.
IntroductionIn patients who have undergone left atrial (LA) interventions such as percutaneous balloon mitral valvuloplasty (PBMV), catheter ablation of atrial fibrillation or mitral valve repair, the quantitation of the changes in LA size and function is becoming an important target to assess the success of procedures or interventions. Echocardiography remains the imaging modality of choice for LA assessment because of its wide availability and cost-effectiveness. Newer echocardiographic techniques such as 3-dimensional echocardiography and deformation imaging still have a limited applicability mainly as research tools, but they can potentially provide valuable information on both LA size and myocardial mechanics. Future studies will demonstrate whether these techniques could be clinically useful in patients undergoing mitral valve interventions such as PBMV, where it is prudent to monitor its impact on LA phasic functions, and to understand how these alterations in LA function may affect management decisions such as anticoagulation and redo procedures.
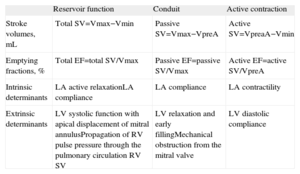
The left atrium plays an integral role in cardiac performance, acting as: a) a reservoir during left ventricular systole; b) a conduit for blood transiting from the pulmonary veins to the left ventricle during early diastole; c) an active contractile chamber that augments left ventricular filling in late diastole, and d) a suction source that refills itself in early systole. Through these varying mechanical functions (Table),1 the left atrium modulates left ventricular filling.2 In addition, the left atrium acts as a volume sensor, the LA wall releasing natriuretic peptides in response to stretch and generating natriuresis, vasodilatation and inhibition of the sympathetic nervous system and renin-angiotensin-aldosterone system. Since LA contraction generates up to 30% of total left ventricular stroke volume in normal individuals, the active LA contribution is of particular importance in the setting of left ventricular dysfunction, in order to maintain an adequate left ventricular stroke volume. The loss of the active LA contribution to left ventricular filling with atrial fibrillation can often lead to functional deterioration.
Left Atrial Phasic Function Parameters and Their Determinants.
| Reservoir function | Conduit | Active contraction | |
| Stroke volumes, mL | Total SV=Vmax−Vmin | Passive SV=Vmax−VpreA | Active SV=VpreaA−Vmin |
| Emptying fractions, % | Total EF=total SV/Vmax | Passive EF=passive SV/Vmax | Active EF=active SV/VpreA |
| Intrinsic determinants | LA active relaxationLA compliance | LA compliance | LA contractility |
| Extrinsic determinants | LV systolic function with apical displacement of mitral annulusPropagation of RV pulse pressure through the pulmonary circulation RV SV | LV relaxation and early fillingMechanical obstruction from the mitral valve | LV diastolic compliance |
EF, emptying fraction; LA, left atrial; LV, left ventricular; RV, right ventricular; SV, stroke volume; Vmax, maximum left atrial volume; Vmin, minimum left atrial volume; VpreA, left atrial volume before atrial contraction.
Modified by To et al.1
Mitral stenosis affects both LA size and function. Chronic pressure overload due to valvular obstruction and atrial inflammation secondary to rheumatic carditis both lead to the dilation of the left atrium and LA appendage, atrial wall fibrosis and disorganization of LA myocardial bundles. All of these changes in the left atrium constitute the basis for atrial fibrillation onset. The occurrence of atrial fibrillation is independently correlated with the severity of mitral stenosis and LA pressure level, but also with the degree of LA enlargement.3 Furthermore, LA size has been shown to be a predictor of LA stasis and spontaneous contrast.4 Consequently, taking into consideration the potential prognostic implications, the evidence of a significant reduction in LA size and of an improvement in LA function(s) after PBMV may be clinically relevant. However, little is known about the effect of PBMV on both LA size and functions.5
With echocardiography, the quantification of LA size in patients with mitral stenosis has been conventionally performed by measuring the anteroposterior LA diameter and the LA area planimetered on a 2-dimensional (2D) apical 4-chamber view of the heart, although limitations regarding its evaluation using these parameters have been reported.6 Indeed, the most recent recommendations for cardiac chamber quantification indicate LA volume as the preferred measure of its size.7 The LA shape is often irregular and its enlargement does not occur in a symmetrical way.6 Therefore, linear 2D measurements such as LA anteroposterior or superoinferior diameters might not reflect its actual size.8 On the other hand, LA volume calculation by 2D echocardiography is limited by significant geometric assumptions and by a low test-retest reproducibility due to the difficulty of replicating the exact position and orientation of 2D imaging planes.
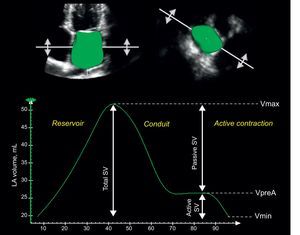
Three-dimensional echocardiography (3DE) has been recently demonstrated to be more accurate and reproducible than 2D for LA volume quantification in head-to-head comparisons with cardiac magnetic resonance9 and 64-slice multidetector computed tomography.10 Furthermore, 3DE could become a more reliable method for the assessment of LA function, providing accurate information on the phasic changes of LA volume during the cardiac cycle1,11 (Figure).
Quantitation of a full-volume 3-dimensional dataset permits the accurate measurement of the left atrial phasic functions and their relationship with the cardiac cycle. Left atrial volume increases to its maximum during the reservoir phase, followed by 2 phases of progressive emptying (conduit and active contraction phases) with the left atrial volume decreasing to the pre-atrial contraction left atrial volume and then the minimum left atrial volume. Accordingly, total left atrial stroke volume can be divided into passive and active components (see also Table). Active SV, active left atrial stroke volume; LA, left atrial; Passive SV, passive left atrial stroke volume; Total SV, total left atrial stroke volume; Vmax, maximum left atrial volume; Vmin, minimum left atrial volume; VpreA, left atrial volume before atrial contraction.
In this issue of Revista Española de Cardiología, Vieira et al. have used 2D and 3DE to study the effects of PBMV on LA volumes and LA emptying fraction, comparing the parameters obtained before the procedure, after 72h, and at 12 months in 28 symptomatic patients with mitral stenosis.12 They showed a significant favorable LA remodeling after succesful PBMV: LA maximal volume decreased from 50±12mL/m2 to 42±11mL/m2 at 72h after PBMV, and further to 40±10mL/m2 at 1-year follow-up. Similarly, LA emptying fraction increased from 32%±10% to 43%±6% at 72h after PBMV and to 47%±6% at 1-year follow-up. In this study, LA volumes measured by 2D echocardiography were 15% larger than the values obtained by 3DE. This finding contradicts all previous studies that compared 2D and 3DE for LA volume assessment and consistently reported larger LA volumes by 3DE.11 Unfortunately, the authors did not include a reference imaging modality (ie, magnetic resonance or computed tomography) in their study and, consequently, which of the 2 echocardiographic techniques provided the most accurate measurement remains unknown.
Nevertheless, accuracy or precision in measurement in comparison with a reference technique is not the only clinically important aspect of a study or test.13 Indeed, this is sometimes of more concern to engineers than it is to clinicians. Clinicians are used to dealing with a certain extent of uncertainty in their practice, where so many variables can have an impact on a patient's clinical presentation or outcome that an inaccuracy of a few percentage points in measuring LA volume, for instance, may be irrelevant. Much more clinically important is the reliability or precision of measurements, which is influenced by both random error and bias. A highly precise or reliable study will give the same measurement on sequential examinations and is a pivotal component of a good test to be used in patient follow-up. In fact, if a study is highly precise despite being of limited accuracy, most clinicians would find it to be very useful, provided that the bias from the actual measurements is reproducible.
Measurement of LA phasic volumes using 2D is time-consuming and errors can arise from geometric assumptions of biplane volume calculations, as well as from difficulties related to restricted windows or timing of atrial events. Now 3DE is becoming the echocardiographic modality of choice to measure LA volumes,11 since the availability of LA 3D data sets that can be quantified throughout the various phases of the cardiac cycle can overcome most of these limitations. In addition, the use of 3DE has the advantages of being independent of geometric assumptions about LA shape, no longer influenced by imaging plane orientation and less dependent on operator expertise due to an automated identification of the endocardium. All these characteristics concur at determining the lower test–retest variability of 3DE LA volumes compared with 2D.14 Last but not least, current 3DE has acceptable temporal resolution, which is not easily achieved with cardiac computed tomography or magnetic resonance and is critical to obtain an accurate assessment of phasic LA functions.
The known disadvantages of 3DE relate to its relatively lower temporal resolution when compared with 2D, poor image quality (which may be less of a problem with 2D imaging as the spatial resolution of this modality is more favorable), and susceptibility to stitching artifacts (since electrocardiogram-gated acquisitions obtained by stitching together 4 to 7 subvolumes acquired from consecutive heart beats are required to create a large volumetric data set with an acceptable temporal resolution). This may be problematic in patients with “irregular” atrial fibrillation.
In addition to LA chamber function, the study of LA myocardial mechanics is an emerging field that may provide new ways to assess LA phasic function. Analogous to assessing left ventricular mechanics by strain and strain rate imaging, measures of myocardial deformation using both tissue velocity imaging and 2D speckle tracking have been increasingly adapted to study LA mechanics.15 These techniques would have been particularly useful to assess LA function changes occurring after successful PBMV, in particular to distinguish between LA volume changes due to the abrupt decrease in LA afterload from an actual recovery in LA myocardial function that may be even more important for patients’ long-term prognosis and freedom from complications, such as atrial fibrillation and embolic events.
In conclusion, assessing the changes in LA size and function in patients who have undergone LA interventions such as PBMV, catheter ablation of atrial fibrillation, or mitral valve repair is becoming an important target to assess the success of procedures/interventions. Echocardiography remains the imaging modality of choice for LA assessment because of its wide availability and cost-effectiveness. Newer echocardiographic techniques such as 3DE and deformation imaging still have a limited applicability mainly as research tools, but can potentially provide valuable information on both LA size and myocardial mechanics. Future studies will demonstrate whether these techniques could be clinically useful in patients undergoing mitral valve interventions such as PBMV, where it is prudent to monitor its impact on LA phasic functions, and to understand how these alterations in LA function may affect management decisions such as anticoagulation and redo procedures.
FundingDenisa Muraru was supported by a Research Grant awarded by the European Association of Echocardiography.
Conflicts of interestDr. Luigi P. Badano has received equipment grants from GE Healthcare and is on the Speakers’ Bureau of this company. Dr. Denisa Muraru has received equipment and research funding from GE Healthcare. Angelica Nour has no conflicts of interest to disclose.