Keywords
INTRODUCTION
Despite successful repair, the estimated survival rate of patients with aortic coarctation (AoCo) is less than that of the general population (after repair, 80% of patients are alive at 40-50 years1). This reduction in survival is due to complications such as recoarctation, hypertension, atherosclerotic disease, heart failure, early stroke, and even sudden death.2-4 The obstruction caused by AoCo causes pressure overload in the left ventricle (LV). After the obstruction has been resolved, LV adaptation to the original pressure overload may persist, even in patients with normal blood pressure and without a significant pressure gradient in the repair site, and abnormal remodeling has been described.5,6
Using conventional endocardial indexes determined by echocardiography, previous studies have demonstrated normal or increased systolic performance in these patients.7,8 The myocardial performance index (MPI), or TEI-Doppler index, is an echocardiographic parameter that enables a more accurate assessment of overall LV performance.9 Its usefulness in the study of several heart diseases has already been demonstrated. The aim of this study was to evaluate overall LV performance using the MPI in children with a history of AoCo after successful repair and attempt to identify the factors that predispose toward persistent abnormalities and late complications.
METHODS
Study Design
This observational study included patients with who had undergone successful repair of isolated AoCo by surgery or catheterization in our hospital from January 1990 to January 2007. Patients were included prospectively, but data were collected retrospectively. Repair was considered successful when the systolic blood pressure difference between the right arm and right leg was £15 mmHg, confirmed by echocardiogram. The exclusion criteria included the following: patients with residual coarctation or recoarctation (systolic blood pressure difference between the right arm and right leg or corrected gradient in the repaired site >15 mm Hg), hypertension (systolic blood pressure or diastolic blood pressure ≥90th percentile for age, sex and body surface
area, or antihypertensive therapy), patients with some associated congenital heart disease (such as bicuspid aortic valve), some other complication associated with AoCo or its repair (aortic aneurysm, neurological sequelae, etc), systemic disease or clinical symptoms which could affect the assessment of LV function (sepsis, surgery, drugs, etc), and in cases where echocardiography was not performed prior to the repair or that was inappropriate for analysis. During the study period, 379 patients diagnosed with AoCo were treated in our hospital by surgery or catheterization: 285 (75%) had some associated congenital heart disease, including bicuspid aortic valve; 49 (52%) of the remaining 94 patients had some complication after AoCo repair (hypertension, recoarctation, residual coarctation, aneurysm in the AoCo site, neurological sequelae, etc). In 5 cases, the echocardiogram performed prior to AoCo repair was not suitable for analysis. The remaining 40 patients formed the study group (34 males). Age at the time of repair ranged from 10 days to 10 years (4.1 [3.2]; median, 3.8 [0.08-6.1] years). Age at the time of the study ranged from 43 days to 15 years (6.9 [2.1]; median, 5.2 [2.5-10.5] years). Follow-up time was between 1 month and 14.6 years (4.25 [2.29]; median, 4.1 [1.25-9.25] years). Surgical repair was performed in 27 (67.5%) patients. The surgical techniques employed were coarctectomy with end-to-end anastomosis in 23 (85%) patients, including 7 neonates, coarctectomy with left subclavian artery angioplasty in 3 (11%), and left subclavian artery angioplasty and teflon patch in 1. Transcatheter aortic angioplasty was performed in 13 (32.5%) using a Tyshak balloon in 11 and a Mansfield balloon in 2. Balloon diameters were 5-18 mm (10.1 [2.3]). The study included a control group of 31 healthy children referred to the hospital for vaccination or first visit for mild disorders such as caries, dermatitis, attention deficit, etc, in whom congenital heart disease or some other systemic disease had been ruled out. There were no differences between groups in age, sex, and body surface area. Patients were classified into 4 groups, according to clinical symptoms at the time of diagnosis as follows: a) asymptomatic and without arterial hypertension; b) with arterial hypertension; c) with heart failure; and d) in shock. The reason for consultation was heart failure in 13 (32.5%) patients; 12 asymptomatic patients were referred due to a murmur or a discrepancy between the femoral pulses, without hypertension being recorded at the time of diagnosis or during follow-up; 11 were referred due to arterial hypertension; and 4 neonates were admitted to the emergency department in a state of shock.
Echocardiographic Studies
The echocardiograms were analyzed prior to AoCo repair. The following were recorded: type of AoCo, gradient in the AoCo site, left ventricular ejection fraction (LVEF), left ventricular shortening fraction (LVSF), and LV mass and volume at LV end-diastole. The values of LV mass and volume at LV end-diastole of the patients were compared to normal values for age, weight, and body surface area,10 and used to classify them into 4 groups:
1. Mild-to-moderate LV hypertrophy without dilatation: LV mass £+3 standard deviations of the normal LV value and volume at end-diastole £+1 standard deviation of the normal value.
2. LV hypertrophy and mild-to-moderate dilatation: LV mass >+3 standard deviations of the normal LV value and volume at end-diastole >+3 standard deviations of the normal value.
3. Severe LV hypertrophy with or without dilatation: LV mass ≥+3 standard deviations of the normal LV value and volume at end-diastole £+3 standard deviations of the normal value.
4. Severe LV dilatation with or without hypertrophy: LV mass £+3 standard deviations of the normal LV value and volume at end-diastole >+3 standard deviations of the normal value.
To evaluate current LV performance, a Sonos 5500 Philips echocardiograph was used with simultaneous electrocardiographic tracing. The measurements were obtained with an average of 5 consecutive cycles. The corrected residual gradient in the AoCo site was obtained in the suprasternal view using the Bernoulli equation. The LVEF and LVSF were obtained in the parasternal long-axis view in M mode following standard methodology. Left ventricular mass was calculated using the Dereveux formula adjusted to the body surface area. The MPI was obtained in the apical 5-chamber view using the following formula9:
MPI=ICT+IRT/ET
where the isovolumetric contraction time (ICT) is the interval between the end of mitral flow and the beginning of aortic flow; the isovolumetric relaxation time (IRT) is the interval between the end of aortic flow and the beginning of the following mitral flow; and ejection time (ET) is the interval from the beginning of aortic flow until the end. The MPI was considered normal11 if it was £0.42.
Statistical Analysis
The statistical analysis was performed with SPSS version 12 software for Windows. Continuous variables with a normal distribution are expressed as mean (standard deviation) and were compared using the Student t test; variables with a non-normal distribution are expressed as median and quartiles and were compared using the Mann-Whitney U test. The discrete variables are expressed as absolute values and percentages and were compared using Pearson's c2 or with Fisher's exact test. Logistic regression analysis was performed to assess the independent role of clinical and echocardiographic factors as predictors of general left ventricular dysfunction based on the MPI. Variables associated with ventricular dysfunction were included in the univariate analysis. The adjusted odds ratios are shown. A P value less than .05 was considered significant. The cutoff was corrected for multiple comparisons.
RESULTS
There was localized juxtaductal AoCo in 29 (72.5%) patients and 11 patients had AoCo associated with a certain degree of hypoplasia of the aortic isthmus or the transverse aortic arch. The pressure gradient in the AoCo site was 45 mm Hg. The LVEF and LVSF were normal in all the patients at the time of diagnosis. Before the repair, 20 (50%) patients had a pattern of moderate hypertrophy, with a slight degree of ventricular dilatation; 15 (37.5%) patients had moderate left ventricular hypertrophy only without dilatation; and 5 patients were of special note due to the special characteristics of the LV. Three had severe LV dilatation, with a slight degree of LV hypertrophy, and 2 had severe LV hypertrophy, given the normal course of the disease. Table 1 shows the baseline clinical and echocardiographic characteristics of the patients before AoCo repair.
Evaluation of the Left Ventricle After Successful Repair of Aortic Coarctation
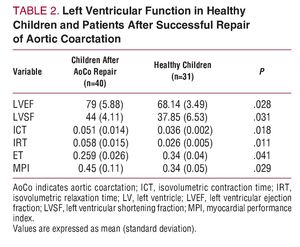
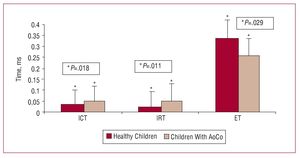
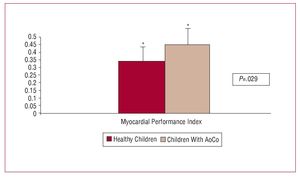
Table 2 shows the results of successful AoCo repair on LV function. The LVEF increased in 33 patients, was normal in 6, and decreased in 1 patient who underwent intervention at 8 years of age, and who had severe hypertension and concentric left ventricular hypertrophy at the time of diagnosis. The LVSF increased in 27 patients and was normal in 13. Both the LVEF and LVSF were significantly higher in the patient group than in the control group (LVEF: 79 [5.88] vs 68.14 [3.49], P=.028; and LVSF: 44 [4.11] vs 37.8 [6.5], P=.031) (Figure 1). The ICT was 0.051 s; IRT, 0.058 s; and ET, 0.259 s. The ICT was significantly greater in the patient group (0.051 vs 0.036; P=.018). This was also the case for the IRT (0.058 vs 0.026; P=.011) and MPI (0.45 vs 0.34; P£.029). On the other hand, the ET was significantly less in the patient group (0.259 vs 0.34; P=.029) (Figures 2 and 3). Nineteen patients (47.5%) had an abnormal MPI (>0.42) and in 21 patients (52.5%) MPI was normal (£0.42).
Figure 1. Comparison of left ventricular ejection fraction (LVEF) and left ventricular shortening fraction (LVSF) in children after aortic coarctation (AoCo) repair and healthy children.
Figure 2. Comparison of isovolumetric contraction time (ICT), isovolumetric relaxation time (IRT), and ejection time (ET) in children after aortic coarctation (AoCo) repair and healthy children.
Figure 3. Comparison of myocardial performance index values in children aortic coarctation (AoCo) repair and healthy children.
The univariate analysis showed a statistically significant association between abnormal MPI and age >4 years at the time of repair, arterial hypertension at the time of diagnosis, and the LV having abnormal echocardiographic characteristics before repair, since the patients older than 4 years (P=.046) at the time of repair, those with hypertension (P=.026), and those with a very dilated LV (P=.042) or severely hypertrophic LV (P=.045) at the time of diagnosis had a significantly greater MPI (Table 3). Multivariate logistic regression analysis, which included the variables associated with ventricular dysfunction in the univariate analysis, age >4 years at the time of repair, severe LV hypertrophy or dilatation before the repair and increased left ventricular mass, had an odds ratio (OR) >1. However, only hypertension was shown to be an independent risk factor predicting left ventricular dysfunction in this patient group (Table 4). There were no significant differences between groups regarding sex, type of coarctation, and the treatment modality for AoCo.
DISCUSSION
Due to the high rate of late complications, some studies point out that AoCo, rather than being an isolated entity characterized by the simple mechanical obstruction of the aorta, is actually a general disease of the cardiovascular system.4 The following factors have been proposed as predisposing to persistent abnormalities: older age at the time of repair,2,3 impaired elastic properties of the aorta,12,13 different thresholds of the autonomic nervous system,14,15 and hypertension3 and persistent LV hypertrophy. After the obstruction caused by AoCo has been eliminated, the LV begins a remodeling process; however, the LV geometry and hypertrophy do not completely return to normal5: abnormal patterns of remodeling with concentric hypertrophy have been verified in 12.5% of patients and eccentric remodeling in up to 27.5%.6 Previous studies conducted with conventional echocardiographic methods have demonstrated that LV systolic function and contractility increase in patients after AoCo repair.7,8
These studies contrast with animal models where pressure overload was induced16,17 and with studies in humans with hypertension18,19 where LV hypertrophy was associated with a gradual deterioration in ventricular function and contractility. In altered LV geometry, fiber shortening is nonuniform, since subendocardial myocardial fiber shortening exceeds subepicardial shortening, and thus the endocardial indices frequently overestimate fiber shortening.20 Some authors have proposed that normal or elevated LVEF and LVSF imply systolic dysfunction in the presence of LV hypertrophy.18
The MPI is an echocardiographic parameter that includes ICT, IRT, and ET in its calculation, making it possible to evaluate overall LV performance. Given that this approach is less dependent on ventricular geometry and preload,9 it is much more sensitive than the endocardial methods and Doppler flow imaging of the mitral valve that are traditionally used to evaluate LV function. The MPI has demonstrated its usefulness in the study of several heart diseases, and has been shown to correlate well with the invasive measurement of left ventricular systolic and diastolic function by cardiac catheterization (derived from pressure vs time and tau).21 To the best of our knowledge, the present study is the first to describe overall LV performance evaluated with the MPI in children with AoCo several years after successful repair. The most important finding of this study was that, despite having normal blood pressure at rest, low gradients in the AoCo site and normal or high LVEF and LVSF values, the MPI of our patients was significantly higher than that of a control group of healthy children, since abnormal MPI values were found in 47.5% of patients. The subclinical alterations in overall LV performance found in our study may be one of the multiple factors that can promote persistent LV hypertrophy in these patients. Our patients also had longer ICT and IRT than the control group and shorter ET, which implies that patients with normal MPI still present subtle abnormalities in LV function that escape notice when using standard methods to assess ventricular function. These findings agree with recent studies that have demonstrated abnormal regional myocardial deformation properties with reduced LV longitudinal shortening and increased LV circumferential shortening in patients after successful AoCo repair.22,23
We found that being aged >4 years at the time of repair and an LV with very abnormal characteristics before the repair could be involved in the general LV dysfunction observed in our patients, although only arterial hypertension before repair proved to be an independent risk factor for general dysfunction evaluated with the MPI (Tables 4 and 5). The findings of this study are clinically relevant, since the subtle and subclinical abnormalities in LV function associated with a rigid aorta with little elasticity, an abnormal pulse wave at the repair site, and the previously described abnormalities of the autonomic system can play a role in the appearance of late arterial hypertension in a high percentage of cases after AoCo repair which, in turn, predispose to greater LV hypertrophy, atherosclerotic disease, and early cardiovascular events. It is likely that the LV of some patients with AoCo, when subject to high afterload, subsequently develops hypertrophy with or without dilatation and, once the obstruction is eliminated, improves in some cases but in others continues to lose normal geometry leading to abnormalities in LV function. This patient subgroup requires the closest observation with continuous blood pressure monitoring, stress testing, and measurement of blood pressure and the gradient in the AoCo site while exercising, as well as following up overall LV performance to carefully assess indications for beta-blockers or angiotensin-converting enzyme inhibitors.
Study Limitations
The present study has several limitations. The most important is follow-up time, which was not homogeneous among the patients and was sometimes very short. The second limitation is that blood pressure and the gradient in the coarctation site were not measured during exercise, and thus we cannot ensure how many of our patients had elevated blood pressure or pressure gradient values in the AoCo site during exercise. Third, the study was conducted in a single hospital center with strict exclusion criteria making the patient group small, and thus decreasing the power of the multivariate analysis.
CONCLUSIONS
The overall LV performance evaluated with the MPI was abnormal in 47.5% of cases of AoCo even after successful repair and despite having normal or increased endocardial indices. It is likely that arterial hypertension before repair, older age at the time of repair and evidence of very abnormal LV at the time of diagnosis can play a role in suboptimal LV remodeling. However, the sample size makes it impossible to identify the independent factors that lead to ventricular dysfunction developing in these patients. Longitudinal studies including a greater number of cases and longer follow-up time are needed to attempt to determine the mechanisms that explain the persistent abnormalities in these patients.
ABBREVIATIONS
AoCo: aortic coarctation
ET: ejection time
ICT: isovolumetric contraction time
IRT: isovolumetric relaxation time
LV: left ventricle
MPI: myocardial performance index
SEE EDITORIAL ON PAGES 1117-9
Correspondence: Dra. N.A. Balderrábano Saucedo.
Dr. Márquez, 164. Col. Doctores. 06720 Mexico DF. Mexico.
E-mail: balderrabano_6@yahoo.es
Received January 3, 2008.
Accepted for publication June 10, 2008.