Secondary prevention in myocardial infarction patients is paramount to prevent recurrences. Dual antiplatelet therapy has been shown to reduce the risk of subsequent events up to 1 year and beyond in the PEGASUS-TIMI 54 trial. This study aimed to estimate the annual number of myocardial infarction patients with PEGASUS characteristics in Spain and to analyze short- and long-term outcomes in these patients.
MethodsThe number of myocardial infarction patients was estimated assuming a Poisson distribution. Myocardial infarction incidence and mortality rates obtained from population registries (IBERICA and REGICOR) were properly adjusted. The proportion of myocardial infarction patients with PEGASUS characteristics was estimated with a REGICOR cohort of consecutive patients from 2003-2009 (n=1391). This cohort follow-up was used to compare the occurrence of reinfarction and death at 1 year and at the end of the follow-up (4.7 years) in patients with and without PEGASUS characteristics by Cox regression.
ResultsThe estimated annual number of stable myocardial infarction patients aged ≥ 50 years and without bleeding events was 41 311. Of these, 22 493 had at least 1 PEGASUS characteristic (diabetes, previous myocardial infarction, or chronic kidney disease). At 4.7 years of follow-up, having any PEGASUS characteristic or age ≥ 65 years was associated with a higher risk of cardiovascular and all-cause death in adjusted analyses (hazard ratio=3.44 and 2.21, 95% confidence interval, 1.22-9.74 and 1.11-4.42, respectively).
ConclusionsIn Spain, more than 50% of the stable myocardial infarction patients aged ≥ 50 years are estimated to have at least 1 PEGASUS characteristic, which substantially increases the long-term risk of cardiovascular and all-cause death.
Keywords
Coronary heart disease (CHD) is the single most common cause of death in Europe, and acute myocardial infarction (AMI) is its major contributor. In Spain, nearly 100 000 individuals have an AMI each year, and 33% die before reaching a medical facility.1 For hospitalized AMI patients, 28-day case-fatality is 13%,1 and for those surviving the first 28-days, 2-year coronary event incidence is 12.6%.2
Aspirin effectively prevents recurrences in patients with a prior coronary event. Dual antiplatelet therapy (DAPT), with aspirin and P2Y12-inhibitors (eg, clopidogrel, prasugrel, ticagrelor) further reduces the risk of subsequent coronary events in high-risk patients up to 1 year.3–6 Recently, the PEGASUS-TIMI 54 trial showed that aspirin+ticagrelor beyond 1 year reduced the primary combined end point of cardiovascular death, AMI, or stroke in AMI patients but increased the risk of major bleeding.7
Patients included in the PEGASUS trial were stable AMI patients aged 50 years and older, with at least 1 of the following risk factors: diabetes, a second previous AMI, multivessel CHD, chronic kidney disease (CKD) or age ≥ 65 years.8 Due to the scarcity of data on stable AMI patients and the effectiveness of aspirin+ticagrelor in high-risk AMI patients, it would be useful to determine how many AMI patients could benefit from this therapy beyond the first year after the event and to identify the long-term risk of these patients.
In the present study, we aimed first to estimate the annual number of stable AMI patients with PEGASUS characteristics in Spain. Secondly, we aimed to compare, in stable AMI patients with and without PEGASUS characteristics, the risk of AMI and death during the second year after the index AMI, and at the end of the follow-up (4.7 years).
METHODSStudy DesignTo estimate the annual number of stable AMI patients with PEGASUS characteristics, we used data from 2 population-based AMI registries: IBERICA,9 conducted in 1997-1998 in 7 Spanish regions, and REGICOR,10 conducted in 1990-2009 in Girona province.
Patients with AMI were classified as having PEGASUS characteristics if they were ≥ 50 years old and had previous AMI, diabetes or CKD, or were at least 65 years old. Multivessel CHD was not taken into account because the information was missing for 60% of the patients. Previous AMI was based on clinical history and information reported in standardized questionnaires. Diabetes was based on clinical history, treatment, and fasting glucose value > 6.9 mmol/L (125mg/dL). Chronic kidney disease was based on the estimated glomerular filtration rate (< 60mL/min/1.73m2), calculated with the Modification in Diet in Renal Disease formula.
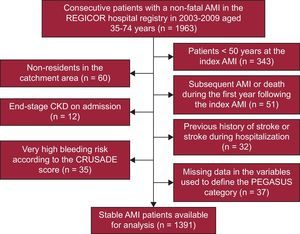
For the comparison of short- and long-term outcomes in stable AMI patients with and without PEGASUS characteristics, we used a cohort study of consecutive AMI patients aged 35-74 years included in the REGICOR reference hospital in 2003-2009. To obtain a population of stable AMI patients similar to the population of the PEGASUS trial, we excluded patients younger than 50 years, patients who died or had a subsequent AMI in the year following the index event, patients with end-stage CKD (estimated glomerular filtration rate < 15 mL/min/1.73 m2), patients who were classified at a very high risk of bleeding by the CRUSADE risk score, and patients with history of ischemic or nonclassifiable stroke (before the AMI and during the first year post-AMI). We also excluded patients for whom the PEGASUS category could not be defined. Baseline was defined as the index AMI date plus 1 year, and thus, the follow-up to determine the occurrence of cardiovascular events and death began 365 days after the index AMI.
The REGICOR study complies with the Declaration of Helsinki and was approved by the local ethics committee. All AMI patients included were duly informed and signed a consent form to participate in the registry.
Outcomes and Variables for Prognosis AnalysisThe incidence of AMI, cardiovascular death, noncardiovascular death, all-cause death, and the composite AMI/all-cause death was analyzed at 1 year and at a median of 4.7 years of follow-up in PEGASUS and non-PEGASUS stable AMI patients. The self-reported incidence of stroke was only examined in the crude analysis, as the information was only available for 43% of the included patients.
The variables used for descriptive and/or adjustment purposes were age, sex, hypertension (based on clinical history, treatment, and observed systolic/diastolic blood pressure > 140/90mmHg), hypercholesterolemia (based on clinical history, treatment, and observed total-cholesterol > 200mg/dL), smoking (smokers were defined as persons currently smoking or quitting < 1 year previously), history of angina, heart failure (based on the New York Heart Association functional classification and considered if II-IV), ST-segment elevation, angiography, reperfusion (including thrombolysis and percutaneous coronary intervention), post-AMI arrhythmia (including ventricular fibrillation and tachycardia), post-AMI angina, left ventricular ejection fraction, maximum Killip class, prescription of evidence-based drugs in-hospital and at discharge (angiotensin-converting enzyme [ACE] inhibitors/angiotensin receptor blocker [ARB], beta-blockers, lipid lowering drugs, antiplatelet drugs).
Statistical AnalysisIBERICA registry estimates, adjusted for clustering and for the 2000 AMI definition change,11 were used for the population aged 45-74 years, under the assumption that the incidence of AMI did not change substantially in the last 17 years.12 The REGICOR registry was used to estimate AMI incidence in the population > 74 years, which was weighted for the expected difference between incidence rates from Girona and Spain observed in the IBERICA Study (Table 1 of the supplementary material). The AMI mortality rates were obtained from the REGICOR registry, as Girona's AMI mortality estimates have been demonstrated to be a robust estimate of Spanish AMI mortality1 (Table 1 of the supplementary material). The annual number of hospitalized stable AMI patients aged ≥ 50 years was calculated using the estimated incidence rates and discounting mortality and bleeding rates. Bleeding rates were obtained by applying the CRUSADE13 and CARDIOCHUS14 scales to the REGICOR registry patients from 2003-2009 (Table 2 of the supplementary material). The percentage of hospitalized patients was obtained from the REGICOR registry.1
The prevalence of PEGASUS characteristics in stable AMI patients ≥ 50 years old (Tables 3 and 4 of the supplementary material) was obtained using REGICOR AMI patient admission data, excluding patients who died or had a subsequent AMI during the first year after the index AMI. It was assumed that prevalence did not change substantially in the first year post-AMI.
Exact 95% confidence intervals (95%CI) for incidence rates and population estimates were obtained using an exact method by assuming a Poisson distribution.
In the prognosis analysis, we first described the patients in the PEGASUS and the non-PEGASUS groups. The incidence of the defined outcomes was assessed at 1-year and at a median of 4.7 years of follow-up, after 1 year of stable disease, by Kaplan-Meier. Sensitivity analyses for the incidence of the assessed outcomes were performed by competing risk-adjusted survival analysis (Table 5 of the supplementary material).15 Excess risk in PEGASUS patients was analyzed at the defined time points using Cox proportional hazards regression models. The proportional hazard assumption of the PEGASUS characteristic was confirmed graphically, by the noncrossing of the survival curves by PEGASUS category, and statistically, by the nonsignificance of the nonzero slope test. Adjustment variables in the models were selected if significantly associated with the outcome and with the PEGASUS variable in bivariate analyses (P<.05). To prevent multicollinearity, the following variables were excluded from the models: PEGASUS characteristics (diabetes, previous AMI and CKD) if the PEGASUS variable was included; thrombolysis and percutaneous coronary intervention if reperfusion was included; left ventricular ejection fraction if maximum Killip class was included; and in-hospital medication if discharge medication was included, the latter was preferred as a proxy of follow-up medication. The C-statistics of the Cox models for the 4.7 years of median follow-up are shown in Table 6 of the supplementary material. Fully adjusted incidence was represented graphically by group (PEGASUS and non-PEGASUS). Predictors of outcome occurrence during the whole follow-up in stable PEGASUS patients were examined using Cox proportional hazard regression models. To account for the effect of not including multivessel CHD in the PEGASUS definition, we conducted a sensitivity analysis using the variable when available (Table 7 of the supplementary material).
Statistical analyses were performed using R software version 3.2.1.16
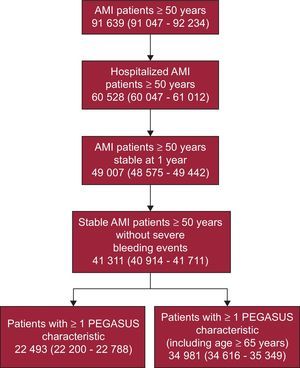
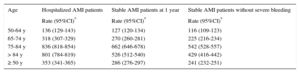
RESULTSYearly Number of Stable Acute Myocardial Infarction Patients With PEGASUS CharacteristicsIt was estimated that the incidence of AMI, hospitalized AMI, stable AMI at 1 year, and of stable AMI without severe bleeding at 1 year was 534, 353, 286 and 241/100 000 inhabitants in individuals ≥ 50 years old (Table 1). These figures yielded an estimation of 91 639 incident AMI cases in individuals ≥ 50 years old in Spain in 2014. Of these, 60 528 were hospitalized, 49 007 were alive and stable at 1-year, and 41 311 had no severe bleeding events during the first year post-AMI (Figure 1, Table 8 of the supplementary material).
Estimated Incident Rate of Acute Myocardial Infarction in Patients ≥ 50 years old, Stable and Without Bleeding Events at 1-year Follow-up, in Spain in 2014
| Age | Hospitalized AMI patients | Stable AMI patients at 1 year | Stable AMI patients without severe bleeding |
|---|---|---|---|
| Rate (95%CI)* | Rate (95%CI)* | Rate (95%CI)* | |
| 50-64 y | 136 (129-143) | 127 (120-134) | 116 (109-123) |
| 65-74 y | 318 (307-329) | 270 (260-281) | 225 (216-234) |
| 75-84 y | 836 (818-854) | 662 (646-678) | 542 (528-557) |
| > 84 y | 801 (784-819) | 526 (512-540) | 429 (416-442) |
| ≥ 50 y | 353 (341-365) | 286 (276-297) | 241 (232-251) |
95%CI, 95% confidence interval; AMI, acute myocardial infarction.
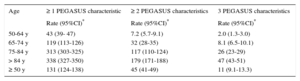
PEGASUS characteristics (diabetes, previous AMI, and CKD) were highly prevalent in AMI patients ≥ 50 years old who did not have another AMI or died during the first year after the index AMI (Table 3 of the supplementary material). Diabetes was the most prevalent characteristic in both men and women (28.9% and 40.4%, respectively). The estimated annual incidence of stable AMI without severe bleeding at 1 year, and at least 1 PEGASUS characteristic was 131/100 000 inhabitants in individuals ≥ 50 years old (Table 2). If age ≥ 65 years was taken into account, the incidence increased to 204/100 000 inhabitants in this population. These figures translated into an annual number of stable AMI patients with at least 1 PEGASUS characteristic of 22 493 and 34 981, respectively (Figure 1, Table 9 of the supplementary material).
Estimated Incident Rate of Acute Myocardial Infarction in Patients ≥ 50 Years Old, by Number of PEGASUS Criteria, in Spain in 2014
| Age | ≥ 1 PEGASUS characteristic | ≥ 2 PEGASUS characteristics | 3 PEGASUS characteristics |
|---|---|---|---|
| Rate (95%CI)* | Rate (95%CI)* | Rate (95%CI)* | |
| 50-64 y | 43 (39- 47) | 7.2 (5.7-9.1) | 2.0 (1.3-3.0) |
| 65-74 y | 119 (113-126) | 32 (28-35) | 8.1 (6.5-10.1) |
| 75-84 y | 313 (303-325) | 117 (110-124) | 26 (23-29) |
| > 84 y | 338 (327-350) | 179 (171-188) | 47 (43-51) |
| ≥ 50 y | 131 (124-138) | 45 (41-49) | 11 (9.1-13.3) |
95%CI, 95% confidence interval; AMI, acute myocardial infarction;
PEGASUS criteria: diabetes, previous acute myocardial infarction and chronic disease.
It was also estimated that 191 491 individuals aged ≥ 50 years old who had an AMI within the preceding 3 years were stable in Spain in 2014 (Table 10 of the supplementary material).
Outcome Analysis in PEGASUS PatientsThe REGICOR reference hospital consecutively collected data on 1963 AMI patients aged 35-74 years in 2003-2009. Of these, data on 1391 patients were available for analysis (Figure 2), with a median follow-up of 4.7 years [interquartile range, 3.2-5.7 years] after 1 year of stable disease.
At baseline, patients with at least 1 PEGASUS characteristic (including age ≥ 65 years) had a higher prevalence of hypertension and heart failure than non-PEGASUS patients (Table 3). During hospitalization, PEGASUS patients less frequently underwent reperfusion. In addition, PEGASUS patients more often had post-AMI arrhythmia, a lower left ventricular ejection fraction and a higher Killip class. Both during hospitalization and at discharge, PEGASUS patients were more often prescribed ACE inhibitors/ARB, but less often received beta-blockers and lipid lowering drugs.
Characteristics of the 1391 Consecutive Acute Myocardial Infarction Patients Included, Aged 50-74 Years, by the Presence of at Least 1 PEGASUS Characteristic (age>64 years, diabetes, previous Acute Myocardial Infarction or Chronic Kidney Disease)
| Non-PEGASUS (n=465) | PEGASUS (n=926) | P | |
|---|---|---|---|
| Age, y | 56.7±4.3 | 66.2±6.5 | <.001 |
| Female gender | 76 (16.3) | 213 (23.0) | .005 |
| Hypertension | 243 (53.2) | 635 (70.1) | <.001 |
| Hypercholesterolemia | 252 (56.8) | 518 (60.0) | .281 |
| Smoking (current) | 273 (59.7) | 274 (30.4) | <.001 |
| History of angina | 156 (34.3) | 350 (39.6) | .064 |
| Heart failure | 70 (15.8) | 211 (24.9) | <.001 |
| During hospitalization | |||
| ST-segment elevation | 279 (60.7) | 463 (51.4) | <.001 |
| Angiography | 384 (83.7) | 746 (80.9) | .240 |
| Reperfusion | 348 (75.0) | 537 (58.5) | <.001 |
| Thrombolysis | 149 (32.0) | 204 (22.1) | <.001 |
| PCI | 285 (61.6) | 438 (47.7) | <.001 |
| Arrhythmia (VT, VF) | 71 (15.5) | 181 (20.1) | .046 |
| Angina | 41 (9.0) | 100 (11.1) | .271 |
| LVEF<50% | 104 (25.0) | 235 (31.6) | .013 |
| III-IV highest Killip class | 19 (4.1) | 74 (8.1) | .008 |
| ACE inhibitors/ARB | 353 (76.7) | 784 (86.6) | <.001 |
| Beta-blocker | 436 (94.8) | 758 (83.0) | <.001 |
| Lipid lowering drugs | 432 (93.5) | 794 (88.3) | .003 |
| Antiplatelet treatment | 456 (99.8) | 910 (99.7) | .999 |
| 4-drug combination | 310 (68.4) | 581 (65.3) | .274 |
| At discharge | |||
| ACE inhibitors/ARB | 267 (58.3) | 678 (74.8) | <.001 |
| Beta-blocker | 392 (85.2) | 668 (73.2) | <.001 |
| Lipid lowering drugs | 418 (90.7) | 728 (81.0) | <.001 |
| Antiplatelet treatment | 455 (99.3) | 871 (97.9) | .071 |
| 4-drug combination | 217 (47.3) | 427 (47.4) | .999 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; CKD, chronic kidney disease; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention; VF, ventricular fibrillation; VT, ventricular tachycardia.
Data are expressed as No. (%) or mean±standard deviation.
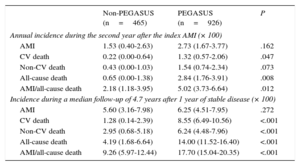
At 1 year of follow-up after 1 year of stable disease, PEGASUS patients had a higher incidence of all-cause death than non-PEGASUS patients. At a median of 4.7 years of follow-up, the incidence of all outcomes, except for AMI, was higher in PEGASUS patients (Table 4). A competing risk analysis of outcome incidence showed similar results (Table 5 of the supplementary material). At 3 years of follow-up, the crude incidence of all outcomes, except for AMI, was higher in PEGASUS patients (Table 11 of the supplementary material). At a median of 3.1 years of follow-up, there was no difference in crude self-reported incidence of stroke (1.1% vs 1.4%, in 174 non-PEGASUS and 446 PEGASUS patients, respectively).
Incidence of Events in Stable Acute Myocardial Infarction Patients With and Without PEGASUS Criteria Obtained by Survival Analysis
| Non-PEGASUS (n=465) | PEGASUS (n=926) | P | |
|---|---|---|---|
| Annual incidence during the second year after the index AMI (× 100) | |||
| AMI | 1.53 (0.40-2.63) | 2.73 (1.67-3.77) | .162 |
| CV death | 0.22 (0.00-0.64) | 1.32 (0.57-2.06) | .047 |
| Non-CV death | 0.43 (0.00-1.03) | 1.54 (0.74-2.34) | .073 |
| All-cause death | 0.65 (0.00-1.38) | 2.84 (1.76-3.91) | .008 |
| AMI/all-cause death | 2.18 (1.18-3.95) | 5.02 (3.73-6.64) | .012 |
| Incidence during a median follow-up of 4.7 years after 1 year of stable disease (× 100) | |||
| AMI | 5.60 (3.16-7.98) | 6.25 (4.51-7.95) | .272 |
| CV death | 1.28 (0.14-2.39) | 8.55 (6.49-10.56) | <.001 |
| Non-CV death | 2.95 (0.68-5.18) | 6.24 (4.48-7.96) | <.001 |
| All-cause death | 4.19 (1.68-6.64) | 14.00 (11.52-16.40) | <.001 |
| AMI/all-cause death | 9.26 (5.97-12.44) | 17.70 (15.04-20.35) | <.001 |
AMI, acute myocardial infarction; CV, cardiovascular
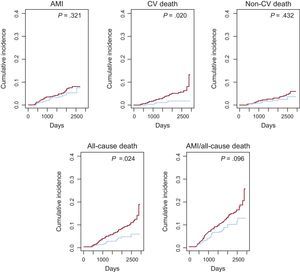
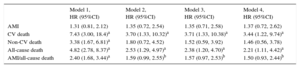
At 1 year of follow-up, stable PEGASUS patients had a higher risk of all-cause death (hazard ratio [HR]=4.4, 95%CI, 1.3-14.6) and of AMI/all-cause death (HR=2.34; 95%CI, 1.2-4.6), but only in unadjusted analysis (Table 12 of the supplementary material). At a median 4.7 years of follow-up, unadjusted HR showed that PEGASUS patients had a higher risk of death (cardiovascular, non-cardiovascular and all-cause) and of having an AMI/all-cause death than non-PEGASUS patients (Table 5). After adjustment for demographic and clinical history variables, cardiovascular and all-cause death remained significantly higher in PEGASUS patients (HR=3.7 and 2.5; 95%CI, 1.3-10.3 and 1.3-5.0, respectively). Further adjustment with discharge medication did not explain the higher risk of cardiovascular and all-cause death observed in PEGASUS patients (Table 5 and Figure 3). In the sensitivity analysis including multivessel CHD in the PEGASUS definition, results at 4.7 years of follow-up were similar although the effects diminished (Table 7 of the supplementary material).
Hazard Ratio of Outcomes During a Median of 4.7 Years of Follow-up for Stable PEGASUS Acute Myocardial Infarction Patients
| Model 1, HR (95%CI) | Model 2, HR (95%CI) | Model 3, HR (95%CI) | Model 4, HR (95%CI) | |
|---|---|---|---|---|
| AMI | 1.31 (0.81, 2.12) | 1.35 (0.72, 2.54) | 1.35 (0.71, 2.58) | 1.37 (0.72, 2.62) |
| CV death | 7.43 (3.00, 18.4)a | 3.70 (1.33, 10.32)a | 3.71 (1.33, 10.38)a | 3.44 (1.22, 9.74)a |
| Non-CV death | 3.38 (1.67, 6.81)a | 1.80 (0.72, 4.52) | 1.52 (0.59, 3.92) | 1.46 (0.56, 3.78) |
| All-cause death | 4.82 (2.78, 8.37)a | 2.53 (1.29, 4.97)a | 2.38 (1.20, 4.70)a | 2.21 (1.11, 4.42)a |
| AMI/all-cause death | 2.40 (1.68, 3.44)a | 1.59 (0.99, 2.55)b | 1.57 (0.97, 2.53)b | 1.50 (0.93, 2.44)b |
95%CI, 95% confidence interval; AMI, acute myocardial infarction; CV, cardiovascular; HR, hazard ratio.
Models: 1, crude hazard ratio; 2, adjusted for age, hypertension, smoking, heart failure; 3, as model 2 plus ST-segment elevation, reperfusion, arrhythmia, maximum Killip class; 4, as model 3 plus beta-blockers and lipid-lowering drugs at discharge.
Incidence of outcomes in stable acute myocardial infarction patients by presence/absence of PEGASUS characteristics. The fully adjusted models presented in Table 5 are represented in this figure. Red and blue lines represent patients with and without any PEGASUS characteristic, respectively. AMI, acute myocardial infarction; CV, cardiovascular.
In PEGASUS patients, heart failure was the most significant predictor of cardiovascular and all-cause mortality, previous AMI and hypertension were the most significant predictors of AMI, and nonprescription of beta-blockers at discharge was the most significant predictor of noncardiovascular death (Table 13 of the supplementary material).
DISCUSSIONWe estimated that, in 2014, there were 41 311 AMI patients ≥ 50 years old in Spain who were stable and without bleeding events at 1-year post-AMI. Of these patients, 22 493 (54.4%) had diabetes, previous AMI, or CKD.
Based on the findings of the PEGASUS trial, we would expect that treating these 22 493 patients for 1 year with aspirin and ticagrelor at 60-mg would prevent 106 events (cardiovascular death, AMI, or stroke) and would cause 78 major bleeding events.7 While the number of prevented cardiovascular events is higher than the number of caused bleeding events, the latter include intracranial bleeding, overt signs of hemorrhage, and fatal bleeding. In the PEGASUS trial, patients receiving aspirin+ticagrelor had a significantly higher occurrence of bleeding events requiring transfusion or study-drug discontinuation, but not of fatal bleeding or intracranial hemorrhage.7 The high ratio of bleeding events caused to cardiovascular events prevented could probably be lowered by carefully considering the treatment of patients at a certain bleeding risk. Thus, estimation of the bleeding risk in these patients is of paramount importance to define their treatment and should be carried out systematically by validated bleeding scores.
In this study, we found that the competing risk-adjusted incidence of AMI/all-cause death in stable AMI patients during the second year after the index AMI was 5%. This incidence is between the 2% and the 9% reported by the CLARIFY registry and a nationwide observational study in Sweden, respectively.17,18 One of the reasons for the incidence difference could be the age of the included patients. On the other hand, while 3-year crude incidence of AMI was almost the same in this study (4.4%) and in the PEGASUS trial (4.2%), compared with the PEGASUS trial, we found a higher incidence of cardiovascular and all-cause death (3.2% vs 2.6% and 6.3% vs 4.0%, respectively). These differences could be due to the higher prevalence of previous AMI and the lower prescription of beta-blockers in our study compared with the PEGASUS trial participants. In addition, a possible higher prevalence of heart failure in the PEGASUS patients of our study could also have had an impact on the higher incidence of cardiovascular and all-cause death.
Our adjusted analysis showed that PEGASUS patients had a higher risk of cardiovascular and all-cause death during follow-up compared with non-PEGASUS patients. In addition to the presence of PEGASUS characteristics, this result could be partially explained by the lower reperfusion, higher Killip class, higher percentage of non—ST-segment elevation AMI and non-classifiable patients, and the higher prevalence of post-AMI arrhythmia in PEGASUS patients. The lower prescription of beta-blockers and lipid-lowering drugs likely contributed to the higher cardiovascular and all-cause death in PEGASUS patients. The presence of more patients with non—ST-segment elevation AMI and nonclassifiable AMI in the PEGASUS group reflects the more complex phenotype and the greater burden of comorbidities in patients with PEGASUS characteristics.19 The higher long-term mortality of patients with non—ST-segment elevation compared with patients with ST-segment elevation20 could partially explain the higher mortality of PEGASUS patients in our study.
Regarding in-hospital management, AMI patients ≥ 50 years old with either diabetes, previous AMI, or CKD received less revascularization and less prescription of guideline-recommended medication (except for ACE inhibitors/ARB) than patients without these characteristics. Part of this differential management is presumably related to the older age of the PEGASUS patients.21 In the present study, cardiovascular and all-cause death risk differences between PEGASUS and non-PEGASUS patients were partially explained by clinical characteristics, in-hospital management, and discharge medication. The persistent differences despite adjustment show the residual risk of these patients even after treatment with evidence-based recommended care. Given these results, the question arises of whether an increase in revascularization and guideline-recommended medication prescription, in addition to DAPT, would decrease even further the occurrence of cardiovascular events in PEGASUS patients.
As for the predictors of the composite AMI/all-cause death at long-term in stable PEGASUS patients, we observed an increased risk for older patients and for those with diabetes, previous AMI, or heart failure. The magnitude of the increased risks was comparable to that described in a nationwide study of stable AMI patients in Sweden.18 In contrast, female sex was not associated with the composite AMI/all-cause death in our study. As for guideline-recommended medication, prescription of beta-blockers at discharge was inversely and independently associated with noncardiovascular and all-cause death and with AMI/all-cause death in stable PEGASUS patients. These results are in line with those of previous studies showing that the use of beta-blockers and statins is associated with a reduced risk of all-cause mortality after AMI.22
The duration of DAPT after acute coronary syndrome has been under debate for the last decade. On the one hand, recent registry studies and clinical trials have shown that premature discontinuation of DAPT (aspirin+clopidogrel / prasugrel) in acute coronary syndrome patients with stent implantation was associated with an increased risk of ischemic events23 and that aspirin+ticagrelor beyond 1 year was associated in AMI patients with a lower risk of cardiovascular events.7 On the other hand, recent randomized studies, with a lower number of patients, have shown that DAPT (aspirin+clopidogrel / ticagrelor / prasugrel) beyond 6 months did not provide additional benefit after stent implantation.24,25 Still, while DAPT beyond 1-year appears to be beneficial in terms of cardiovascular events prevented, at least in AMI patients, the increase in bleeding events calls for further analysis of these patients. In addition, the optimum total length of DAPT has yet to be determined. A recent study from the FAST-MI 2005 Registry has shown that aspirin+clopidogrel for 1 and 2 years had no impact on 5-year mortality,26 highlighting the importance of assessing long-term outcomes in stable AMI patients to define the duration of DAPT.
To our knowledge, this is the first comparison of long-term outcomes in stable AMI patients with and without high-risk characteristics using real-world data. Two studies have previously reported outcomes in this population, the CLARIFY registry17 and a Swedish observational study,18 but these studies did not compare patients with and without high-risk features or analyze long-term outcomes. In addition, this is the first study estimating the population prevalence of these patients.
LimitationsThe estimation of the annual number of AMI patients ≥ 50 years old with PEGASUS characteristics in Spain has certain limitations. First, AMI incidence rates were obtained from IBERICA, carried out in the late 1990s. These estimates, the most recent for Spain, despite being adjusted for clustering and updated by the 2000 AMI definition change, may differ from the real estimates. This limitation highlights the need for updated population estimates of AMI incidence and mortality in Europe. Second, due to data availability, we used the prevalence of PEGASUS characteristics at hospitalization for the index AMI instead of at 1-year post-AMI. However, we would not expect a significant increase in risk factor prevalence during this year. Third, due to the high percentage of missing data on multivessel CHD (60%), we did not include it in the analysis. Based on preliminary data from the REGICOR hospital registry, > 50% of AMI patients had multivessel CHD, and the inclusion of multivessel CHD would increase the number of patients with at least 1 PEGASUS characteristic by 14%. Thus, we would expect an even higher number of stable AMI patients with at least 1 PEGASUS characteristic in Spain.
There are also limitations in the outcome analysis of PEGASUS and non-PEGASUS patients. First, this was an observational study, and potential confounding caused by measured and unmeasured variables may be present. Second, while we included all AMI patients aged 35-74 years from a reference area of approximately 600 000 inhabitants during 2003-2009, the study could not have sufficient power to detect differences in certain outcomes such as AMI. Third, we had no information on prescribed or used medication during the follow-up; thus, we could only include prescribed medication during hospitalization and at discharge. While medication at discharge could be considered as a proxy for follow-up medication, it is affected by the proportion of days covered, which may vary considerably among the included patients. Fourth, we had no information on bleeding events during follow-up, so we could not analyze their incidence. Fifth, we did not include multivessel CHD in the PEGASUS definition due to data completeness. However, the sensitivity analysis including multivessel CHD in the PEGASUS definition, when available, showed similar results in the prognosis analysis but diminished effects. Sixth, while it is possible that changes in the management of AMI patients that have occurred in the last decade could affect the obtained results, the high prescription of evidence-based medication observed in the included patients suggests that the modification would be moderate.
CONCLUSIONSIn 2014, there were 22 493 AMI patients ≥ 50 years old in Spain who had survived 1 year without bleeding events and had at least one PEGASUS characteristic (diabetes, previous AMI or CKD). Stable AMI patients aged 50-74 years with any PEGASUS characteristic had a higher risk of cardiovascular and all-cause death at 4.7 years than those without any PEGASUS characteristics. The increased risk of death of AMI patients with PEGASUS characteristics indicates the need to strengthen secondary prevention and lifestyle modifications and to properly define the required duration of DAPT in these patients.
FUNDINGThe REGICOR AMI Registry was supported by the Instituto de Salud Carlos III-FEDER (grant numbers RD06/0009, RD12/0042, FIS-90/0672, FIS-93/0568, FIS 94/0539, FIS96/0026-01, FIS99/0655, FIS99/0013-01, FIS 99/9342, PI081327, PI11/01801, CP12/03287 [MG], and IFI14/00007 [SSB]), the Catalan Agency for Management of University and Research Grants (grant numbers 2005SGR00577, 2009SGR1195, 2014SGR240), Fundació La Marató TV3 (grant number ID#081630) and Agència d’Informació, Avaluació i Qualitat en Salut (grant number AATRM 034/33/02). I.R. Dégano was funded by the RECERCAIXA Program, Obra Social “La Caixa” (grant number RE087465).
CONFLICTS OF INTERESTJ. Marrugat reports grants, consultancy fees, or honoraria from AstraZeneca, Sanofi, Shire, Gilead, Daichii-Sankyo, Gendiag and Ferrer.
The authors are grateful to Susanna Tello, Marta Cabañero, Leny Franco, and Isabel Ramió for project and data management. We also appreciate the revision of the English text by Elaine Lilly, PhD, of Writer's First Aid.