Keywords
INTRODUCTION
The involvement of the right ventricle (RV) in hemodynamic stability and in the maintenance of an adequate cardiac output has been underestimated for decades. However, scientific evidence has demonstrated the fundamental role of the systolic function of RV in the course of a number of diseases. For some time now, we have been aware of the prognostic value of this parameter in congenital heart diseases, in which its influence is largely explained by anatomical variations that confer on the right chambers a greater prominence in the systemic circulation.1,2 However, the prognostic importance of right ventricular systolic function in other conditions that are encountered more frequently in routine clinical practice, such as heart failure,1,3 pulmonary hypertension,3,4 pulmonary thromboembolism,1,3,5 and myocardial infarction,2,3 has recently been stressed. Thus, in this context, the availability of a simple, reproducible and accurate method for evaluating the output of RV in routine clinical practice is essential.
Right ventricular systolic function can be assessed by means of different imaging techniques used in cardiology: two-dimensional and three-dimensional echocardiography, angiography, radionuclide ventriculography and magnetic resonance. Of these, that which is most readily available and widely utilized in routine clinical practice is two-dimensional echocardiography, which, moreover, is inexpensive and risk-free. The availability of an echocardiographic parameter that enables a simple and reproducible estimate of right ventricular systolic function continues to be one of the great challenges in echocardiography.
The purpose of the present study is to assess the inter- and intra-observer variability in different echocardiographic parameters for the analysis of the function of RV to aid in determining those that show the highest reliability.
METHODS
All the patients admitted to our center to undergo isolated mitral valve surgery were consecutively enrolled in the study. Those patients with concomitant coronary artery disease or aortic valve disease were excluded.
An echocardiographic system (Vivid 3, General Electric) equipped with a 1.5 to 3 MHz transducer was employed. The images were analyzed in the workstation of our central image-processing unit using the Echo Pac 3.1.0 software package.
Two researchers, working independently, performed transthoracic echocardiography in all the patients included in the study within a period of less than 24 hours to avoid differences attributable to a variation in the fluid status and, thus, in preload. Subsequently, following an interval of between one and three months, and on the basis of images recorded in the echocardiographic system, one of the researchers again analyzed the echocardiographic parameters being studied to obtain the intra-observer variability.
The measurements of right ventricular function included in the analysis were the tricuspid annular plane systolic excursion (TAPSE), tricuspid annular peak systolic velocity on tissue Doppler imaging (TDPV), fractional shortening of right ventricular diameters (FS-dia), fractional shortening of the right ventricular outflow tract (FS-RVOT) and fractional shortening of right ventricular areas (FS-area). The recording of each parameter was carried out according to the guidelines of the American Society of Echocardiography6 and those provided in the studies that endorsed the use of each of these parameters.2,6-16
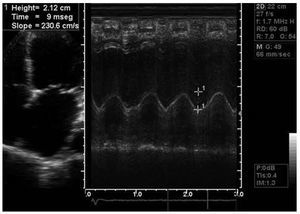
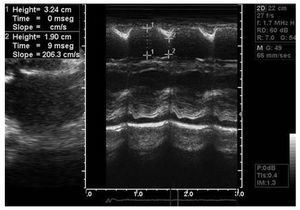
The TAPSE was calculated in M mode in the apical four-chamber view.2,8,9 The cursor was placed at the junction between the tricuspid annulus and the lateral wall of RV. The TAPSE is defined as the systolic displacement of said point along the vertical axis with respect to the baseline situation, which represents the longitudinal shortening of the ventricular base with respect to the apex (Figure 1).
Figure 1. Tricuspid annular plane systolic excursion in apical four-chamber view.
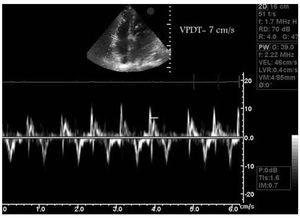
The TDPV was obtained in the apical four-chamber view and in pulsed tissue Doppler mode by placing the cursor at the junction between the base of the anterior cusp of the tricuspid valve and the lateral wall of RV.9,10 In this way, tissue Doppler provided a series of systolic and diastolic deflections. The first systolic peak represents the isovolumetric contraction and, thus, was discarded, and the TDPV was considered to be the maximum value of the next systolic deflection (Figure 2).
Figure 2. Tricuspid annular peak systolic velocity on tissue Doppler imaging (VPDT) in apical four-chamber view.
The proper calculation of TAPSE and TDPV requires the correct placement of the cursor, whether in M mode or in pulsed tissue Doppler mode, in such a way that it lies parallel to the longitudinal movement of the tricuspid plane. The angulation of the cursor with respect to the displacement of the ventricular base results in a significant underestimation of its measurement.16 For both TAPSE and TDPV, the mean of three beats was taken if the patient was in sinus rhythm and the mean of 5 beats was used in patients with atrial fibrillation.
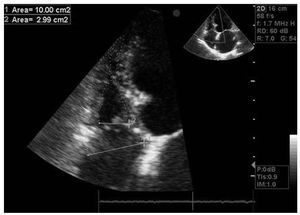
The FS-area was calculated in the apical four-chamber view applying the following formula (Figure 3)6,8,13-15:
Figure 3. Fractional shortening of right ventricular areas in apical four-chamber view.
(diastolic area - systolic area) / diastolic area (in %)
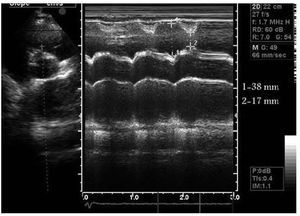
The calculation of the FS-RVOT required a perpendicular section along the parasternal short axis of the outflow tract at the level of the aortic valve.11 In M-mode, we obtained the maximum diastolic diameter and the minimum systolic diameter and applied the following formula, the result of which is expressed in percentage (Figure 4):
Figure 4. Fractional shortening of right ventricular outflow tract on parasternal short axis.
(maximum diastolic diameter - minimum systolic diameter) / maximum diastolic diameter
The calculation of the FS-dia was based on the end-systolic and end-diastolic diameters obtained in M-mode at the level of the papillary muscles in the parasternal long axis.12 It is expressed as a percentage, calculated by means of the formula (Figure 5):
Figure 5. Fractional shortening of right ventricular diameters on parasternal long axis.
(end-diastolic diameter - end-systolic diameter) / end-diastolic diameter
With the measurements recorded for each of these parameters, the intraclass correlation coefficient was determined for both the inter- and intra-observer variability. The relationship between the strength of agreement and the intraclass correlation coefficient values is shown in Table 1.17-19
The SAS V8.2 statistical software package (Statistical Analysis Software Institute Incorporated, Cary, North Carolina, United States) was utilized to calculate the intraclass correlation coefficient.
RESULTS
The study population, enrolled between October 2006 and November 2007, was comprised of a total of 30 consecutive patients who were scheduled to undergo isolated mitral surgery, all of them in the same hospital.
The majority of the patients were women, and the mean age was 67 years. The most common etiology of the mitral valve disease was rheumatic. In most of the cases, it presented as severe mitral insufficiency with severe pulmonary hypertension. Left ventricular function was preserved in the majority of the patients. The most relevant demographic, clinical and echocardiographic characteristics are summarized in Table 2.
The analysis of the FS-dia could not be carried out in six patients since it was not possible to obtain a suitable image that would enable the perpendicular section of RV at the level of the papillary muscles. Moreover, in one of these patients it was impossible to study the FS-RVOT due to a deficient parasternal acoustic window. The strength of the agreement in the inter- and intra-observer analysis for each of the measurements analyzed is shown in Table 3.
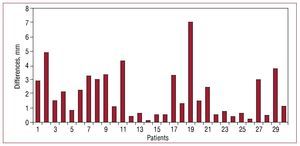
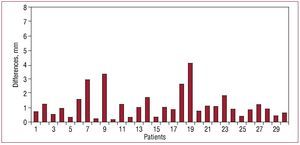
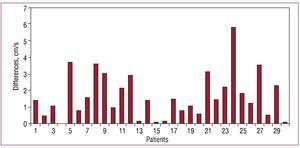
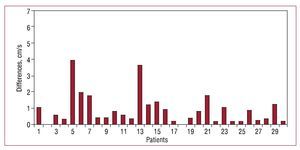
According to our results, TAPSE and TDPV were the parameters that showed the strongest agreement. The intraclass correlation coefficient was good for the inter-observer analysis and excellent for the intra-observer analysis in both measurements. In contrast, the FS-dia, the FS-RVOT and the FS-area exhibited a significantly low strength of agreement (0.27-0.51) both in the measurements performed by the 2 researchers and in those carried out by the same individual. The absolute and relative differences found in these measurements are summarized in Table 4. These values are presented in bar graphs (Figures 6-9) for TAPSE and TDPV, the parameters with the strongest agreement.
Figure 6. Absolute differences in inter-observer measurements of tricuspid annular plane systolic excursion.
Figure 7. Absolute differences in intra-observer measurements of tricuspid annular plane systolic excursion.
Figure 8. Absolute differences in inter-observer measurements of tricuspid annular peak systolic velocity using tissue Doppler imaging.
Figure 9. Absolute differences in intra-observer measurements of tricuspid annular peak systolic velocity using tissue Doppler imaging.
To determine the clinical relevance of the differences observed in the inter- and intra-observer measurements for TAPSE and TDPV, we considered 15 mm for TAPSE2,6 and 12 cm/s for TDPV2 as cutoff points to define normality.
We then categorized the results as normal if they were equivalent to or higher than the preestablished cut-off point and as indicative of disease if they were lower. With respect to TAPSE, the researchers differed as to the category to which to assign the patient in only 2 cases (7%), and 3 patients (10%) were assigned to different groups by the same observer; with regard to the TDPV, 5 patients (17%) were classified in different categories by each of the researchers and 2 (7%) were placed in 2 different groups by the same observer.
DISCUSSION
Undoubtedly, it is necessary to obtain information on right ventricular systolic function for clinical decision-making and for the evaluation of the prognosis in patients with different cardiovascular diseases. There are a number of imaging techniques for evaluating right ventricular function; of these, that most widely used in routine clinical practice is two-dimensional echocardiography. However, the echocardiographic evaluation of RV is far from perfect, and there is no echocardiographic parameter reliable enough to be universally accepted.
The difficulties involved in the echocardiographic assessment of RV start with its complex anatomy. In contrast to left ventricle, there is no geometric model that enables an estimate of its volumes on the basis of a 2-dimensional measurement. Other peculiarities of RV that limit its assessment by means of ultrasound are: a) its retrosternal position, with the resulting difficulty in the visualization of the anterior segments; b) the poor demarcation of the endocardial border, which is compromised by the marked trabeculation of its myocardium, especially in the apical segment; and c) the significant influence of preload and afterload on the systolic function of the RV, which entails certain variability in its analysis and, thus, an obstacle for the validation of certain measurements.
Cardiac magnetic resonance has successfully overcome many of the limitations of echocardiography; thus, at the present time, it is considered to be the technique of choice for the morphological and functional analysis of RV.20 Nevertheless, it requires complex and costly technical and computing equipment that is not available in all hospitals. On the other hand, magnetic resonance can not be performed in the growing group of patients with intracardiac devices, such as pacemakers and defibrillators, that are sensitive to magnetic fields. Finally, the analysis of the RV is a painstaking study that requires personnel with expertise and takes time, a circumstance that comes to be one more limitation to the routine use of magnetic resonance in the assessment of RV.7
In recent years, different echocardiographic parameters have been proposed to estimate right ventricular systolic function. Among those that have had the greatest impact are TAPSE, TDPV, FS-area, FS-RVOT and FS-dia. According to the results of our study, of the parameters analyzed, TAPSE and TDPV are those that exhibit the strongest agreement in both intra- and inter-observer measurements, while FS-dia, FS-RVOT and FS-area show poor inter- and intra-observer agreement. It is interesting to see that the FS-dia, FS-RVOT and FS-area present an intraclass correlation index below that acceptable even for measurements made by a single observer. We can interpret this fact to be an additional indicator of their marked variability.
Right ventricular function as estimated by means of TAPSE presents an excellent correlation with the ejection fraction calculated using radionuclide ventriculography and magnetic resonance, as a number of studies have shown.8,9,12 The TAPSE is not only proving to be one of the most useful parameters in the assessment of right ventricular function, but likewise has demonstrated its prognostic implication in patients with advanced heart failure.21 A similar situation occurs with the TDPV, which shows a significant correlation with radionuclide ventriculography9,10 and with magnetic resonance13 and, in addition, constitutes an independent prognostic factor in heart failure.22
The results of our study agree with recent publications in which the inter- and intra-observer variability in the estimate of TAPSE and the TDPV are similar to those found in our analysis.10,16
It is important to point out that, in our study group, 70% of the patients had atrial fibrillation at the time of the echocardiogram. This fact is of interest since the first trials that validated the TDPV designated the absence of sinus rhythm as an exclusion criterion.10,22 In our study, the presence of atrial fibrillation did not affect the excellent reproducibility of TAPSE and the TDPV.
In recent studies, the FS-area has exhibited a significant degree of correlation with the ejection fraction as calculated by magnetic resonance13-15 and radionuclide ventriculography.8 However, the difficulty with endocardial demarcation, especially of the anterior segments due to their retrosternal position, results in a high variability and poor agreement in the intra- and inter-observer measurements, a characteristic that had already been reported in earlier studies.13
The FS-RVOT is a parameter that is easy to obtain; there was only one case in which it was not possible to calculate it due to a deficient parasternal acoustic window. However, according to the data in our study, it does not qualify as a reproducible parameter. These findings are not confirmed by previous publications,11 in which the results in terms of variability were better. This disagreement might be attributed to differences between the study groups, and future studies will probably be required to determine that or those populations in which the variability does not limit its utilization.
The FS-dia has been found to be highly dependent on the quality of the acoustic window given that, in 20% of the patients, it could not be calculated. This is the first study that analyzes the intra- and inter-observer variability of the FS-dia. According to our results, its reproducibility is not good and, thus, the estimate of right ventricular function by this method is not reliable.
The impossibility of calculating the FS-RVOT and the FS-dia in certain patients indicates the importance of the acoustic window in the measurement of these parameters. The parasternal image is difficult to obtain in some cases, a circumstance that is considered to be an additional limitation to the generalization of the use of the two measurements. On the other hand, the absence of an apical acoustic window is exceptional, a fact that facilitates the determination of TAPSE, TDPV and FS-area.
Limitations
Our study basically presents 2 limitations: the fact that it was carried out in patients with isolated mitral valve disease and, thus, our results are applicable exclusively to this clinical context; and the fact that the number of patients is small. However, the excellent agreement values obtained for TAPSE and TDPV indicate that they are highly reproducible parameters for the assessment of right ventricular systolic function. Studies with larger groups of patients and in other clinical contexts will be necessary in order to be able to apply our conclusions on a general basis.
CONCLUSIONS
TAPSE and TDPV are the echocardiographic parameters with the lowest inter- and intra-observer variability, a fact that makes them the most reliable and reproducible parameters for the assessment of right ventricular systolic function in patients with isolated mitral valve disease.
ABBREVIATIONS
FS-area: fractional shortening of right ventricular areas
FS-dia: fractional shortening of right ventricular diameters
FS-RVOT: fractional shortening of right ventricular outflow tract
RV: right ventricle
TAPSE: tricuspid annular plane systolic excursion
TDPV: tricuspid annular peak systolic velocity on tissue Doppler imaging
This study has been funded in part by the Red Cooperativa de Investigación Cardiovascular (RECAVA), division of the Instituto de Salud Carlos III, Spain
Correspondence: Dr. M. Pinedo.
Secretaría de Cardiología. Hospital Clínico Universitario. Avda. Ramón y Cajal, 3, 7.a planta. 47005 Valladolid. Spain.
E-mail: mpinedog@gmail.com
Received August 14, 2009.
Accepted for publication January 26, 2010.