To the Editor,
Percutaneous aortic valve replacement may be an alternative in the treatment of severe symptomatic aortic valve stenosis (AS) with a high surgical risk.
In most cases a femoral approach is used, but in spite of the reduction in the diameter of the release devices, this approach is contraindicated in the presence of peripheral femoro-illiac arterial disease. Transapical deployment of the Edwards-Sapiens prosthesis involves a left thoracotomy and is associated with greater mortality than the femoral approach, although it is generally used in patients with a higher EuroSCORE.1
We present 2 cases in which the left subclavian artery (LSA) was used for vascular access for the implant of a CoreValve (Breda, Holland) aortic prosthesis, after discarding the possibility of a femoral approach.
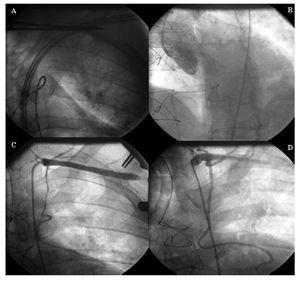
Case 1. The patient was a 68-year-old man with chronic obstructive pulmonary disease and a stroke with residual hemiparesis. He was diagnosed with AS (area, 0.45 cm2/m2) and severe pulmonary hypertension, and was in NYHA functional class IV. Cardiac catheterization showed a porcelain thoracic aorta, and femoro-iliac disease with severe stenosis at various levels. After evaluating the surgical risk (logistic EuroSCORE of 30.5%), the LSA was used because it had a favorable anatomy and diameter. The implant was carried out under local anesthesia and superficial sedation. The cardiac surgeon performed an infraclavicular incision, exposing the LSA. After making the arteriotomy, a 7 Fr flexometallic introducer was advanced and, after imaging the left ventricle, exchanged for an 18 Fr introducer with a high-support guidewire (Figure, A). After aortic valvuloplasty with a 22 mm balloon and cardiac overstimulation with a pacemaker, the release system of the 26 mm CoreValve prosthesis was advanced to the left ventricle. The implant was guided by angiography to verify the correct position, and an absence of a transvalve gradient and aortic regurgitation was determined. Finally, the surgeon sutured the LSA, and closed the planes. After 24 h in the post-surgery recovery unit the patient was transferred to the ward and discharged on the fourth day. After a follow-up of 3 months the patient, who was asymptomatic, died of sudden death.
Figure 1. Implant of the CoreValve aortic prosthesis for which the left subclavian artery was used for vascular access. A: advancing the prosthesis release system via the left subclavian artery. B: angio-graphic result after implantation of the CoreValve aortic prosthesis. C: iatrogenic dissection of the left mammary artery. D: implant of overlapping drug-eluting stents in the left mammary artery.
Case 2. A 50-year-old man had a history of anterior and inferior acute myocardial infarctions (AMI), with coronary surgery with mammary to left anterior descending and saphenous to marginal grafts in 1993. He had aortic valve disease, moderate stenosis and severe regurgitation, with ventricular dilation and moderate dysfunction, and was in NYHA functional class III. The surgical risk (EuroSCORE of 10.9%), a permeable mammary artery graft and severe femoro-iliac disease all indicated the implantation of a CoreValve prosthesis via the LSA. The procedure was carried out without aortic valvuloplasty, implanting a 29 mm CoreValve prosthesis, with the technique described above. After verifying the correct position and the absence of periprosthetic regurgitation (Figure, B), the patient presented anterior ST segment elevation and hemodynamic instability that necessitated intubation and mechanical ventilation, with inotropic support. After discarding other possible causes (spasm or ischemia from the introducer that was withdrawn), proximal iatrogenic dissection of the mammary artery was visualized (Figure, C), which was treated with the implant of overlapping drug-eluting stents (Figure, D). The course was favorable, with mild CK-MB mass elevation of 28 ng/mL. The patient was extubated after 24 h and discharged after 7 days. After a follow-up of 4 months the patient remained asymptomatic.
The LSA is an attractive approach for the treatment of severe AS with the CoreValve prosthesis in patients in whom a femoral approach is not possible. This approach demands surgeon collaboration and can be undertaken with local anesthesia and superficial sedation.
An isolated case has been reported using the LSA.2 In the series of Grubbe et al3 involving 136 patients, a subclavian approach was used in 3 cases, although no analysis was made of the results or complications.
We present 2 cases with a LSA approach, and consider one of the potential complications of this access to be dissection of the mammary artery graft.
Accordingly, in patients with symptomatic AS, with a high surgical risk or in whom a femoral approach is not possible, the LSA may be an alternative to the transapical approach.