Pneumonectomy significantly alters the position of the heart, thereby hindering implantation of a conventional pacemaker. In addition, there is limited evidence of the feasibility of leadless pacemakers in patients with pneumonectomy syndrome.
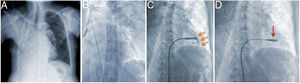
We present the case of a 64-year-old woman who, 10 years previously, had undergone pneumonectomy for polycystosis and invasive ductal carcinoma (figure 1A). The patient also underwent bilateral mastectomy and had received chemotherapy and radiotherapy. She had permanent and symptomatic atrial fibrillation. Drug therapy could not satisfactorily control ventricular response while ventricular function was preserved. She was referred for atrioventricular (AV) node ablation and pacemaker implantation. Given the high risk of implanting a conventional device, a leadless option was chosen; ablation was to be performed during the same procedure.
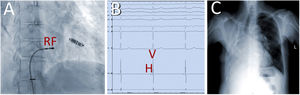
First, the leadless pacemaker was implanted with right femoral venography to guide the procedure. The device was advanced to the right ventricle and deployed with monitoring in the anterior view, while control of the degree of apposition to the right ventricular endocardium was monitored by contrast injection in 2 orthogonal views (figure 1B,C, video 1 of supplementary data). After initial midseptal deployment, excellent pacing and sensing parameters were observed (figure 1D, video 2 of supplementary data). After withdrawal of the Micra deployment system, and with a telescopic 14-Fr introducer in the long introducer, compact AV node ablation was performed with radiofrequency (RF). The junctional escape rhythm was 40 bpm, with normal His-ventricular (HV) interval (figure 2A-C, video 3 of supplementary data).
Performing the 2 procedures simultaneously seems to be a feasible and safe alternative in patients with complex anatomy and avoids potential complications.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.04.028