The European Society of Cardiology (ESC) guidelines are endorsed by the Spanish Society of Cardiology (SEC) and translated into Spanish for their publication in the Revista Española de Cardiología. Under the policy introduced in 2011, each new guideline is accompanied by an article that formulates comments in accordance with the objectives and methodology recommended in the article that established the Guidelines Committee of the SEC.1
In the present article, we discuss the new European guidelines for ST-segment elevation acute myocardial infarction (STEMI).2 The Guidelines Committee established a work group composed of members proposed by the Ischemic Heart Disease, Hemodynamics, Clinical Cardiology, Heart Failure, and Geriatric Cardiology work groups.
As a general comment, we consider that the present guidelines introduce highly interesting developments and that the topics are dealt with clearly and in detail. However, we should also point out that it contains 157 recommendations, 69 (44%) of which are accompanied by level C evidence (expert consensus), predominantly in the sections on in-hospital management, heart failure, and complications, fields in which there thus remains ample room for individualization and progress in clinical research. In applying them, we should not forget that the guidelines themselves remind us that the level A and B recommendations are based on clinical trials, and that even these results are open to interpretation. The different therapeutic options could be influenced by the available resources. Thus, it will be increasingly necessary to perform cost-efficiency studies that aid us in choosing among the different strategies.
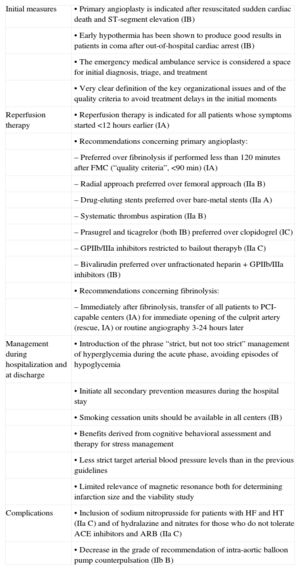
For the purpose of making the article more readable and to highlight the most relevant or novel aspects, as well as those that are not made clear or are not addressed, we have summarized them in Tables 1–2, respectively.
2012 European Society of Cardiology Guidelines for the Treatment of ST-Segment Elevation Acute Myocardial Infarction. Most Relevant and/or Novel Aspectsa.
| Initial measures | • Primary angioplasty is indicated after resuscitated sudden cardiac death and ST-segment elevation (IB) |
| • Early hypothermia has been shown to produce good results in patients in coma after out-of-hospital cardiac arrest (IB) | |
| • The emergency medical ambulance service is considered a space for initial diagnosis, triage, and treatment | |
| • Very clear definition of the key organizational issues and of the quality criteria to avoid treatment delays in the initial moments | |
| Reperfusion therapy | • Reperfusion therapy is indicated for all patients whose symptoms started <12hours earlier (IA) |
| • Recommendations concerning primary angioplasty: | |
| – Preferred over fibrinolysis if performed less than 120minutes after FMC (“quality criteria”, <90 min) (IA) | |
| – Radial approach preferred over femoral approach (IIa B) | |
| – Drug-eluting stents preferred over bare-metal stents (IIa A) | |
| – Systematic thrombus aspiration (IIa B) | |
| – Prasugrel and ticagrelor (both IB) preferred over clopidogrel (IC) | |
| – GPIIb/IIIa inhibitors restricted to bailout therapyb (IIa C) | |
| – Bivalirudin preferred over unfractionated heparin + GPIIb/IIIa inhibitors (IB) | |
| • Recommendations concerning fibrinolysis: | |
| – Immediately after fibrinolysis, transfer of all patients to PCI-capable centers (IA) for immediate opening of the culprit artery (rescue, IA) or routine angiography 3-24hours later | |
| Management during hospitalization and at discharge | • Introduction of the phrase “strict, but not too strict” management of hyperglycemia during the acute phase, avoiding episodes of hypoglycemia |
| • Initiate all secondary prevention measures during the hospital stay | |
| • Smoking cessation units should be available in all centers (IB) | |
| • Benefits derived from cognitive behavioral assessment and therapy for stress management | |
| • Less strict target arterial blood pressure levels than in the previous guidelines | |
| • Limited relevance of magnetic resonance both for determining infarction size and the viability study | |
| Complications | • Inclusion of sodium nitroprusside for patients with HF and HT (IIa C) and of hydralazine and nitrates for those who do not tolerate ACE inhibitors and ARB (IIa C) |
| • Decrease in the grade of recommendation of intra-aortic balloon pump counterpulsation (IIb B) |
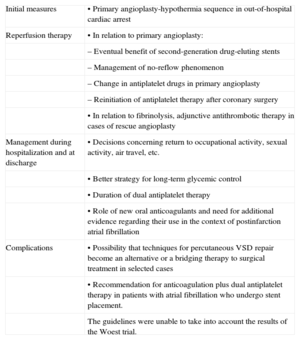
2012 European Society of Cardiology Guidelines for the Treatment of ST-Segment Elevation Acute Myocardial Infarction. Aspects Not Clarified and Aspects Not Addressed.
| Initial measures | • Primary angioplasty-hypothermia sequence in out-of-hospital cardiac arrest |
| Reperfusion therapy | • In relation to primary angioplasty: |
| – Eventual benefit of second-generation drug-eluting stents | |
| – Management of no-reflow phenomenon | |
| – Change in antiplatelet drugs in primary angioplasty | |
| – Reinitiation of antiplatelet therapy after coronary surgery | |
| • In relation to fibrinolysis, adjunctive antithrombotic therapy in cases of rescue angioplasty | |
| Management during hospitalization and at discharge | • Decisions concerning return to occupational activity, sexual activity, air travel, etc. |
| • Better strategy for long-term glycemic control | |
| • Duration of dual antiplatelet therapy | |
| • Role of new oral anticoagulants and need for additional evidence regarding their use in the context of postinfarction atrial fibrillation | |
| Complications | • Possibility that techniques for percutaneous VSD repair become an alternative or a bridging therapy to surgical treatment in selected cases |
| • Recommendation for anticoagulation plus dual antiplatelet therapy in patients with atrial fibrillation who undergo stent placement. | |
| The guidelines were unable to take into account the results of the Woest trial. |
VSD, ventricular septal defect.
The guidelines especially stress the prevention of delays in treatment. When STEMI is suspected, it is essential to facilitate rapid access to defibrillation during the initial moments, if indicated, and guarantee earlier access to reperfusion. The new position is that the first therapeutic option for patients resuscitated from sudden cardiac death and who have ST-segment elevation is the performance of primary angioplasty, provided the recommended time intervals are met. Moreover, the guidelines point to evidence showing that patients who remain in coma after resuscitation from out-of-hospital cardiac arrest benefit from therapeutic hypothermia, provided it is initiated early.
The specification of the degree of ST-segment elevation according to the age (under or over 40 years) and sex of the patients continues to be a matter of controversy. We feel that this issue could produce confusion for many professionals who must make decisions on the basis of the first electrocardiogram. We have made very little progress in the diagnosis of patients with left bundle branch block. The only new publication involves a 2011 clinical trial, but the literature offers no observations from registries establishing the true incidence of the final diagnosis of STEMI among patients who undergo catheterization because of chest pain and left bundle branch block.
This section refers to cases of suspected coronary occlusion without ST-segment elevation which, on occasion, can be extremely serious (occlusion of left main coronary artery, of a saphenous vein bypass graft to circumflex artery, etc.), but can sometimes correspond to noncoronary disease. This aspect has been addressed previously in the guidelines for non-ST-elevation acute coronary syndrome, which stress the importance of the cardiologist in documenting the clinical history as well as the need for an emergency echocardiogram.
We consider the recommendation that all hospitals that provide care to STEMI patients record time-to-treatment and regularly re view the data to ensure that they are com plying with the recommendations. In addition, the publication of these data (times of symptom onset, first medical contact, performance of electrocardiogram, initiation of reperfusion, etc.) may be useful in stimulating improvements in health care. The practice of showing the results of health care processes is not widespread either in Spain or in Europe as a whole.
The guidelines introduce the novel idea that the out-of-hospital emergency medical service plays an essential role in the entire health care process and that it must be considered not only a mode of transport, but a space for the initial diagnosis, triage, and treatment. Thus, ambulance services should be capable of performing electrocardiograms, treating pain, maintaining hemodynamic stability, carrying out resuscitation maneuvers if necessary, triaging the patient to the most appropriate center, and initiating reperfusion therapy in the case of fibrinolysis, as well as adjunctive antiplatelet therapy in the case of primary angioplasty. In Spain, some communities have had highly efficient management protocols for years. We should keep in mind that these protocols, while adapted to the special characteristics of each region, should remain faithful to the basic recommendations of the ESC, especially with respect to the target times.
Thus, the optimal treatment of STEMI is based on an efficient out-of-hospital emergency service and a good network of interconnected hospitals of different levels. The keys to the effectiveness of this organization are:
- •
Clearly defined geographical areas.
- •
Consensus protocols that take into account patient risk and the transport system available at any given time.
- •
Prehospital evaluation for appropriate triage, bypassing hospitals in which angioplasty cannot be performed.
- •
Arrival directly in the catheterization laboratory of the referral hospital, bypassing the emergency service.
It would be useful to recommend that patients with stable ischemic heart disease always carry a copy of their baseline electrocardiogram. This implies that a copy of the latest electrocardiogram be provided with the hospital discharge report.
Reperfusion TherapyThe present guidelines introduce important changes with respect to the previous recommendations. The section on reperfusion therapy is evaluated in the following 6 subsections:
Decision to ReperfuseThe most important aspect of this decision is the time factor, that is, treatment within 12hours of symptoms onset. The class I indication is maintained for patients whose symptoms began more than 12hours earlier if persistence of ischemia is demonstrated, although this is supported only by level C evidence. Reperfusion is not indicated (class III A) for stable patients who had a myocardial infarction more than 24hours earlier, in the absence of residual ischemia or viability.
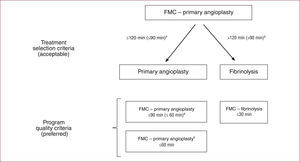
Selection of the Reperfusion StrategyA clear algorithm for the use of reperfusion therapy is presented. The most important aspect lies in increasing the strength of the indication for primary angioplasty as the treatment of choice, provided it is performed within 120minutes by an experienced team. In this respect, the objectives in terms of acceptable and preferred delays are clearly expressed. The period of 120minutes between the first medical contact and wire passage is considered to be the maximum delay to primary angioplasty in order for this to be selected as the reperfusion technique of choice. The interval during which angioplasty is preferred over fibrinolysis is reduced to 90minutes in the case of large myocardial infarction in early presenters. One novel aspect is the establishment of “quality criteria” for reperfusion therapy to be applied in a selective and individualized manner. Thus, less than 90minutes from first medical contact to wire passage is considered a quality criterion for all patients (60minutes in large myocardial infarctions in early presenters) and <60minutes for those who are brought directly to the primary angioplasty center. Maximum delays between first medical contact and STEMI diagnosis of 10minutes and between first medical contact and fibrinolysis of 30minutes are also established as quality criteria. From the practical point of view, all these criteria should be considered when designing protocols in S TEMI programs and when evaluating the results of their implementation (Fig. 1). When it is not possible to perform primary angioplasty within the first 120minutes of the first medical contact, a fibrinolytic agent should be administered. In this case, without awaiting the outcome, the patient should be transported immediately to an emergency percutaneous coronary intervention (PCI)-capable center (indication changed from IIa A to IA), where the decision will be made whether to carry out rescue angioplasty (if there are no criteria for reperfusion) or routine angiography (3-24 hours) if fibrinolysis is successful. This modification has a practical implication in defining the needs for transfer to another hospital and the increase in the range of indications for angioplasty.
Decision algorithm to select the type of therapy based on the estimated delay (acceptable) and the quality criteria for a reperfusion therapy program (preferred). This algorithm is valid regardless of the delay in the first medical contact. Thus, even in patients presenting early with ST-segment elevation acute myocardial infarction, primary angioplasty is preferred over fibrinolysis, if performed within the indicated time intervals. FMC, first medical contact.
aFor large infarctions in early presenters.
bIf the patient is in a percutaneous coronary intervention-capable center.
Technical and Pharmacological Aspects. The most novel feature is related to the introduction of radial access as the approach of choice in the majority of cases (class IIa B), due to the reduced incidence of bleeding and the resulting lower rate of mortality with respect to the femoral approach. Regarding the type of stent, the guidelines stress the importance of selecting the proper size and recommend the use of drug-eluting rather than bare-metal stents (IIa A) if the patient has no contraindications for dual antiplatelet therapy and is likely to be compliant. However, they do not mention the eventual benefits of second-generation drug-eluting stents over first-generation or bare-metal stents. The presentation of these guidelines has been followed by the publication of 2 randomized studies (EXAMINATION3 and COMFORTABLE-AMI4) that demonstrate the efficacy and safety of second-generation stents in this situation. Another new recommendation is the systematic use of aspiration catheters during the procedure. This indication has been changed from class IIb to IIa B. The results of remote conditioning and postconditioning studies are inconclusive.5 The different maneuvers undertaken to treat the failure to reestablish myocardial flow (no-reflow phenomenon) in the catheterization laboratory have also not been found to be sufficiently effective.
As a practical summary, it can be proposed that primary angioplasty be carried out using the radial approach, with thrombectomy, followed by implantation of a drug-eluting stent.
From the pharmacological point of view, one of the most novel aspects is the introduction of prasugrel and ticagrelor as antiplatelet drugs of choice (class IB for both), over clopidogrel (IC) which, in these guidelines, is relegated to situations in which prasugrel and ticagrelor cannot be administered or are contraindicated and to patients treated with fibrinolysis alone. The possibility of changing drugs in patients who have undergone clopidogrel loading prior to primary angioplasty is not mentioned in these guidelines. An important aspect, should coronary artery surgery be necessary in patients receiving these treatments, is the recommendation that surgery be postponed until 7 days after the discontinuation of prasugrel, 5 days in the case of clopidogrel, and 3 days to 5 days in the case of ticagrelor. In this situation, for those patients in whom the discontinuation of antiplatelet therapy is not advisable, the possibility of bridging therapy (with short half-life glycoprotein IIb/IIIa [GPIIb/IIIa] inhibitors) can be considered, although there is no clinical evidence to support its efficacy.
The use of GPIIb/IIIa inhibitors in STEMI has been restricted to bailout therapy in the presence of massive intracoronary thrombus, in situations of no reflow, or in thrombotic complications (IIa C). Their systematic use on arrival in the catheterization laboratory is not recommended (IIa C). As another novel feature, the guidelines present the results of the INFUSE-AMI and AIDA trials, which compare intracoronary with intravenous administration of abciximab, revealing no clear differences between the 2 strategies.
The new development with respect to anticoagulation therapy is the recommendation of bivalirudin as the agent of choice over heparin associated with GPIIb/IIIa inhibitors, based on the reduced mortality observed at 30 days and for up to 3 years in the HORIZONS-AMI trial. The guidelines mention the interaction that the administration of unfractionated heparin prior to randomization may have had in the reduced risk of stent thrombosis in a considerable number of patients. The efficacy of bivalirudin administered in combination with prasugrel or ticagrelor is not known, since clopidogrel was the adenosine diphosphate (ADP) receptor antagonist used in that trial. In the ATOLL trial, enoxaparin, when compared with unfractionated heparin, reduced the incidence of the composite endpoint (30-day mortality, myocardial reinfarction, procedural failure, and bleeding), a fact that supports its recommendation as adjunctive therapy when bivalirudin is not employed. As a practical summary concerning adjunctive therapy in primary angioplasty, pretreatment of the patient with acetylsalicylic acid and prasugrel or ticagrelor is recommended (if there are no contraindications). Likewise, the favorable safety and efficacy profile of bivalirudin with respect to combined heparins and GPIIb/IIIa inhibitors indicates that bivalirudin could be the anticoagulant of choice. Glycoprotein IIb/IIIa inhibitors would be used in situations of higher thrombogenic risk.
FibrinolysisAdjunctive Antithrombotic Therapy and Invasive Treatments. Should angioplasty not be available within the target time, the benefit of prehospital fibrinolysis is increasingly evident, especially in patients who can be treated within 60minutes of symptoms onset. The most relevant new feature, mentioned above, is the indication that once treated the patient be transferred immediately to a PCI-capable center, with the organizational implications that this entails. As adjunctive antiplatelet therapy, a combination of acetylsalicylic acid and clopidogrel is recommended, with enoxaparin as the anticoagulant of choice. Neither bivalirudin nor the new P2Y12 receptor antagonists have been studied in this context.
Treatment for Nonreperfused PatientsThis section deals with patients who arrive at the hospital more than 12hours after symptoms onset without persistent symptoms or ischemia, or those who cannot be reperfused for some clinical reason. The recommended antiplatelet therapy includes acetylsalicylic acid and clopidogrel, although ticagrelor is now added on the basis of the data of those patients in the PLATO trial who had not been revascularized. With respect to anticoagulant therapy, fondaparinux, enoxaparin, or unfractionated heparin is recommended at the same doses as those administered after fibrinolysis.
Special Clinical SituationsIn patients with multivessel disease, in the context of the acute phase of STEMI, the recommendation is to treat only the culprit artery (except in the case of cardiogenic shock or persistence of ischemia after treatment of the culprit lesion). With respect to the treatment of the other arteries with lesions, a practical recommendation is to choose a “conservative strategy”, initially with medical treatment, and treatment of the other stenoses only when there are symptoms or induced ischemia. In the case of critical stenoses in segments proximal to major vessels, the strategy should be “staged” percutaneous or surgical revascularization in a later procedure (according to a multidisciplinary decision) during the hospital stay or within 1 month of the myocardial infarction.
The recommendation not to apply sex differences in the treatment is highly relevant, as is the fact that the guidelines stress the need to adjust the dose of antithrombotic therapy in elderly patients, women, and patients with renal failure; Table 18 of the guidelines is devoted to detailing the doses of these drugs for patients with creatinine clearance of <60 mL/min. The failure to make this adjustment is a common error that leads to a considerable increase in the incidence of bleeding.
Management During Hospitalization and at DischargeLogistic Questions, Risk Assessment, and Imaging StudiesThe guidelines recommend that all hospitals that participate in the initial care of STEMI patients be equipped with a cardiac intensive care or coronary care unit. These units should be capable of providing specialized treatment to patients with acute coronary syndrome, arrhythmias, and heart failure, and their staff should be familiar with mechanical circulatory support systems, invasive and noninvasive hemodynamic monitoring, invasive and noninvasive respiratory monitoring and support, therapeutic hypothermia techniques, and renal support.
The management and duration of the hospital stay differ depending on patient risk. Although the levels of evidence are low, the guidelines recommend shortening the stay. For low-risk patients who undergo successful primary angioplasty, they consider same-day transfer to another center with no catheterization laboratory to be reasonable, although the level of recommendation is IIb C, and hospital discharge can be considered after 72hours if adequate ambulatory follow-up is possible. The question is, which patient is considered to be low-risk? Different indices (PAMI, Zwolle) can aid in very early risk stratification in patients who have undergone primary angioplasty.
The guidelines remark on the utility of the echocardiogram performed on admission in cases of uncertain diagnosis. This technique is also recommended to determine infarction size and left ventricular function, and to rule out complications. The use of magnetic resonance for these purposes is considered an alternative only when ultrasound is not feasible (IIb C).
The guidelines also point out that, once primary angioplasty has been performed and the coronary anatomy is known, the systematic assessment of ischemia prior to discharge is less important. These are level IA recommendations during the first 4 weeks to 6 weeks but only for patients with multivessel disease or in whom the possibility of revascularization of untreated vessels is being considered. Once again, the guidelines describe the strengths and weaknesses of each test, but still do not make their position clear in favor of a given modality. They are only categorical, and this is new, with regard to ruling out the utility of coronary computed tomography in this situation (III C).
For the viability study, they again enumerate the available techniques (nuclear imaging techniques, stress echocardiography, and magnetic resonance) and, because of the limited difference in the results obtained with each, leave it to the physician to decide which to employ.
TreatmentFor the first time, a special section is devoted to the management of hyperglycemia. The guidelines point out the adverse prognostic implications of hyperglycemia and recommend diagnostic efforts in patients without known diabetes mellitus. The most important and novel message is summarized in the recommendation for the “strict, but not too strict” control of hyperglycemia, with emphasis on the need to avoid hypoglycemia. This strategy is condensed to maintaining blood glucose levels below 200 mg/dL (≤11 mmol/L) and over 90 mg/dL (<5 mmol/L) during the acute phase, much more permissive than the levels accepted up to now. The objectives are clearer than the strategy for achieving them, and insulin infusion, adjusted in accordance with the results of blood glucose monitoring, is recommended in some patients (IIa B). The use of glucose-insulin-potassium infusions is not indicated (III A).
The current guidelines present a fundamental difference with respect to the previous ones concerning the medical management of the acute and subacute phases and over the long term. The organization of the information is very clearly summarized in Table 22 of the guidelines.
All the treatment and secondary prevention measures should be initiated during the hospital stay with the aim of achieving maximum compliance after discharge. The relevant aspects are the emphasis on smoking cessation, with the recommendation that smoking cessation units be made available in every center, and the comments on benefits derived from cognitive behavioral assessment and therapy for stress management. It is important to point out that cardiac rehabilitation, so underutilized in Spain, continues to be a class IB indication.
One important change refers to arterial blood pressure control. Based on data from a retrospective analysis of the PROVE-IT TIMI 22 trial, the present guidelines are less strict than the previous ones and recommend that the target systolic blood pressure be under 140mmHg, but not under 110mmHg.
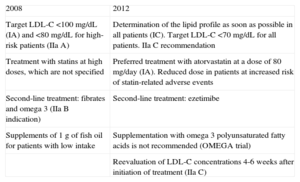
In lipid-lowering therapy, early intensive statin therapy is recommended for all STEMI patients, regardless of their cholesterol concentrations. On this occasion, the guidelines take a clear stand in favor of atorvastatin at a dose of 80mg. The major recommendations concerning this matter and the differences with respect to the preceding guidelines are shown in Table 3 of the present article.
Comparison of the Recommendations of the European Society of Cardiology for Long-Term Lipid-Lowering in the 2008 and 2012 Guidelines for ST-Segment Elevation Acute Coronary Syndrome.
| 2008 | 2012 |
| Target LDL-C <100 mg/dL (IA) and <80 mg/dL for high-risk patients (IIa A) | Determination of the lipid profile as soon as possible in all patients (IC). Target LDL-C <70 mg/dL for all patients. IIa C recommendation |
| Treatment with statins at high doses, which are not specified | Preferred treatment with atorvastatin at a dose of 80 mg/day (IA). Reduced dose in patients at increased risk of statin-related adverse events |
| Second-line treatment: fibrates and omega 3 (IIa B indication) | Second-line treatment: ezetimibe |
| Supplements of 1g of fish oil for patients with low intake | Supplementation with omega 3 polyunsaturated fatty acids is not recommended (OMEGA trial) |
| Reevaluation of LDL-C concentrations 4-6 weeks after initiation of treatment (IIa C) |
With regard to antiplatelet therapy, the administration of acetylsalicylic acid is not questioned, and the pre dominance of prasugrel and ticagrelor over clopidogrel has been mentioned in another section. The recommendations concerning the duration of antiplatelet therapy have not changed. The recommendation to maintain treatment with these agents for 12 months in patients who did not undergo stent placement (IIa C) may be debatable.
Doubts about the interaction between proton pump inhibitors and clopidogrel have been shelved because of the lack of evidence of its clinical significance, and the classical indications are maintained.
For anticoagulation therapy, more recent —and at the same time controversial— is the possibility of adding an oral factor Xa inhibitor (rivaroxaban) to acetylsalicylic acid and clopidogrel as adjunctive therapy in secondary prevention for patients at low bleeding risk (level IIb B recommendation), as tested in the ATLAS-ACS TIMI 51 trial. It is not known whether this strategy is superior to the combination of acetylsalicylic acid with prasugrel or ticagrelor. In addition to the fact that this indication has not yet been approved by the responsible agencies, a recent meta-analysis6 published after the guidelines had been released concludes that the new anticoagulant drugs show no net clinical benefit following acute coronary syndrome.
The guidelines continue to recommend (level IC) triple antithrom-botic therapy (dual antiplatelet therapy and oral anticoagulation) for patients with atrial fibrillation and STEMI. This may need to be revised in the wake of the results of the WOEST trial,7 which could not be included in the guidelines as both were presented at the same time at the last ESC congress. Said study demonstrated greater benefit, including a reduction in the overall mortality, from treatment with clopidogrel and oral anticoagulation versus the same treatment plus acetylsalicylic acid.
With respect to the remaining treatments, the postponement of beta-blockers is recommended until the patient is stabilized, except in the presence of hypertension or tachycardia and in the absence of heart failure. The indication is now level IIa B, although the recommendation remains strong for patients with ventricular dysfunction or heart failure (IA). The level of recommendation of IB is maintained for the use of aldosterone antagonists in patients with a left ventricular ejection fraction (LVEF) <40% and diabetes mellitus or heart failure, although the drug of first choice (eplerenone or spironolactone) is not specified. Given that the evidence for patients after STEMI is based exclusively on eplerenone, with its lower rate of secondary effects and its excellent results in patients with heart failure in less advanced stages (EMPHASIS HF trial), we feel that eplerenone should be considered a first-line treatment within this group of drugs.
If the recommendations of the guidelines are followed strictly, after a myocardial infarction the patient will be discharged with an average of 6 to 10 pills. Taking into account that most of these patients are older individuals, many of whom have comorbidities that require treatment with other drugs, it is common to find patients with therapeutic regimens that make adherence difficult. If we want to translate the effectiveness shown by the drugs in clinical trials to a true efficacy in real life, it is essential to introduce measures that facilitate rational administration of these me dications. These measures could include the discontinuation of drugs with a marginal benefit in a given patient or the use of formulations that combine active ingredients.
ComplicationsHeart Failure and ShockIn this section, Table 23 of the guidelines summarizes a total of 29 recommendations (8 more than in the preceding guidelines), most of which are based on consensus and thus have the lowest level of evidence (C), as there are no specific references in the literature.
The need for echocardiography is strongly emphasized by the use of the imperative “must be performed.”
The use of sodium nitroprusside in the treatment of hypertension and the combination of hydralazine and isosorbide dinitrate in patients with heart failure who cannot take angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are recommendations that had not been included in previous guidelines. The data from 2 very recent randomized studies include the recommendation that norepinephrine be utilized for shock, in which it is preferred over dopamine (IIb B). The use of levosimendan, a costly drug whose efficacy in comparison with that of other inotropic agents has not been irrefutably demonstrated, continues to be highly controversial. The guidelines accord it the lowest class of recommendation and level of evidence admissible in Killip class III (IIb C), behind dopamine and dobutamine. Given its mechanism of action (independent of beta-adrenergic stimulation), its possible use in patients who have been treated with beta-blockers is mentioned.
On the basis of 2 recent meta-analyses, the grade of recommendation of the use of intra-aortic balloon pump counterpulsation has been lowered from class I to class IIb B. The publications of these guidelines nearly coincided with that of the largest randomized study on balloon counterpulsation to date.8 In a series of 600 patients with cardiogenic shock after myocardial infarction, who were going to undergo revascularization, counterpulsation did not reduce 30-day mortality. It should be taken into account that the follow-up in this study was very short and that 40% of the patients included had previous cardiac arrest (possible distributive shock, in which balloon counterpulsation is not beneficial). Nonetheless, this new information, which was not available when the guidelines were drawn up, calls into question the utility of intra-aortic balloon counterpulsation in general. In our opinion, studies performed in general contexts should not rule out the indication for this technique for certain individual patients, given the extensive positive experience accumulated over the years. The decision should be made quite early, to avoid the development of irreversible multiple organ failure, and by cardiologists with extensive experience in the care of patients of this type. We expect that it will be possible to define the subgroups of patients who can benefit from intra-aortic balloon pump support in the near future. Further on, the guidelines refer to the stabilizing role of balloon counterpulsation in the mechanical complications of myocardial infarction (severe acute mitral regurgitation and ventricular septal defect).
The grade of recommendation of the use of a ventricular assist device in the management of refractory shock has also been reduced (from IIa C to IIb C), on the basis of a meta-analysis involving the Tandem Heart and Impella systems 2,5. These systems, which did not reduce 30-day mortality compared to balloon counterpulsation, may not be the most suitable devices at the present time.
The guidelines pay very little attention to ultrafiltration, although they support it with a considerable grade of recommendation (IIa B) in cases of volume overload refractory to diuretics, especially in the presence of hyponatremia.
Other ComplicationsThere are no novel inputs with respect to arrhythmias. The guidelines insist on the need to carefully weigh the indication for coated stents in patients who should continue to receive anticoagulation therapy for atrial fibrillation. Nor are there important developments concerning the management of ventricular arrhythmias. The relationship between the development of malignant arrhythmias after the acute phase (24-48 hours) and a poor prognosis in patients with a markedly reduced LVEF should also be pointed out. Revascularization probably cannot prevent recurrence in these cases, even though the original arrhythmia may have been related to a transient ischemic attack . Under these circumstances, the placement of an implantable cardioverter-defibrillator is a IA recommendation.
The guidelines still fail to provide specific recommendations as to the best time for the surgical repair of postinfarction ventricular septal defects. Given the higher mortality rate associated with inferobasal defects, we feel that surgery should be considered earlier, even in the absence of confirmed evidence.
The incidence of ventricular mural thrombi has decreased significantly with improvements in reperfusion therapy. We have no recent data on the duration of anticoagulation therapy in these cases. The guidelines propose that, at the present time and taking into account the combination of dual antiplatelet therapy and anticoagulation, the latter can be discontinued earlier than 6 months if an imaging technique at 3 months demonstrates that the thrombus has disappeared.
Conflicts of InterestCoordination of the Spanish nationwide clinical trial PLATO: Astra-Zeneca (MH). Clinical Commitee endpoint: Eli-Lilly (AB). Research grants awarded to the institution: Abbot-Vascular (AC), Boston Cientific (AC), GSK (MH), Medtronic (AC). Consultancies: Abbott (MS), Astra-Zeneca (AB, JB, JL-S, MS, MH), Bayer (AB, AF, JB), Boheringer-Ingelheim (FW), Boston Scientific (IL), Chiesi (JB, FW), Cordis (MS), Daiichi-Sankyo (JB, AF, JL-S, FW), Eli-Lilly (AF, MS), Ferrer (AF), Medtronic (MS), MSD (AF), Rovi (AB), Sanofi (IL). Educational reports and presentations: Abbott (AC, AF), Astra-Zeneca (AC, AF, J-L S, MH), Bayer (AC, JL-S, MP, MH), Biotronic (AC), Boheringer-Ingelheim (JL-S, FW, MH), Chiesi (AF, FW), Daiichi-Sankyo (AC,AF, JL-S, FW), Eli-Lilly (AF, MH), Ferrer (AC,AF), GSK (AF), Menarini (JL-S, MH), MSD (AF, FW), Roche (AF), Rovi (MH).
| Coordinators: |
| Fernando Worner |
| Angel Cequier |
| Spanish Society of Cardiology Working Group on the Clinical Practice |
| Guidelines for ST-Elevation Acute Coronary Syndrome: |
| Alfredo Bardají |
| Vicente Bodí |
| Ramón Bover |
| Manuel Martínez-Sellés |
| Manel Sabaté |
| Alejandro Sionis |
| Manuel Vázquez de Prada |
| Group of Expert Reviewers for the Clinical Practice Guidelines for ST-Elevation Acute Coronary Syndrome: |
| Fernando Arós |
| Fernando Arribas |
| José Barrabés |
| Oscar Díaz de Castro |
| Magda Heras |
| Ramón López Palop |
| José Luis López-Sendón |
| Nicolás Manito |
| M. Carmen de Pablo |
| Tomás Ripoll |
| Alberto San Román |
| José M. de la Torre |
| Spanish Society of Cardiology Clinical Practice Guidelines Committee: |
| Antonio Fernandez-Ortiz (President) |
| Ángel M. Alonso Gómez |
| Manuel Anguita |
| Angel Cequier |
| Josep Comín |
| Isabel Diaz-Buschmann |
| Ignacio Fernández Lozano |
| José Juan Gómez de Diego |
| Manuel Pan |
| Fernando Worner |