In recent years, cardiac imaging has advanced technologically, and patients with cardiovascular disease have become increasing more complex. This has led to the development of multimodal imaging, that is, the integration of several different imaging techniques with a single objective: to establish a precise diagnosis of the disease, in order guide treatment and predict prognosis throughout the patient's follow-up. In addition to the 2 classic cardiological investigations—echocardiography and myocardial perfusion scintigraphy—other more modern and complex complementary techniques have been developed, such as cardiac magnetic resonance imaging, computed tomography, and positron emission tomography in its different modalities: positron emission tomography-computed tomography, and positron emission tomography-magnetic resonance imaging. Each of these options has its indications for appropriate use,1,2 and they are widely used in the diagnosis of coronary artery disease, valvular disease, heart failure, congenital heart disease, and arrhythmias.
The development of such investigations in the field of cardiovascular disease has been accompanied by their increased availability in health care facilities and an increased demand for them. Consequently, the number of procedures that patients undergo has increased markedly. Therefore, cardiac imaging units have become core units in hospitals, with a high caseload; often they do not have an actual physical structure, but are a functional entity organized between the radiology and cardiology services. In addition, interest has grown in minimally invasive techniques for the treatment of cardiovascular disease—transcatheter aortic valve implantation, transcatheter treatment of mitral regurgitation (MitraClip), left atrial appendage obliteration, and closure of prosthetic leaks, intracardiac shunts, and congenital heart defects. This means that imaging techniques are now indispensable for monitoring procedures and interventions and assessing the outcomes.
The above factors have all contributed to a significant increase in health care spending, with cardiovascular imaging techniques being one of the main reasons for such a trend. A recent editorial article on the subject reported that in recent years, health care costs in patients with cardiovascular disease had increased by almost 4,8% per year.3 Although there were marked differences between the United States and Spain, the article describes the significant increase in the health care costs of cardiovascular disease between 2000 and 2006, which leapt from 1.6 billion dollars to 5.1 billion dollars.3,4
To reduce healthcare spending and minimize patient risk, cardiac imaging techniques must be used efficiently, which means avoiding overuse and underuse. Overuse, or abuse, is when an investigation does not lead to an improvement in the patient's treatment or prognosis5 and is associated with an increased patient risk (from radiation, contrast, or use of pharmacological stressors) or a delayed diagnosis in another patient who would have benefited from that investigation. In contrast, underuse is characterized by an incomplete or incorrect diagnosis with negative consequences for the patient.
One of the main reasons for using cardiac imaging techniques is the need to reach a correct diagnosis and optimize treatment promptly. In a social setting of limited resources, the appropriate use of an investigation in one patient may be delayed by the inappropriate use of that investigation in another patient. The second individual might have benefited from a different, more appropriate investigation. To minimize this problem, guidelines on the appropriate use of the different investigations are extremely useful. Such guidelines describe the indications and limitations of the various techniques and allow the correct choice of investigation for each patient, maximizing the benefit and minimizing the risk, which is essentially the concept of patient-centered medicine. This concept, which involves adapting clinical practice guidelines to the individual, has evolved greatly in recent years. This effective practice requires an in-depth knowledge of not only cardiovascular disease, but also of cardiac imaging techniques: different tests are indicated for screening an asymptomatic patient than for diagnosing a patient with symptoms, or for monitoring treatment response. Consequently, the usefulness of a particular diagnostic test will vary between distinct populations and within each population between different subjects, according to the pretest probability of having a certain condition.6 When different diagnostic options are equally valid for a particular patient, the indicated method should be that which is the safest and most efficient for that particular patient.
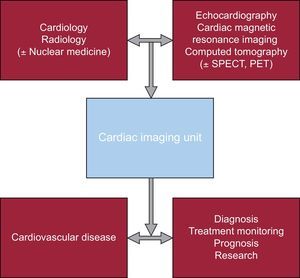
ORGANIZATION OF CARDIAC IMAGING UNITSFrom the points above, it stands to reason that the ideal organizational model for cardiac imaging units is that in which decisions on the various clinical processes constituting cardiovascular disease are made by a multidisciplinary team, which includes physicians from different specialties. The joint organization of functional cardiac imaging units formed by cardiac imaging specialists and radiologists allows the professionals involved to work as a team, optimizing the use of new imaging techniques to better understand cardiovascular anatomy and physiology. Ideally, nuclear medicine should be integrated in multidisciplinary cardiac imaging units. However, given the differences between distinct countries and hospitals in the use and level of development of nuclear medicine, the decision to include nuclear medicine should take into account the particular situation of each health care facility. In patients with cardiac disease, such a model provides maximum efficiency in solving diagnostic problems, allows treatment monitoring, improves prognosis, and contributes, in turn, to promoting research in this field (Figure).6
Diagram representing the multidisciplinary organization of functional cardiac imaging units. Several cardiac imaging specialists must work together to make an impact on cardiovascular disease, optimizing the diagnosis, treatment monitoring, improving the prognosis, and encouraging basic and clinical research. PET, positron emission tomography; SPECT, single photon emission computed tomography.
This process is strengthened by a change in the diagnostic expertise and organization of such units: this means a transition from a unit made up of physicians specialized in one particular imaging technique to a more heterogeneous unit composed of different specialists, each with specific expertise on a different imaging technique or techniques, all based on a common organ or system. Such a model allows the medical team to choose the most appropriate test according to the individual characteristics of each patient.
One of the cardiac imaging techniques that has been most developed in recent decades is cardiac magnetic resonance imaging. This technique complements the information obtained from the classic investigations in cardiovascular disease and provides essential information for the diagnosis and prognostic stratification of various cardiovascular diseases. Therefore, it is essential to have the appropriate technology and for the medical staff to be sufficiently trained and skilled, with experience in both the technical aspects of cardiac magnetic resonance imaging and the clinical aspects of cardiovascular disease.
The standards for training and accreditation of the medical professionals that perform and report cardiac magnetic resonance studies have been clearly established by various international scientific societies and working groups.7,8 In Spain, the Spanish Society of Cardiology and the Spanish Society of Medical Radiology recommend the creation of multidisciplinary heart disease units or committees, under the coordination and supervision considered most functional in each case, taking into account the characteristics of each center.9 Such units would be required to develop comprehensive, rationalized protocols on cardiac imaging, with the aim of obtaining better diagnostic and therapeutic efficiency for each cardiac patient. This would avoid the redundancy of unnecessary investigations and procedures that significantly increases spending and resource use.
The Spanish Society of Cardiology and the Spanish Society of Medical Radiology have produced an important joint document. Unlike those of other national and international scientific societies, this pioneering document regulates the operating of cardiac imaging units. The aim of the document is to coordinate all of the above organizational points for cardiac imaging units, to establish the indications for cardiac magnetic resonance imaging, to standardize reporting, and to standardize the training, accreditation, and competency of the different cardiac imaging specialists. The document stresses the importance of a consensus between specialties, by creating joint criteria that allow advances to be made in the rational and efficient use of imaging techniques.9
TRAINING AND ACCREDITATION OF CARDIAC IMAGING UNITSThe significant increase in the number of cardiac imaging techniques in recent decades has helped to markedly improve the management of cardiovascular disease; however, it also represents a challenge to the training of cardiac imaging specialists.
In Spain, as in many other countries, there is no standardized training program for cardiac imaging. Therefore, the training of cardiology residents and fellows depends on experience and the most frequently-assessed conditions in those hospitals.10 However, developments in modern medicine require most cardiac imaging specialists to be able to use multiple imaging techniques.11 To standardize training, it is recommended that cardiac imaging specialists are accredited by the national or an international scientific society that corresponds to their specialty. Therefore, the European cardiology and radiology societies have an accreditation system for specialists who meet the standards set in terms of both training time and the number of cases seen and who, finally, pass a theory test to support their expertise. The standards for training and accreditation of cardiac imaging professionals in Spain are described in the consensus document of the Spanish Society of Cardiology and the Spanish Society of Medical Radiology.9
Cardiac imaging specialists are faced with various challenges. They must be proactive in encouraging different cardiac imaging programs and training channels and provide opportunities to fellows and residents in training. Another significant challenge is the presence of nonmedical factors that affect the diagnostic process. The availability and cost of an investigation, the health care patterns, and other, individual factors, some of which relate to the level of the professionals’ training, can determine how often an investigation method is used. Therefore, it is essential to establish an efficient, patient-centered model, which selects only the techniques that best suit the individual patient.
In addition, to establish a high quality of care, it is not only the specialists who need adequate training; there should also be an accreditation system for hospitals, especially in cardiac imaging units, to ensure the availability of the appropriate technology, optimal investigation protocols, and compliance with safety standards to avoid unnecessary risk to patients.
Finally, cardiac imaging units are one of the essential pillars necessary for basic and clinical research. Cardiovascular imaging is an essential tool in the field of cardiovascular disease, both in making an early diagnosis and in assessing disease progression. The development of the best basic science should be combined with the best imaging techniques. In addition, by standardizing specialist training, investigation protocols between different centers, and interpretation of results, multicenter and population-based studies can be developed, which constitute the backbone of translational research, particularly its clinical and epidemiological aspects.
In modern medicine, the use of imaging techniques in diagnostics is a world of exciting challenges and has undoubtedly been one of the most spectacular advances in medical history.12,13 Imaging techniques extend to almost all areas of medicine, not only in diagnostics, but also in the understanding of pathophysiology, prevention, treatment, prognosis, and research into the various cardiac diseases.14 The establishment of joint protocols such as those proposed by the Spanish scientific societies9 are essential and promote the rational use of imaging techniques in cardiology; this will benefit our health systems and, ultimately, the patient, which is the whole point of medical practice.
CONFLICTS OF INTERERSTNone declared.