hospital admission (P<.001), and hospital (P<.001) and 30-day mortality (P<.001).
ConclusionsThe management of acute heart failure in elderly patients requires a multidimensional approach which goes beyond merely cardiological aspects of treatment.
Keywords
.
INTRODUCTIONPopulation aging has a number of socio-economic consequences that require active aging policies aimed at improving quality of life in the elderly.1 Acute disease and, more frequently, exacerbation of chronic diseases can trigger a dependence cascade.2
Acute heart failure (AHF) is a highly prevalent condition which is directly related to age and is a frequent cause of visits to emergency departments (ED), as well as admissions and re-admissions.3,4 It is associated with high morbidity and mortality as well as with functional deterioration.5 This makes the ED a key stage in treatment, as its immediate management can influence overall and functional prognosis in the short term. Physiological changes associated with aging and the greater likelihood of comorbidities and polymedication2 make it necessary to take age into account during evaluation and urgent decision making.
Before developing strategies aimed at improving the outcomes of emergency treatment in this age group, it is essential to find out more about the local context. The literature addressing how changes associated with aging are dealt with in the clinical context or in terms of guideline implementation has focused on inpatient or outpatient settings, with little attention paid to ED, even though over a quarter of patients seen for AHF in ED are discharged directly from the ED.6 In light of this lack of information, the main objective of the present study was to determine whether there are differences by age in the profile, clinical presentation, management and short-term outcomes of patients treated for AHF in Spanish EDs.
METHODSStudy DesignMultipurpose, multicenter, non-interventional cohort study in which patients with AHF treated in 29 Spanish EAHFE (Epidemiology Acute Heart Failure Emergency) participating in the EAHFE registry were prospectively followed up.
Patient SelectionThe cohort of patients was drawn from the EAHFE registry and included all consecutive patients treated for an episode of AHF over one month periods in 2007 (948 from EAHFE-1) and 2009 (1483 from EAHFE-2) and over a two month period in 2011 (3414 from EAHFE-3). A total of 29 Spanish EDs participated in the registry, which included 5845 consecutive patients seen for AHF. The Framingham criteria6 were used to define AHF. For the present study, patients for whom date of birth or more than 10% of all study variables were missing were excluded.
Study VariablesData was collected on demographic information, medical history, geriatric syndromes, clinical manifestations of the acute episode, the results of certain tests (B-type natriuretic peptide assay, troponin plasma assay, and urgent echocardiography) and consultations with the cardiology specialist in the ED, immediate drug treatment, final destination after emergency care (admission or discharge) and outcome during hospitalization (hospital mortality) and 30 days following the index episode in the ED (mortality and revisits).
Statistical AnalysisQualitative variables are shown by frequency distributions. Quantitative variables with a normal distribution are summarised as mean (standard deviation) or median [interquartile range]. The chi-square test was used or Fisher's exact test when more than 25% of the expected frequencies were <5; P for linear trend was also estimated. The sample was split into 4 groups by age (<65, 65-74,75-84 and ≥85 years). Data analysis was performed using SPSS software, version 18.0.
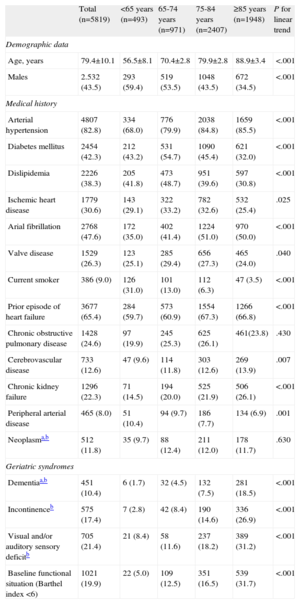
RESULTSA total of 5819 patients were included (99.5% of the total in the EAHFE registry). Mean age was 79.4 (10.1) years and 2532 (43.5%) were male; 493 (8.5%) were under 65 years, 971 (16.7%) 65-74, 2407 (41.4%) 75-84, and 1948 (33.5%) were 85 years or older (Table 1).
Baseline Characteristics of Patients Included in the Study, by Age Group
| Total (n=5819) | <65 years (n=493) | 65-74 years (n=971) | 75-84 years (n=2407) | ≥85 years (n=1948) | P for linear trend | |
| Demographic data | ||||||
| Age, years | 79.4±10.1 | 56.5±8.1 | 70.4±2.8 | 79.9±2.8 | 88.9±3.4 | <.001 |
| Males | 2.532 (43.5) | 293 (59.4) | 519 (53.5) | 1048 (43.5) | 672 (34.5) | <.001 |
| Medical history | ||||||
| Arterial hypertension | 4807 (82.8) | 334 (68.0) | 776 (79.9) | 2038 (84.8) | 1659 (85.5) | <.001 |
| Diabetes mellitus | 2454 (42.3) | 212 (43.2) | 531 (54.7) | 1090 (45.4) | 621 (32.0) | <.001 |
| Dislipidemia | 2226 (38.3) | 205 (41.8) | 473 (48.7) | 951 (39.6) | 597 (30.8) | <.001 |
| Ischemic heart disease | 1779 (30.6) | 143 (29.1) | 322 (33.2) | 782 (32.6) | 532 (25.4) | .025 |
| Arial fibrillation | 2768 (47.6) | 172 (35.0) | 402 (41.4) | 1224 (51.0) | 970 (50.0) | <.001 |
| Valve disease | 1529 (26.3) | 123 (25.1) | 285 (29.4) | 656 (27.3) | 465 (24.0) | .040 |
| Current smoker | 386 (9.0) | 126 (31.0) | 101 (13.0) | 112 (6.3) | 47 (3.5) | <.001 |
| Prior episode of heart failure | 3677 (65.4) | 284 (59.7) | 573 (60.9) | 1554 (67.3) | 1266 (66.8) | <.001 |
| Chronic obstructive pulmonary disease | 1428 (24.6) | 97 (19.9) | 245 (25.3) | 625 (26.1) | 461(23.8) | .430 |
| Cerebrovascular disease | 733 (12.6) | 47 (9.6) | 114 (11.8) | 303 (12.6) | 269 (13.9) | .007 |
| Chronic kidney failure | 1296 (22.3) | 71 (14.5) | 194 (20.0) | 525 (21.9) | 506 (26.1) | <.001 |
| Peripheral arterial disease | 465 (8.0) | 51 (10.4) | 94 (9.7) | 186 (7.7) | 134 (6.9) | .001 |
| Neoplasma,b | 512 (11.8) | 35 (9.7) | 88 (12.4) | 211 (12.0) | 178 (11.7) | .630 |
| Geriatric syndromes | ||||||
| Dementiaa,b | 451 (10.4) | 6 (1.7) | 32 (4.5) | 132 (7.5) | 281 (18.5) | <.001 |
| Incontinenceb | 575 (17.4) | 7 (2.8) | 42 (8.4) | 190 (14.6) | 336 (26.9) | <.001 |
| Visual and/or auditory sensory deficitb | 705 (21.4) | 21 (8.4) | 58 (11.6) | 237 (18.2) | 389 (31.2) | <.001 |
| Baseline functional situation (Barthel index <6) | 1021 (19.9) | 22 (5.0) | 109 (12.5) | 351 (16.5) | 539 (31.7) | <.001 |
Data are expressed as n. (%) or mean±standard deviation.
Regarding the relationship between cardiovascular risk factors and age groups, there was a significant increase in blood pressure (P<.001), atrial fibrillation (P<.001) and previous episode of decompensated heart failure (HF) (P<.001) as age increased. Conversely, there was a progressive decrease in diabetes mellitus (P<.001), dyslipidemia (P<.001), current smoking (P<.001), ischemic heart disease (P=.025), peripheral arterial disease (P=.001) and valvular disease (P=.040) (Table 1).
Regarding comorbidity and geriatric syndromes, we observed a significant increase in the frequency of stroke (P<.001), chronic renal failure (P<.001), dementia (P<.001), urinary incontinence (P<.001), sensory deficits (P<.001), and severe baseline functional dependence (P<0.001) as age increased (Table 1).
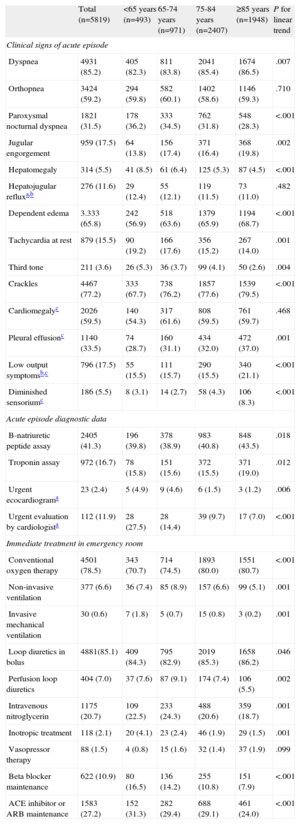
Statistically significant differences by age were also found in terms of diagnostic clinical signs. As age increased, there was a higher percentage of patients with dyspnea (P=.007), jugular venous distention (P=.002), pulmonary rales (P<.001), pleural effusion (P=.001), edema (P<.001), symptoms of low cardiac output (P<.001), and decreased sensorium (P<.001). By contrast, as age decreased the frequency of paroxysmal nocturnal dyspnea (P<.001), hepatomegaly (P<.001), tachycardia at rest (P=.001), and third heart sound (P=.004) increased (Table 2).
Clinical, Diagnostic, and Treatment Data for Patients Included in the Study, by Age Group
| Total (n=5819) | <65 years (n=493) | 65-74 years (n=971) | 75-84 years (n=2407) | ≥85 years (n=1948) | P for linear trend | |
| Clinical signs of acute episode | ||||||
| Dyspnea | 4931 (85.2) | 405 (82.3) | 811 (83.8) | 2041 (85.4) | 1674 (86.5) | .007 |
| Orthopnea | 3424 (59.2) | 294 (59.8) | 582 (60.1) | 1402 (58.6) | 1146 (59.3) | .710 |
| Paroxysmal nocturnal dyspnea | 1821 (31.5) | 178 (36.2) | 333 (34.5) | 762 (31.8) | 548 (28.3) | <.001 |
| Jugular engorgement | 959 (17.5) | 64 (13.8) | 156 (17.4) | 371 (16.4) | 368 (19.8) | .002 |
| Hepatomegaly | 314 (5.5) | 41 (8.5) | 61 (6.4) | 125 (5.3) | 87 (4.5) | <.001 |
| Hepatojugular refluxa,b | 276 (11.6) | 29 (12.4) | 55 (12.1) | 119 (11.5) | 73 (11.0) | .482 |
| Dependent edema | 3.333 (65.8) | 242 (56.9) | 518 (63.6) | 1379 (65.9) | 1194 (68.7) | <.001 |
| Tachycardia at rest | 879 (15.5) | 90 (19.2) | 166 (17.6) | 356 (15.2) | 267 (14.0) | .001 |
| Third tone | 211 (3.6) | 26 (5.3) | 36 (3.7) | 99 (4.1) | 50 (2.6) | .004 |
| Crackles | 4467 (77.2) | 333 (67.7) | 738 (76.2) | 1857 (77.6) | 1539 (79.5) | <.001 |
| Cardiomegalyc | 2026 (59.5) | 140 (54.3) | 317 (61.6) | 808 (59.5) | 761 (59.7) | .468 |
| Pleural effusionc | 1140 (33.5) | 74 (28.7) | 160 (31.1) | 434 (32.0) | 472 (37.0) | .001 |
| Low output symptomsb,c | 796 (17.5) | 55 (15.5) | 111 (15.7) | 290 (15.5) | 340 (21.1) | <.001 |
| Diminished sensoriumc | 186 (5.5) | 8 (3.1) | 14 (2.7) | 58 (4.3) | 106 (8.3) | <.001 |
| Acute episode diagnostic data | ||||||
| B-natriuretic peptide assay | 2405 (41.3) | 196 (39.8) | 378 (38.9) | 983 (40.8) | 848 (43.5) | .018 |
| Troponin assay | 972 (16.7) | 78 (15.8) | 151 (15.6) | 372 (15.5) | 371 (19.0) | .012 |
| Urgent ecocardiograma | 23 (2.4) | 5 (4.9) | 9 (4.6) | 6 (1.5) | 3 (1.2) | .006 |
| Urgent evaluation by cardiologista | 112 (11.9) | 28 (27.5) | 28 (14.4) | 39 (9.7) | 17 (7.0) | <.001 |
| Immediate treatment in emergency room | ||||||
| Conventional oxygen therapy | 4501 (78.5) | 343 (70.7) | 714 (74.5) | 1893 (80.0) | 1551 (80.7) | <.001 |
| Non-invasive ventilation | 377 (6.6) | 36 (7.4) | 85 (8.9) | 157 (6.6) | 99 (5.1) | .001 |
| Invasive mechanical ventilation | 30 (0.6) | 7 (1.8) | 5 (0.7) | 15 (0.8) | 3 (0.2) | .001 |
| Loop diuretics in bolus | 4881(85.1) | 409 (84.3) | 795 (82.9) | 2019 (85.3) | 1658 (86.2) | .046 |
| Perfusion loop diuretics | 404 (7.0) | 37 (7.6) | 87 (9.1) | 174 (7.4) | 106 (5.5) | .002 |
| Intravenous nitroglycerin | 1175 (20.7) | 109 (22.5) | 233 (24.3) | 488 (20.6) | 359 (18.7) | .001 |
| Inotropic treatment | 118 (2.1) | 20 (4.1) | 23 (2.4) | 46 (1.9) | 29 (1.5) | .001 |
| Vasopressor therapy | 88 (1.5) | 4 (0.8) | 15 (1.6) | 32 (1.4) | 37 (1.9) | .099 |
| Beta blocker maintenance | 622 (10.9) | 80 (16.5) | 136 (14.2) | 255 (10.8) | 151 (7.9) | <.001 |
| ACE inhibitor or ARB maintenance | 1583 (27.2) | 152 (31.3) | 282 (29.4) | 688 (29.1) | 461 (24.0) | <.001 |
ACE, angiotensin converting enzyme; ARB, angiotensin receptor blockers.
Values are expressed as n. (%).
Among the diagnostic procedures performed in the emergency room, there was a significant age-associated increase in requests for B-type natriuretic peptide (P=.018) and plasma troponin (P=.012) assays. Emergency physician requests for urgent assessment by the attending cardiologist (P<.001) or echocardiography in the ED (P=.006) were inversely related to age and statistically significant (Table 2).
Regarding immediate treatment, as age increased there was greater use of oxygen (P<.001) and loop diuretics administered via intravenous bolus (P=.046) and less use of non-invasive (P=.001) and invasive (P=0.001) mechanical ventilation, continuous infusion loop diuretics (P=.002), intravenous nitroglycerin (P=.001), inotropic therapy (P=.001) and maintenance treatment with beta blockers (BB) (P<.001), angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB) (P<.001) (Table 2).
A total of 4424 patients were admitted from the ED (76.5%), of which 251 (4.5%) died during hospitalization. During the 30-day follow-up, 489 (8.8%) patients died and 888 (18%) reconsulted at the ED for any reason. We found a statistically significant linear trend between age group and the likelihood of hospitalization (P<.001) and death both during hospitalization (P<.001) and at 30 days follow-up (P<.001). In contrast, the probability of a revisit to the ED was similar between the different age groups (Figure).
DISCUSSIONIn our view, the main interest of this study lies in the fact that it has shown age to be a relevant factor in the profile and management of AHF patients treated in the emergency room and that it has done so in a very large sample of subjects with AHF from a large number of Spanish EDs. These differences by age could affect outcomes both during hospitalization and in the short term. The study also provides information on the process of care in the ED for elderly patients with AHF, which can be useful when designing an individualized care plan and in managing social welfare resources.
AHF was found to be a very common condition in the elderly (3 out of 4 patients were aged over 75 years). This may be due to the high population prevalence and incidence rates for HF, rates which double with each decade of life from 45 years on as a result of the changes associated with aging and increased survival in diseases which generate the syndrome.7 A population study in over 7000 patients with chronic HF who were followed for three years found that 1/10 patients had been admitted because of the disease.8 Likewise, almost two-thirds of episodes requiring hospitalization occur in patients over 70 years of age.3
Our data seem to define two clear, age-based cardiovascular risk factor profiles, with hypertension and atrial fibrillation being the more common risk factors in the longer-lived groups, while dyslipidemia, diabetes mellitus, and current smoking are more common in younger groups. This is probably reflected in the rates of ischemic heart disease and peripheral arterial disease found in the younger population. These data are consistent with those from a study of more than 200 000 HF patients, which showed a decreasing prevalence of diabetes mellitus and ischemic heart disease with age, but increasing rates of atrial fibrillation.9 These results provide an insight into the different pathophysiological mechanisms leading to AHF in different age groups. In older age groups, AHF may be the result of a series of physiological changes associated with aging, whereby the loss of functional reserve means that ever decreasing stimuli will lead to decompensation; this contrasts with the development of AHF from non-heart-healthy lifestyles and diseases seen in younger populations.10 These age-related changes also underlie the higher frequency of systolic hypertension, atrial fibrillation and AHF with preserved systolic function described in the oldest age groups10 and the possibly multifactorial etiology.11
Of note is the rise in comorbidity patients’ age increases and the presence of markers of frailty such as dementia, incontinence, sensory deficit and severe baseline functional dependence, particularly in the population aged 85 years or over. These data are consistent with previous studies which documented an increase in the degree of comorbidity with advancing age, an increase which is greater in non-heart related diseases.9 Other studies12 have confirmed that over three quarters of elderly patients with HF have three or more comorbidities and half have over five and that the percentage of patients with five or more comorbidities has increased over time (from 42% to 58%) in parallel with the average number of drugs prescribed (4.1 to 6.4).13 This increases the risk of adverse reactions and reduces safety in the ED.14 Furthermore, the degree of comorbidity has been shown to be correlated with increased mortality and short-term re-admission during the acute episode9 as well as with an increased use of hospital resources for patients with chronic HF.12 Other non-cardiac diseases and the presence of markers of frailty, which are more likely in patients 85 years or older, have been reported to be factors for a poor prognosis in patients with AHF.5,15 These factors may therefore be equally or more important in the evolution of the AHF than heart disease itself and may affect short term outcomes.
The frequency of symptoms and signs that orient the diagnosis of AHF in the emergency room also differ by age group. In older patients, findings are more likely to be those related to pulmonary congestion and low cardiac output, such as poorer mental status. Diagnostic difficulty increases, as signs are frequently less specific (e.g. edema) and reproducible (e.g. elevated jugular venous pressure) while typical (e.g. paroxysmal nocturnal dyspnea) and specific (e.g. third tone) signs appear less frequently.16 Increasing age therefore makes the clinical diagnosis of AHF more complex due to the frequent presence of atypical features, the interference of symptoms deriving from associated processes, the increased difficulty of interpreting the results of the physical examination and the tendency to attribute to age certain symptoms resulting from the impact at a distance of anterograde HF.17
With respect to urgent diagnostic tests, we found that there were proportionally more requests for B-type natriuretic peptide and troponin plasma assays in older age groups, a finding which can be justified by the greater difficulty involved in diagnosis and decision-making in older patients.18–21 On the other hand, we found a progressive age-related decline in requests for urgent cardiac evaluation, which may limit access to certain diagnostic and therapeutic procedures such as echocardiography in the emergency room, and the place of admission. These data corroborate previous findings that age is associated with a lower number of echocardiographic studies in patients with HF22 and which indicate some age-based discrimination.
In terms of drug treatment, older patients were less likely to receive loop diuretics by continuous infusion, intravenous nitroglycerin, inotropics and invasive and noninvasive mechanical ventilation, and treatment with BBs, ACE inhibitors or ARBs was less likely to be maintained. At the same time, prescription of bolus diuretics and oxygen therapy increased. These results underline the fact that age is associated with a decreased use of the pharmacologic and non-pharmacologic measures recommended by clinical guidelines, when they do not explicitly mention patient age,16 which may affect short-term outcomes.23
Despite recent published data on the efficacy and safety of loop diuretics regardless of the dosage form,24 an increasing amount of data points to the greater safety of diuretics in perfusion.25 This needs to be taken into account in a segment of population whose glomerular filtration rate is deteriorating and which has a higher prevalence of chronic renal failure and diuretic resistance. Intravenous nitroglycerin has shown positive hemodynamic properties and reduces the rate of procedures26 as well as the need for furosemide,27 which would reduce the likelihood of side effects associated with diuretics, especially in a group as vulnerable as the elderly. On the other hand, according to a meta-analysis of data from 5840 patients, treatment with levosimendan appears to have a beneficial effect on mortality compared with placebo and with dobutamine.28 The proportion of patients receiving these drugs, particularly levosimendan, decreases with age, regardless of clinical status and degree of ventricular function.29,30 Noninvasive ventilation, despite the current controversy over its effect on hospital mortality,31,32 is a non-pharmacological treatment which is effective in some patients regardless of age. Finally, withdrawal of chronic treatment with BB, ACE inhibitors or ARBs during the acute phase is not always justified and can have long-term prognostic implications.33
At this point, it is necessary to reflect on the lack of evidence regarding HF treatments in the elderly. This is even more alarming in the acute phase and in patients with systolic dysfunction.16 In fact, the PREDICT (Personalized Risk Evaluation and Diagnosis In the Coronary Tree) study, which analyzed 251 clinical trials in HF, found that a quarter of them excluded patients using an arbitrary age limit and almost half had one or more exclusion criteria which could limit the inclusion of elderly patients.34 When considering immediate treatment, it should be remembered that clinical guidelines focus on purely cardiological aspects and are based on clinical trials in which very elderly patients and/or patients with a high degree of comorbidity are under-represented, but this should not be used as an excuse to give poorer quality or different treatment to that provided to younger patients.
The relationship between mortality and age, both during hospitalization and over the short-term, was notable, although no relationship was found with revisits. These results are consistent with those from studies that have shown that both in-hospital and long-term mortality increase with age in HF patients.35 The difference between age groups in in-hospital mortality could have been due to the many variables that differ between age groups, such as levels of comorbidity, the frequency of factors associated with frailty, differences in immediate management due to the presence of disease, and the lack of published evidence for the treatments used. Short-term mortality and readmission may be related to other unmeasured aspects, such as compliance with disease-modifying treatments, ambulatory monitoring, adherence, dietary restrictions, and exercise.36
LimitationsThe present study has some limitations, such as those inherent to the study design and the lack of common protocols for SHF care in the different centers.
CONCLUSIONSThe present study provides data on daily clinical practice and revealed age-dependent differences in cardiovascular risk factors, comorbidity, geriatric syndromes, clinical presentation, and diagnostic and therapeutic procedures. These data should lead us to reflect on the care of elderly patients with AHF in the emergency room, as the care provided may not be well-suited to their priorities and needs. A multidimensional approach which does not focus purely on cardiological parameters appears to be the key in elderly patients, particularly the very elderly. Likewise, collaboration is needed between the different specialties involved in their care to avoid any age-related bias. A comprehensive geriatric evaluation adapted to the dynamics of the ED could help in identifying non-cardiological concomitant diseases and psychological, functional and social factors that could influence outcomes,2 while also contributing to the development of a care plan which better targeted all of an individual's specific needs.37,38
CONFLICT OF INTERESTSNone declared.
EAHFE-Group ICA-SEMES registry researchers: Héctor Alonso (Hospital Marqués de Valdecilla, Santander); Cristina Gil, Marta Fuentes (Hospital Universitario Salamanca); José Valles, M. José Pérez-Durá (Hospital La Fe, Valencia); José Pavón, Ana Bella Álvarez (Hospital Dr. Negrín, Las Palmas de Gran Canaria); Antonio Noval (Hospital Insular, Las Palmas de Gran Canaria); José M. Torres (Hospital Reina Sofía, Córdoba); María Luisa López-Grima (Hospital Dr. Peset, Valencia); Alfons Aguirre (Hospital del Mar, Barcelona); Helena Sancho, Francisco Ruiz (Hospital de Valme, Sevilla); José Miguel Franco, Antonio Giménez (Hospital Miguel Servet, Zaragoza); Sergio Pardo (Hospital San Juan, San Juan de Alicante); Ana Belén Mecina (Hospital de Alcorcon, Alcorcón); Josep Tost (Consorci Sanitari de Terrassa, Terrassa); Jordi Fabregat (Hospital Mútua de Terrassa, Terrassa); Francisco Epelde (Consorci Sanitari i Universitari Parc Taulí, Sabadell); Susana Sánchez (Hospital Rio Ortega, Valladolid); Pascual Piñera (Hospital Reina Sofía, Murcia); Raquel Torres (Hospital Severo Ochoa, Leganés); Miguel Alberto Rizzi, Aitor Alquezar (Hospital de Sant Pau, Barcelona); Javier Lucas (Hospital General de Albacete, Albacete); Fernando Richard (Hospital de Burgos, Burgos); José Garrido (Hospital Virgen de la Macarena, Sevilla).